Introduction
Ectopic pregnancy is the most common cause of pregnancy related deaths in the first trimester of pregnancy. It accounts for 6-10% of all pregnancy related deaths. As per the Confidential Enquiry into Maternal and Child Health (CEMACH) Report, the number of deaths attributed to ectopic pregnancy has increased from 47 in 2002-2004 to 75 in 2008-2010 triennium [1]. Whereas in past, most of the patients with ectopic pregnancy presented with acute symptoms and intra-abdominal hemorrhage which meant resorting to immediate surgery, the scenario is much different in recent times. Advances in laboratory and imaging technologies in last few decades allow an early diagnosis of ectopic pregnancy, many times even before the patient develops any symptoms. Consequently, in many such patients surgery is not always necessary. Expectant and medical management are feasible options in properly selected cases.
Conservative management of unruptured ectopic pregnancy using single dose methotrexate (MTX) with the aim of conserving the tube was first described by Stovall et al., [2]. Studies have been conducted in past to show MTX being comparable in efficacy to laparoscopic salpingostomy [3,4]. However, careful selection of cases for medical management is important. There are some cases which resolve with single dose of MTX but there are some who require an additional dose. There are some cases in which tubal rupture occurs after MTX, risk of this being quoted as ranging from 7% to 14% [5-12] and then there are cases who fail to respond to either a single or repeated dose of MTX and need surgical intervention.
Since this modality of management of ectopic pregnancy has only recently been started in Mafraq Hospital, Abu Dhabi, United Arab Emirates (UAE), this study was conducted to evaluate its efficacy and various factors which may have influence on the success rate.
Objective
In the present study, we evaluated the efficacy of medical management of selected cases of ectopic pregnancy with injection MTX and the factors influencing the success of medical management.
Materials and Methods
This is an observational retrospective study which included patients who attended Mafraq Hospital in the Department of Obstetrics and Gynecology between August 2008 and December 2011 and were diagnosed to have ectopic pregnancy. Diagnosis of ectopic pregnancy was made by single/serial serum Beta Human Chorionic Gonadotrophin (Beta HCG) estimation combined with transvaginal sonography and/or clinical presentation.
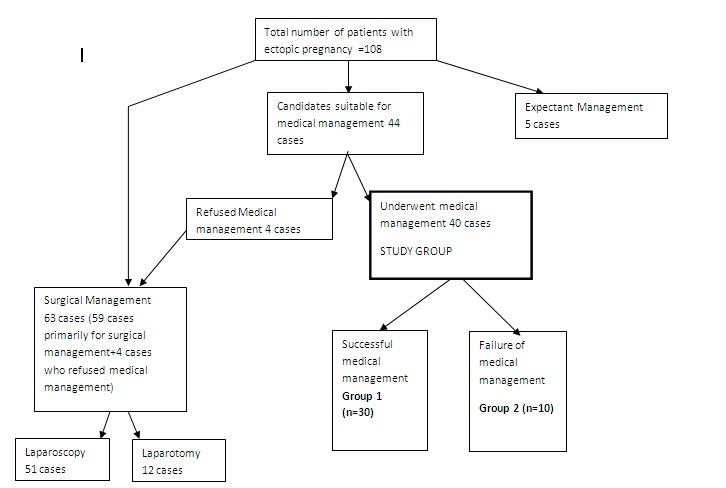
There were 108 cases of ectopic pregnancy which were admitted during the study period. Five of these were managed expectantly. Of the remaining lot of 103, women with contraindications to MTX (i.e. leucopenia, thrombocytopenia, or elevated serum liver enzymes or creatinine) were excluded. Sixty three cases (59 cases that were primarily for surgical management plus 4 cases that refused medical management) underwent surgical management. Of these, 51/63 were managed by laparoscopic approach and remaining 12/63 managed by laparotomy. One out of these 12 cases managed by laparotomy was cervical pregnancy and she underwent total hysterectomy.
In all, 44 cases fulfilled the study inclusion criteria for medical management with injection methotrexate.
The inclusion criteria for medical management were as follows:
- Hemodynamic stability
- Adnexal mass ≤ 4 cm
- Absent cardiac activity
- Hemoperitoneum <100 ml
- Pregnancy of unknown location (PUL)
Four out of these 44 cases who met the inclusion criteria declined medical management and opted for surgery as the primary mode of management. Finally 40 women were available for evaluation and they constituted the “study group”. [Table/Fig-1] shows the flow of participants included in the study.
Baseline investigations in the form of complete blood count, blood group and rhesus type, renal and liver function tests were done apart from serum Beta HCG at the beginning of the medical treatment. All the patients in the study group were informed about possible side effects of MTX, possibility of tubal rupture and intra-abdominal hemorrhage necessitating surgical intervention, protocol for serum Beta HCG monitoring, possibility of needing additional doses of MTX and possibility of failure of medical management. Written informed consent was obtained from all the cases in the study group.
All the patients in the study group were treated medically with a single intramuscular injection of MTX in a dose of 50 mg/m2. The day when the first dose of injection was given was considered as day 1. Beta HCG levels in serum were measured on day 4 and day 7 after giving the injection. A subsequent dose of intramuscular MTX 50 mg/m2 was given to patients whose serum Beta HCG levels did not decline by at least 15% between day 4 and day 7 after receiving a dose of injection MTX. A subsequent dose of MTX was also given in patients whose Beta HCG levels showed plateau or increased during the follow up. As per the departmental protocol, maximum number of MTX doses given was 2 except one patient who received 3 doses. She was hemodynamically stable and refused surgical intervention for rising Beta HCG levels even after 2 doses but ultimately was operated on 15th day as her Beta HCG levels continued to plateau. Eventually 28/40(75%) received a single dose, 11/40 (22.50%) received 2 doses and 1/40 (2.5%) received 3 doses of MTX. All the patients irrespective of the number of doses of injection MTX received were then followed up with weekly measurement of serum Beta HCG until it reached a normal value of <5mIU/ml.
Non sensitized Rhesus negative patients were given anti-D immunoglobulin for prophylaxis as per the protocol. All the patients who received MTX were advised to use contraception and not to conceive within the next three months after MTX treatment.
Successful response to methotrexate was defined as the decline in Beta HCG level to <5 mIU/ml with one or more doses of MTX and without a need for surgery. These cases formed Group 1 (n=30).
Patients who required surgical intervention after receiving MTX for the reasons of hemodynamic instability or signs of tubal rupture were considered as medical treatment failures. These cases formed Group 2 (n=10).
The patient demographic data (e.g. age and parity), presence or absence of free fluid in the pelvis, size of the adnexal mass, period of amenorrhoea, pretreatment Beta HCG, and post-treatment Beta HCG follow up pattern between day 1 and day 4 were compared between the success group and the failure group. In univariate analysis frequency distributions were generated for each variable separately.
Categorical variables were summarized in percentages and continuous variables in terms of mean and standard deviation. In bivariate analyses, differences in percentages between the comparison groups were tested by Chi-square test and the differences in means were tested by t-test. Crude estimates of Odds ratio (OR) were also calculated to quantify association between an exposure and an outcome i.e. success.
In multivariate analyses, unconditional, multiple logistic regression models were used to obtain estimates of ORs accounting for the role of confounders. E.g. age, parity. Receiver Operative Characteristic Curve (ROC) analysis and tests for diagnostic accuracy (e.g. sensitivity, specificity, positive predictive value, and negative predictive value) were also performed. Significance was determined as p< 0.05.Statistical analyses were carried out in STATA software version 10.1, 2009, and Epi Info version 7.1.0.6, 2012.
Flow chart showing inclusion and exclusion of patients in the study cohort and the treatment outcomes
Characteristics of subjects in study groups a = mean ±Standard deviation (SD) b = No. (%)*= significant, p <0.05
| Characteristics | Group 1 (n=30) | Group 2 (n=10) |
| Agea ( years) | 29.06 ± 5.27 | 28.70 ± 6.01 |
| Amenorrhoeaa Weeks* | 4.33 ± 0.79 | 5.45 ± 1.01 |
| Adnexal mass sizea (Cms) | 1.79 ± 0.98 | 3.46 ± 0.34 |
| Presence of free luidb | 11(36.67) | 8(80) |
Beta HCG levels in success and failure groups on day1, day4 and day 7 and corresponding changes
| Characteristics | Group 1 (n=30) | Group 2 (n=10) | p-value |
| Beta HCG levelsa mIU/ml |
| Day 1 | 3152.6+/-2287.5 | 13327.8+/-5956.9 | 0.0001 |
| Day 4 | 3296.5+/-2688.2 | 15669.6+/-5939.6 | 0.0001 |
| Day 7 | 2139.6+/-3530.7 | 15087.2+/-7908.1 | 0.0001 |
| Day 1-4 | 14.3+/-14.2 | 21.1+/-12.3 | 0.1844 |
| Day 4-7 | 65.6+/-34.9 | 22.7+/-8.5 | 0.0005 |
| Day 1-7 | 69.5+/-31.0 | 54.5+/-17.0 | 0.1551 |
Changes in Beta HCG levelsa % a = mean ± standard deviation
Success rates according to day 1 Beta HCG ranges
| Serum Beta HCG concentration mIU/ml | Group 1 ( n=30) | Group 2 (n=10) | Success Rate in study group (95%CI) |
| <1000 | 6 | 0 | 100.00% |
| 1000-1999 | 4 | 0 | 100.00% |
| 2000-4999 | 18 | 0 | 100.00% |
| 5000-9999 | 1 | 4 | 20.0 (6.3 -80.6)% |
| 10000-14999 | 1 | 1 | 50.0 (1.3-98.7)% |
| 15000 or more | 0 | 5 | 0.0% |
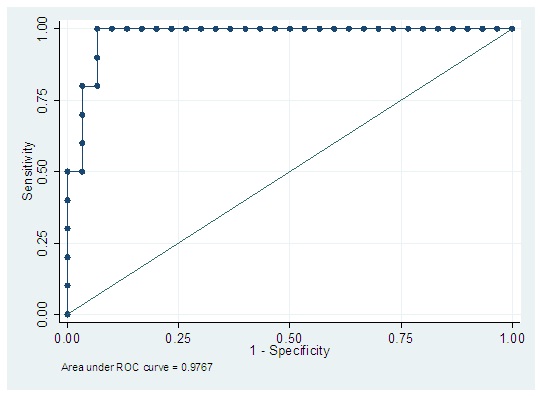
Receiver Operating Characteristic (ROC) Curve for Day 1 Beta HCG levels
Sensitivity =100%, Specificity =93.33%, Percentage correctly classified =95%
Falling trend of Beta HCG from day 1-4 and its effect on success of the treatment
| Trend | Group 1 (n=30) | Group 2 (n=10) | p value |
| Falling Beta HCG day 1-4 | 8 | 0 | 8 |
| Rising Beta HCG day 1-4 | 22 | 10 | 32 |
| Total | 30 | 10 | 40 |
Sensitivity =26.66%, Specificity =100%, PPV =100%, NPV =31.25% and percentage correctly classified =45%
Validity measures for significant predictors of success along with likelihood of success (OR) and statistical significance (p-value)
| Group 1 | Group 2 | Sensitivity | Specificity | PPV | NPV | P Value |
| Free fluid | | | 63.33% | 80% | 90.47% | 42.10% | 0.0175 |
| No | 19 | 2 |
| Yes | 11 | 8 | | | | | |
| Adnexal mass |
| <3 cms | 29 | 1 | 96.66% | 90% | 96.66% | 90% | 0.0001 |
| >3cms | 1 | 9 |
| Amenorrhoea |
| <6 weeks | 29 | 1 | 96.66% | 90% | 96.66% | 90% | 0.0001 |
| >6 weeks | 1 | 9 |
Results
The characteristics of 40 women with ectopic pregnancy who received medical management are presented in [Table/Fig-2].Thirty women were successfully treated with one or more doses of MTX whereas 10 women had failure of medical treatment. The women in success and in failure group did not differ significantly in terms of age and parity. However, mean adnexal mass size, duration of amenorrhoea and the number of cases with presence of free fluid in the pelvis were lower in the successfully treated group [Table/Fig-2].
Baseline Beta HCG levels at the time of initiation of medical management with injection MTX (Day1) were 3152.6± 2287.5 mIU/ml (Mean±SD) in success group and 13327.8±5956.9 mIU/ml in failure group and these levels in two groups were significantly different (p =0.0001). Characteristics of Beta HCG levels on day 1, day 4 and day 7 between success and failure groups are shown in [Table/Fig-3].
The success rates according to the initial (day1) serum Beta HCG concentrations are shown in [Table/Fig-4]. It is evident that success rate went down with increasing level of day 1 serum Beta HCG concentrations. However, a specific cut off for identifying maximum success rate from these levels is desirable and that was done with Receiver Operating Curve (ROC) analysis.
ROC analyses for day 1 Beta HCG levels [Table/Fig-5] revealed that the optimum cut off point for Beta HCG level was 5921 mIU/ml (Area under ROC curve =0.976; sensitivity= 100%; specificity =93.33%, percentage correctly classified =95%). All of these parameters are suggestive of good predictive accuracy of this cut-off. For clinical practice a rounded cut off value of <6000 mIU/ml of day 1 (pretreatment) Beta HCG can be considered as a good predictor of success of medical management with MTX.
Detailed sensitivity, specificity, positive and negative predictive values of the tests were also calculated to evaluate if fall in Beta HCG between day 1 and day 4 was a significant factor in predicting the success of medical management with MTX [Table/Fig-6].
Trend of changes in Beta HCG levels between day 1 and day 4 were also analysed: 8/40 (i.e. 20%) women showed a falling serum Beta HCG level. All of these eight women had successful treatment with a single dose of MTX thus giving it a positive predictive value (PPV) of 100%. Of the remaining 32/40 women showing a rising Beta HCG between day 1-4, 22/32 (68.75%) had successful medical management thus the negative predictive value was 31.25%.
Falling serum Beta HCG between day 1-4 had very well predicted success of MTX therapy (irrespective of number of doses of MTX) [Table/Fig-6] .
Sensitivity, Specificity, Positive Predictive Value and Negative Predictive Value were also estimated to determine the acceptable cut off for adnexal mass size and duration of amenorrhoea in weeks. This analysis revealed that adnexal mass size ≤3 cms and duration of amenorrhoea <6 weeks are good predictors of success of medical management as shown in [Table/Fig-7].
The success rate of medical management for all those patients with no visible adnexal mass on scan was 100% and resolution was achieved with a single dose of MTX in all of them.
Majority i.e. 22 out of 30 patients (73.3%) in success group received a single dose of MTX while 8 out of 30 (26.66%) patients needed second dose of MTX. Whereas in failure group 6 out of 10 (60%) received a single dose, 3 out of 10(30%) required second dose and 1 out of 10(10%) received 3 doses of MTX before being operated. On an average, subjects in success group required less number of doses (Mean ± SD) as compared to subjects in failure group (1.3 ± 0.4 vs. 1.5 ± 0.7). But this difference was not statistically significant (p=0.2688).
In failed medical treatment cases, indication for surgery was increasing abdominal pain or inappropriate changes in serum Beta HCG levels ( rising or plateauing) after one or more doses of MTX. In the present study medical management with MTX irrespective of the number of doses received was successful in 75% cases (30 out of 40).
No serious side effects of MTX were seen in either group 1 or group 2 including patients who received multiple doses of MTX.
Discussion and Conclusion
Systemic use of MTX has been proven to be successful in the medical management of unruptured ectopic pregnancies. Many studies before have evaluated various predictive factors for success of medical management with MTX. According to a study conducted by Lipscomb et al., [13] in Memphis (n=350) initial level of Beta HCG is the best prognostic factor in predicting the success. They found a 94% success rate when the pretreatment Beta HCG level was < 10,000 mIU/ml and a 75% success rate when the initial level was above 10,000 mIU/ml. They concluded that an initial Beta HCG level above10, 000mIU/ml was a risk factor for MTX treatment failure. 82% women who were successfully treated required only one dose in their study. Various studies after the one by Lipscomb et al., have suggested different cut off levels of pretreatment Beta HCG above which MTX treatment may prove to be less effective. Geum Joon Cho et al., [14] in their study conducted on 126 Korean women concluded that initial Beta HCG level was the only predictor of success for the repeated injections, particularly in the cases with initial Beta HCG < 6000mIU/ml. All women in the study by Geum Joon Cho received multiple injections of MTX. In another study by Stika et al., [15], 50 women of ectopic pregnancy were treated with a single dose of MTX and it was concluded that cases with initial serum Beta HCG level > 5000mIU/ml had a greater probability of requiring either multiple doses of MTX or surgical intervention. However exact increase in such risk was not given by Stika et al., They found a success rate of 84.6% with repeated injections of MTX. In another study by Yoshika Yamashita et al., [16] done on 44 Japanese women it was concluded that a serum Beta HCG level > 5,000 mIU/ml is not necessarily resistant to MTX treatment, and patients with interstitial pregnancy are particularly good candidates for conservative treatment even if initial HCG is > 5,000 IU/ml. However the number of cases with initial Beta HCG >5,000 mIU/ml who were treated with MTX in this study was only 14. In yet another study 44 women treated with a single dose of MTX, an initial Beta HCG level of 15,000mIU/ml was found to have a positive predictive value of 97% and a negative predictive value of 69% for success of medical management with MTX [9]. Tawfiq et al., [17] in their study recommend against MTX use when initial Beta HCG was >4000m IU/ml and they emphasize that presence of vaginal bleeding and pelvic pain are most reliable factors to predict failure of treatment. According to the guideline on management of tubal pregnancy from prestigious Royal College of Obstetricians and Gynaecologists, although medical therapy can be successful at serum HCG concentrations considerably higher than 3000 IU/l, quality-of-life data suggest that MTX is only an attractive option for women with an initial Beta HCG below 3000mIU/ml [18]. It is evident that different studies have suggested different cut-offs for Beta HCG levels which may be due to varying inclusion and exclusion criteria, varying sample sizes, varying number of doses of MTX used and most important factor could be different study populations with geographic, ethnicity and race, environmental and biologic variations.
In this study, we found a cut off level of pretreatment Beta HCG of 6000 mIU/ml to give optimum sensitivity and specificity for using medical management with MTX successfully. The suggested cut-off is same as given by Geum Joon Cho et al., in their study conducted on Korean population.
Nguyen et al., [19] reported that a fall in serum Beta HCG between days 1–4 after MTX injection predicted treatment success with no further intervention in 100% of cases (n=30). Monika Skubisz et al., [20] based on proposition by this study and another small study[21] that a fall in serum Beta HCG between day 1-4 confers earlier prognostic information analysed this parameter in their study conducted on 206 Scottish women between 2006-2011. They verified that a decline in serum Beta HCG between days 1-4 after MTX injection provides an early indication of likelihood of treatment success.
In our study, our observation is similar to the observation made by these two studies. However, the number of cases in our study is small and further studies with larger numbers of subjects may be needed to validate this observation.
Karnchana Srivichai MD et al.,[22]in their study conducted on 106 Thai patients with ectopic pregnancy found that in all of the failed cases adnexal mass size was larger than 3.5 cms in diameter whereas in successful cases mean diameter of adnexal mass was 2.3 ± 0.8 cms. Lipscomb et al., [23] found a success rate of 90% in patients with ectopic mass size between 3.5 and 4 cms and a success rate of 93% in those with masses smaller than 3.5 cms. In our study a success rate of 96.6% with medical management was found when the adnexal mass size was less than 3 cms. Our findings are consistent with Lipscomb GH et al., [13].
Presence of free fluid by many is considered as a contraindication to MTX therapy as it may indicate an ongoing tubal rupture. However ruptured fallopian tube is found on surgery only in about 50 to 62% of women in whom free fluid is found on culdocentesis. In the study by Gary H. Lipscomb et al., they concluded that presence of free fluid confined to the pelvis did not affect the success rate. In our study free fluid < 100 ml was found in 47.5% of cases treated medically with MTX and it was found to be a significant factor in predicting the success or failure of MTX therapy. Success rate was found to be lower in cases in which free fluid was present in the pelvis.
Presence of fetal cardiac activity is considered a relative contraindication for MTX therapy. Most of the studies report an increase in failure rate when fetal cardiac activity was present. However, success rate as high as 88% has also been reported when fetal cardiac activity was present [24]. This factor could not be evaluated in our study as presence of fetal cardiac activity was an exclusion criterion. Other authors have evaluated peritrophoblastic doppler blood flow to predict failure and have recommended using doppler along with other parameters to constitute a predictive score grading system [24]. However, evaluation of peritrophoblastic doppler study was not possible in our study as it is not a routine practice of sonologists to perform Doppler study for ectopic pregnancy
Embryonic sac size has also been found to be an important variable in some studies. Mamdoh Eskandar et al., in their study found the optimum cut off for sac size to be 3.4 cms. This factor could not be evaluated in our study as separate measurement of sac size was not available in many patients.
Results of this study indicate that pretreatment Beta HCG level of <6000 mIU/ml, adnexal mass size <3 cms, amenorrhoea < 6 weeks and absence of free fluid in the pelvis are predictors of a successful treatment with MTX. In properly selected cases medical management of ectopic pregnancy with MTX is highly effective and can be considered a forward step taken towards conservation of fallopian tubes especially in countries like UAE where there is inclination towards large family size based on religious and cultural background. At the same time importance of careful clinical vigilance and monitoring cannot be underestimated since the ectopic pregnancy still remains at the risk of rupture even when the patient is on medical management. It is important to note that in failure group in this study 4 out of 6 cases that were operated for increased abdominal pain were eventually not found to have rupture of ectopic pregnancy during surgery. These cases may not truly represent failure as they were found to be operated too soon. In such cases decision to offer surgical management is confounded by a subjective symptom of pain with a possibility of being faced with a case of ruptured ectopic pregnancy. It is difficult to know if the pain is a resolution pain or because of rupture. Fear of rupture and possible risk of life threatening intraperitoneal hemorrhage associated with it will continue to lead the clinicians to resort to surgery. However, the importance of keeping in mind the fact that after giving MTX, patient may complain of abdominal pain even when the pregnancy is unruptured and resolving cannot be underestimated. This pain is usually attributed to separation of degenerating trophoblastic tissue [25].
Changes in Beta HCG levelsa % a = mean ± standard deviation
Sensitivity =26.66%, Specificity =100%, PPV =100%, NPV =31.25% and percentage correctly classified =45%
[1]. Confidential Enquiry into Maternal and Child Health RCOG, UK 2008-2010 [Google Scholar]
[2]. TG Stovall, FW Ling, LA Gray, Single-dose methotrexate for treatment of ectopic pregnancy.Obstet Gynecol. 1991 77(5):754-57. [Google Scholar]
[3]. PJ Hajenius, S Engelsbel, BW Mol, F Van Der Veen, WM Ankum, PMM Bossuyt, Systemic Methotrexate versus laparoscopic salpingostomy in tubal pregnancy: a randomized clinical trial.Lancet. 1997 350:774-79. [Google Scholar]
[4]. G Dias Pereira, PJ Hajenius, BWJ Mol, WM Ankum, DJ Hefferren, PMM Bossuyt, Fertility outcome aftersystemic methotrexate and laparoscopic salpingostomyfor tubal pregnancy.Lancet. 1999 353:724-25. [Google Scholar]
[5]. JL Glock, JV Johnson, JR Brumsted, Efficacy and safetyof single-dose systemic methotrexate in the treatment ofectopic pregnancy.Fertil Steril. 1994 62:716-21. [Google Scholar]
[6]. TG Stovall, FW Ling, Single-dose methotrexate: anexpanded clinical trial.Am J Obstet Gynecol. 1993 168:1759-65. [Google Scholar]
[7]. MA Henry, WL Gentry, Single injection of methotrexatefor treatment of ectopic pregnancies. Am J Obstet Gynecol. 1994 171:1584-87. [Google Scholar]
[8]. Z Gross, JJ Rodriguez, BL Stalnaker, Ectopic pregnancy:Nonsurgical, outpatient evaluation and single-dose Methotrexate treatment.J Reprod Med. 1995 40:371-74. [Google Scholar]
[9]. GH Corsan, M Karacan, S Qasim, MK Bohrer, MX Kemmann, E Qasim, Identification of hormonal Parameters for successful systemic singledosemethotrexate therapy in ectopic pregnancy.Hum Reprod. 1995 10:2719-22. [Google Scholar]
[10]. MX Ransom, AJ Garcia, M Bohrer, GH Corsan, E Kemmann, Serum progesterone as a predictor ofmethotrexate success in the treatment of ectopicpregnancy.Obstet Gynecol. 1994 83:1033-37. [Google Scholar]
[11]. D Hidlebaugh, P O’Mara, Clinical and financial analysesof ectopic pregnancy management at a large health plan.J Am AssocGynecolLaparosc. 1997 4:207-13. [Google Scholar]
[12]. LD Thoen, MD Creinin, Medical treatment of ectopicpregnancy with methotrexate.FertilSteril. 1997 68:727-30. [Google Scholar]
[13]. GH Lipscomb, ML McCord, TG Stovall, Predictors of success of methotrexate treatment in women Withtubal ectopic pregnancies.N Engl J Med. 1999 341:1974-78. [Google Scholar]
[14]. Cho Geum Joon, Lee Sang Hoon, Predictors of success of repeated injections of single-dose Methotrexate regimen for tubal ectopic pregnancy.J Korean Med Sci. 2006 21:86-9. [Google Scholar]
[15]. CS Stika, L Anderson, MC Frederickson, Single-dose methotrexate for the treatment of ectopic pregnancy: Northwestern Memorial Hospital three-year experience.Am J Obstet Gynecol. 1996 174:1840-46. [Google Scholar]
[16]. Yamashita Yoshiki, Katoh Sousuke, Yoshida Yoko, Fujiwara Satoe, Kawabe Sachiko, Hayashi Mika, MTX Could Be First-Line Therapy Even in Cases Where hCG Level is Greater than 5,000 IU/ml, Ectopic Pregnancy-Modern Diagnosis and Management, Dr. MichaelKamrava (Ed.), ISBN: 978-953-307-648-5, In Tech, Available from:http://www.intechopen.com/books/ectopicpregnancy-modern-diagnosis-and-management/mtx-could-be-firstlinetherapy-even-in-cases-where-hcg-level-is-greater-than-5-000-iu-ml. [Google Scholar]
[17]. A Tawfiq, AF Agameya, P Claman, Predictors of treatment failure for ectopic pregnancy treated with single-dose methotrexate.Fertil Steril. 2000 74:877-80. [Google Scholar]
[18]. RCOG: The Management of Tubal Pregnancy. Green-top Guidelines. London, UK: RCOG; 2010:10. [Google Scholar]
[19]. Q Nguyen, M Kapitz, K Downes, C Silva, Are early human chorionicgonadotropin levels after Methotrexate therapy a predictor of response in ectopic pregnancy?Am J ObstetGynecol. 2010 202(630):631-35. [Google Scholar]
[20]. Skubisz Monika, Dutton Philip, Duncan William Colin, Using a decline in serum hCG between days 0–4 to predict ectopic pregnancy treatment success after single dose methotrexate retrospective cohort study.BMC Pregnancy and Childbirth. 2013 :13-30. [Google Scholar]
[21]. MM Skubisz, J Li, EM Wallace, S Tong, Decline in Beta hCG levels between days 0 and 4 after a single dose Of methotrexate for ectopic pregnancy predicts treatment success: a retrospective cohort study.BJOG. 2011 118(13):1665-68. [Google Scholar]
[22]. MD Karnchana Srivichai, MD Chumnong Uttavichai, Medical treatment of ectopic pregnancy: A ten-Year review of 106 cases at Maharaj Nakorn Chiang Mai Hospital.J Med Assoc Thai. 2006 89(10):1567-71. [Google Scholar]
[23]. GH Lipscomb, D Bran, ML McCord, JC Portera, FW Ling, Analysis of three hundred fifteen ectopic pregnancies treated with single-dose methotrexate.Am J Obstet Gynecol. 1998 178:1354-58. [Google Scholar]
[24]. J Elito, AP Reichmann, MN Uchiyama, L Camano, Predictive score for the systemic treatment of unruptured ectopic pregnancy with a single dose of methotrexate. IntJ Gynaecol Obstet. 1999 67(2):75-9. [Google Scholar]
[25]. Eskandar Mamdoh, Single dose methotrexate for treatment of ectopic pregnancy: risk factors for treatment failure.Middle East Fertility Society Journal. 2007 12(1):57-62. [Google Scholar]