Visual loss in Takayasu Arteritis – Look Beyond the Eye
Jayanthi Peter1, George Joseph2, Vivek Mathew3, John Victor Peter4
1 Assistant Professor, Department of Ophthalmology, Christian Medical College, Vellore, India.
2 Professor and Head, Department of Cardiology Unit I, Christian Medical College, Vellore, India.
3 Professor, Department of Neurology, Christian Medical College, Vellore, India.
4 Associate Professor, Department of Medicine, Christian Medical College, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayanthi Peter, Schell Eye Hospital, Christian Medical College,Vellore 632004, India. Phone : +91 9994067762, E-mail : peterjohnvictor@yahoo.com.au
Patients with Takayasu arteritis often present with reduced vision related either to the disease per se or due to complications of therapy. We report a patient with Takayasu arteritis who developed acute onset bilateral visual loss 6wks following percutaneous revascularization of occluded aortic arch branches. No ocular cause for the visual loss was evident. The reason for visual loss in this patient was an extraocular cause. Ocular and extraocular causes of visual loss in Takayasu arteritis are discussed.
Ischemia, Takayasu arteritis, Visual loss
Case Report
A 32-year-old woman with history of inflammatory arthritis, presented with transient right focal seizures followed by blurred vision that resolved completely, two months prior to presentation to our hospital. A further short, self-limiting episode occurred two weeks later. On examination both upper limb blood pressures were not recordable. Systemic examination was otherwise normal. Erythrocyte sedimentation rate was 45mm at one hour, C-reactive protein was 10.4mg/L and anti-nuclear antibody was negative. Magnetic resonance angiogram revealed bilateral subclavian and common carotid artery stenosis, consistent with a diagnosis of Type I Takayasu arteritis. She underwent percutaneous transluminal angioplasty with stenting of the right subclavian and right common carotid arteries. She was advised mycophenolate, tapering doses of prednisolone, aspirin, clopidogrel, fenfibrate and atorvastatin and sent for eye examination.
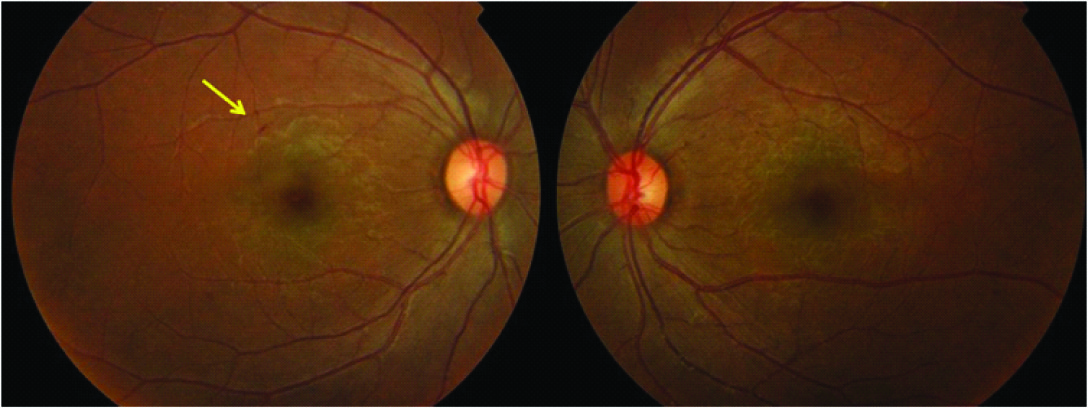
Best corrected visual acuity was 6/6 in both eyes. The anterior segment was normal. Dilated fundus examination revealed few retinal hemorrhages not involving the fovea [Table/Fig-1]. No specific ophthalmic intervention was advised.
Fundus photograph with the arrow pointing to a small hemorrhage in the right eye
She returned two months later with sudden onset visual loss in both eyes associated with multiple episodes of vomiting and reduced sensation in the right side of the body that occurred two weeks earlier. Visual acuity was perception of light in the right eye and hand movements in the left eye. Anterior segment was within normal limits. Pupils were normal and reacting with no relative afferent pupillary defect. Fundus examination was normal in the right eye. A single hemorrhage was seen in the left eye retinal periphery. The absence of significant ocular findings despite severe visual loss and the presence of sensory symptoms suggested a lesion along the visual pathway.
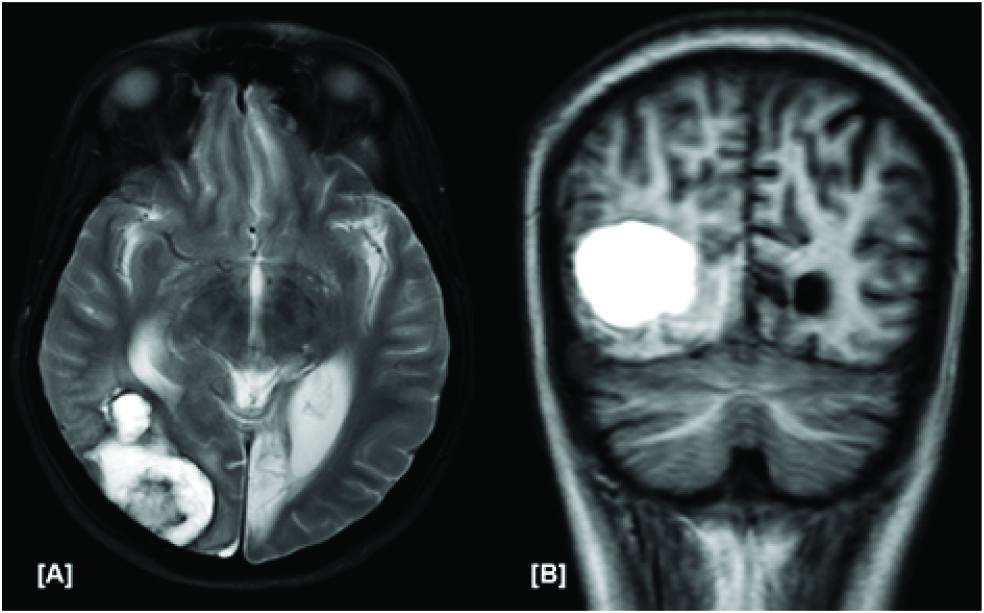
Magnetic resonance imaging (MRI) of the brain showed a large sub-acute occipital bleed on the right side and a chronic occipital infarct on the left side [Table/Fig-2a,b] without mass effect or features of raised intracranial pressure. She was reviewed by the neurosurgeons who advised to stop anti-platelet drugs and start phenytoin. On review 15d later, vision had improved to 4/60 in both eyes. She was subsequently lost to follow up.
Magnetic resonance imaging (MRI) of the brain: [A] T2 weighted axial images of brain showing subacute hemorrhage in the right occipital lobe, and a chronic infarct in the left calcarine cortex; [B] T1 weighted images showing hyperintensity suggestive of subacute hemorrhage
Discussion
The initial presentation with right focal seizures and transient ocular symptoms suggested left cerebral and posterior circulation ischemia respectively as the likely cause for the symptoms. The MRI finding of a chronic infarct of the left occipital cortex may explain the visual symptoms. The subsequent presentation of acute onset blindness of both eyes may be attributed to the new hemorrhage in the right occipital cortex on the background of pre-existing chronic infarct in the left occipital cortex. The ischemic event is likely due to occlusion of the aortic arch branches while the hemorrhage may have been due to antiplatelet therapy or cerebral aneurysms. Angioplasty related artery to artery embolization and re-perfusion injury due to cerebral hyperperfusion was considered as alternative aetiological possibilities. However, these were less likely in view of the long lag-period (6wks) between procedure (angioplasty) and symptom onset.
Reduced vision is common in Takayasu arteritis [1] and may be acute or chronic, transient or permanent, partial or complete or related to the disease per se or due to treatment [Table/Fig-3]. Acute unilateral transient complete loss of vision,termed amaurosis fugax, is due to emboli to the retinal artery. Acute onset of visual symptoms with permanent visual loss may occur with embolic occlusion of the central or branch retinal artery [2,3], venous occlusion [4], anterior ischemic optic neuropathy [5] and vitreous hemorrhage due to bleeding from new vessels in proliferative Takayasu retinopathy. Vascular events (ischemia or hemorrhage) involving the occipital cortex, as in this patient, are extra-ocular causes for acute visual loss.
Causes of visual loss in takayasu arteritis
| Ocular causes |
|---|
| Anterior Segment of the eye | Posterior segment of the eye |
|---|
| Disease related | Neovascular glaucoma (6) Uveitis (7) Cataract Sclerokeratitis (8) | Amaurosis fugax (1) Central or branch retinal artery occlusion (2, 3) Central or branch retinal vein occlusion (4) Anterior ischaemic optic neuropathy (5) Vitreous haemorrhage Ocular ischaemia (1) Macular oedema (1) Exudative retinal detachment (5) |
| Treatment related | Steroid induced Cataract (1) Steroid induced Glaucoma (1) | Glaucomatous optic neuropathy (1) Steroid induced central serous retinopathy |
| Extra-ocular causes |
|---|
| Anterior circulation | Posterior circulation |
|---|
| Disease related | Anterior circulation stroke* | Posterior circulation stroke† |
| Treatment related | Reperfusion injury |
* Anterior circulation stroke may occur due to infarction as a result of occlusion of the aortic arch vessels or as a result of haemorrhage - visual loss as a result of involvement of the optic tract along its pathway; †Visual loss in posterior circulation stroke is due a lesion in the occipital lobe as a result of infarction or haemorrhage
Chronic visual loss in Takayasu arteritis may be due to Takayasu or hypertensive retinopathy [1,5], ocular ischemic syndrome [1], neovascular glaucoma [6], uveitis [7], cataract [1] and sclerokeratitis [8]. Treatment for Takayasu arteritis with disease modifying agents may also result in reduced vision due to complications such as steroid induced cataract, glaucoma and central serous retinopathy [1].
Conclusion
Visual loss is the most common ocular symptom in Takayasu arteritis. Since a variety of causes may result in reduced vision in Takayasu arteritis, a proper history and search for a cause is warranted. In some situations, such as highlighted in this case who had sensory symptoms along with visual loss at the time of presentation, the cause for visual loss was not in the eye per se. A careful history is thus important to ascertain the cause of visual loss in Takayasu arteritis patients to reduce unnecessary investigations and referrals.
* Anterior circulation stroke may occur due to infarction as a result of occlusion of the aortic arch vessels or as a result of haemorrhage - visual loss as a result of involvement of the optic tract along its pathway; †Visual loss in posterior circulation stroke is due a lesion in the occipital lobe as a result of infarction or haemorrhage
[1]. Peter J, David S, Danda D, Peter JV, Horo S, Joseph G, Ocular manifestations of Takayasu arteritis: a cross-sectional studyRetina 2011 31:1170-78. [Google Scholar]
[2]. Peter J, David S, Joseph G, Horo S, Danda D, Peter JV, Rare retinal manifestations in Takayasu arteritisJ Rheumatol 2013 40:1404-05. [Google Scholar]
[3]. Noel N, Butel N, Le Hoang P, Small vessel involvement in Takayasu’s arteritisAutoimmun Rev 2013 12:355-62. [Google Scholar]
[4]. Conrath J, Hadhadj E, Serratrice J, Ridings B, Branch retinal vein occlusion reveals Takayasu’s arteritisJ Fr Ophthalmol 2004 27:162-65. [Google Scholar]
[5]. Peter J, David S, Joseph G, Horo S, Danda D, Hypoperfusive and hypertensive ocular manifestations in Takayasu arteritisClin Ophthalmol 2010 4:1173 [Google Scholar]
[6]. Zhou B, Ye P, Wei S, Preliminary clinical analysis of neovascular glaucoma secondary to carotid artery diseaseClin Exp Optom 2011 94:207-11. [Google Scholar]
[7]. Kausman JY, Walker A, Piper S, Acute panuveitis and Takayasu’s arteritisArch Dis Child 2003 88:938-39. [Google Scholar]
[8]. Arya SK, Nahar R, Narang S, Jain R, Kalra N, Sood S, Sclerokeratitis in Takayasu’s arteritis: a case reportJpn J Ophthalmol 2005 49:548-50. [Google Scholar]