The first few years of life is the most crucial period of life as this age is known for accelerated growth and development, warranting regular monitoring [1]. Any adverse influences during this period may result in severe limitations in their development [2]. It is well recognised that preschool children are nutritionally vulnerable segment of the population, also very susceptible to morbidity due to infections [3]. This age group is most affected by various common and easily treatable illnesses [2]. Prevalence, severity and frequency of morbidity due to infections depend upon infant and young child feeding and caring practices, nutritional status of the child, and environmental hygiene. Effect of morbidity on nutritional status depends upon severity and duration of infection, health care provided, feeding during illness and convalescence [3]. The population characteristics in rural area like socio-cultural variation, low socio economic status, poor health care utilization and over all compromised living condition make the rural children susceptible for various diseases. It is seen that malnutrition is more common in hilly areas than other parts of the country as majority of the children living in rural hilly areas are deprived of proper supply of food. Although, studies have been conducted on health problems among preschool children in India, there are still several localities for which epidemiological information is not available. Keeping in view, an attempt was made to assess the pattern of morbidities in toddlers residing in rural areas of Uttarakhand and to assess the health care utilization by their parents for the same.
Methods
The present cross-sectional study was conducted in children below three years of age from eight villages of Rural Health Training Centre (RHTC), under the administrative control of Department of Preventive and Social Medicine, Himalayan Institute of Medical Sciences Dehradun, India. Duration of the study was from 1st May 2009 to 30th April 2010. A list of households having the study subjects from all the eight villages under RHTC was prepared & a total of 789 under three children were enlisted from these eight villages. The estimated sample size was calculated according to the formula: N=4pq/d2 where p is the prevalence of malnutrition, q=1-p, and d is relative error. Taking malnutrition as a proxy indicator for morbidities,the prevalence of malnutrition in children under three years of age was found to be p=45.9% [4] and relative precision d as 10 % of p, the sample size was calculated to be 468. Considering a no-response rate of 5% it was estimated to be 491 & hence the sample size was rounded off to 500 children.
To conduct this study, a predesigned pretested structured questionnaire was developed and all the questions were framed keeping the study objectives in mind to obtain the necessary information.This questionnaire was tested with a pilot study of 50 mothers of the same area, who had children less than three years of age. The researcher herself interviewed the mothers at the time of pilot testing. The objective of this pilot study was to test the data collection tool’s wording, as well as the clarity of stated questions & hence, reliability of these questions were checked in the pilot study and suitable modifications were made, before finally administering them to respondents.
A door–to–door survey was conducted and households with at least one infant below three years were selected. Taking the inclusion/exclusion criteria into account i.e. infants of multiple births defects, children who were absent for atleast three consecutive visits, parents who did not gave consent, or the child was uncooperative during clinical examination or while taking anthropometry, incomplete questionnaire, families with more than one child, in 0-3 years age group, only the younger child was selected for the present study. Hence, a total of 500 children were covered from these eight villages. Verbal informed consent was obtained from each of the mother and they were reassured that the information obtained will be confidential and used only for the purpose of this study.
An informed consent was taken prior to the interview and mothers were assured of the maintenance of confidentiality of their given information. After ensuring the confidentiality and building a rapport, in depth interview of mothers was undertaken and information regarding child’s age, sex, immunization status etc. was collected. Ages of most of the children were also estimated and cross-checked with reference to the local events such as some important festivals, siblings in the family, horoscopes etc. Information on the occurrence of any illness the child had in the preceding three months was obtained on recall basis. Morbidity Profile was taken keeping in mind the important under five illnesses (diarrhea, URTI, measles), along with history of Pica & worm infestation. The mother’s queries and doubts regarding the same were also answered for ethical reasons. Thereafter, clinical examination was done. Weight was measured using Salter spring balance for children who could not stand and Electronic weighing machine was used for older children. Height was measured without shoes to the nearest 0.1cm using calibrated Stadiometer. For children less than two years of age an Infantometer was used to measure the height. Nutritional status was assessed as per the growth chart developed by WHO using New WHO standards (MGRS 2006), with the help of Anthropometric calculator (Version 2.0.2) [5]. The signs for nutritional deficiencies were also noted in all children. The influence of different child related factors on the morbidity profile of children like immunization and nutritional status were analyzed using appropriate statistical tests. To keep a check on validity of the data, 10% of it was cross checked. Whole process of data collection was monitored by independent observers and supervised by the investigator. The information thus obtained was compiled, tabulated andanalyzed statistically to draw out observationsand meaningful conclusions. Chi-square test was applied as and where found appropriate. For the purpose of the study, morbidity was classified into three categories:
Acute diarrheal disease: defined as at least three watery stools in a 24h period, being considered a new episode if there was a 48h symptom-free interval.
Acute respiratory illness: defined as running nose or cough either with or without fever lasting for at least 72h.
Other morbidities included history of pica, worm infestation etc.
Inclusion criteria: All under-three children including neonates, except those meeting the exclusion criteria were included in the study.
Exclusion criteria: Pre-term newborn, congenital anomalous child and severely ill child were excluded from the study.
Fully Immunized children: An infant who has received BCG; three doses of DPT, OPV and and measles before one year of age.
Results
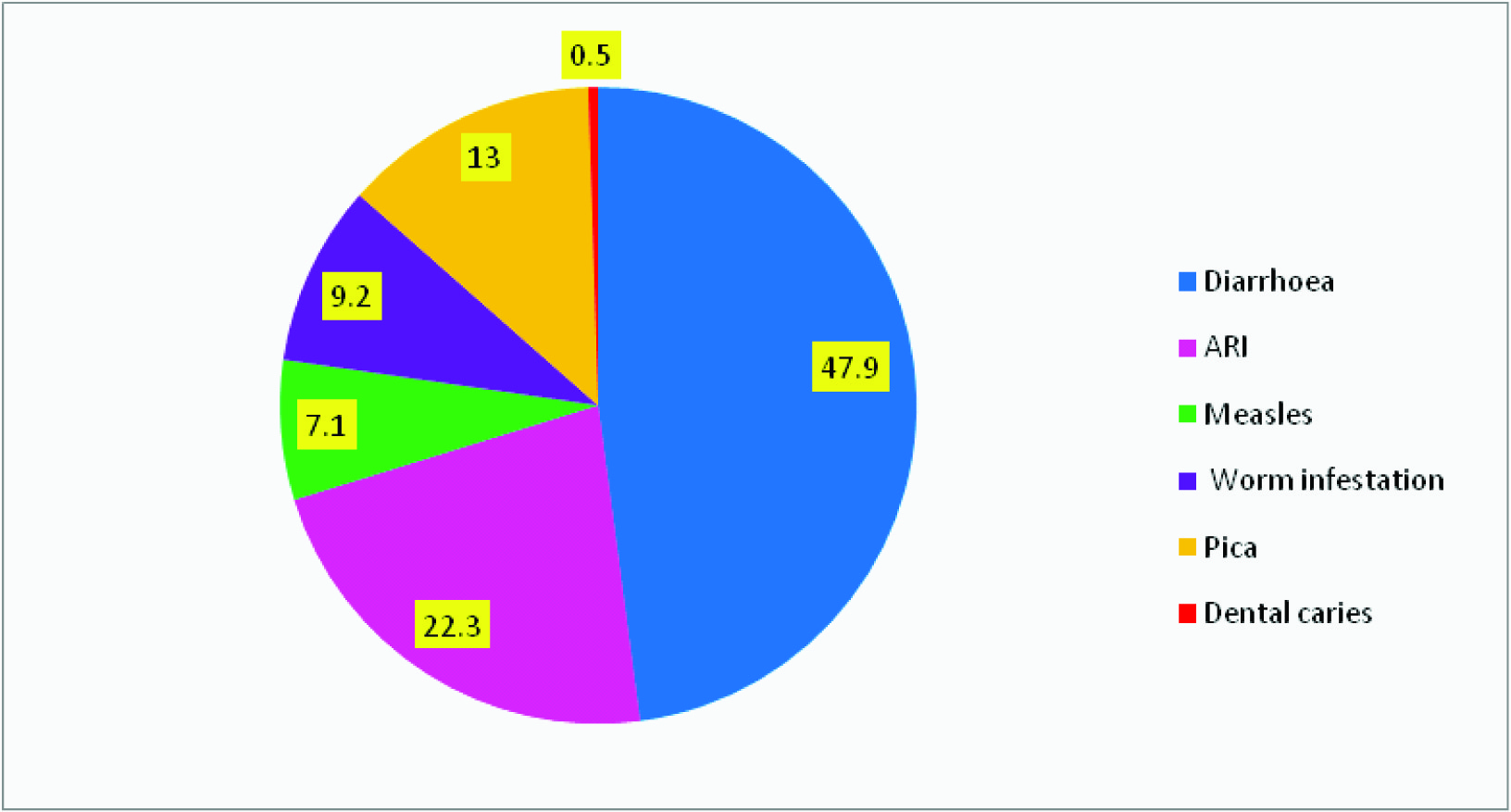
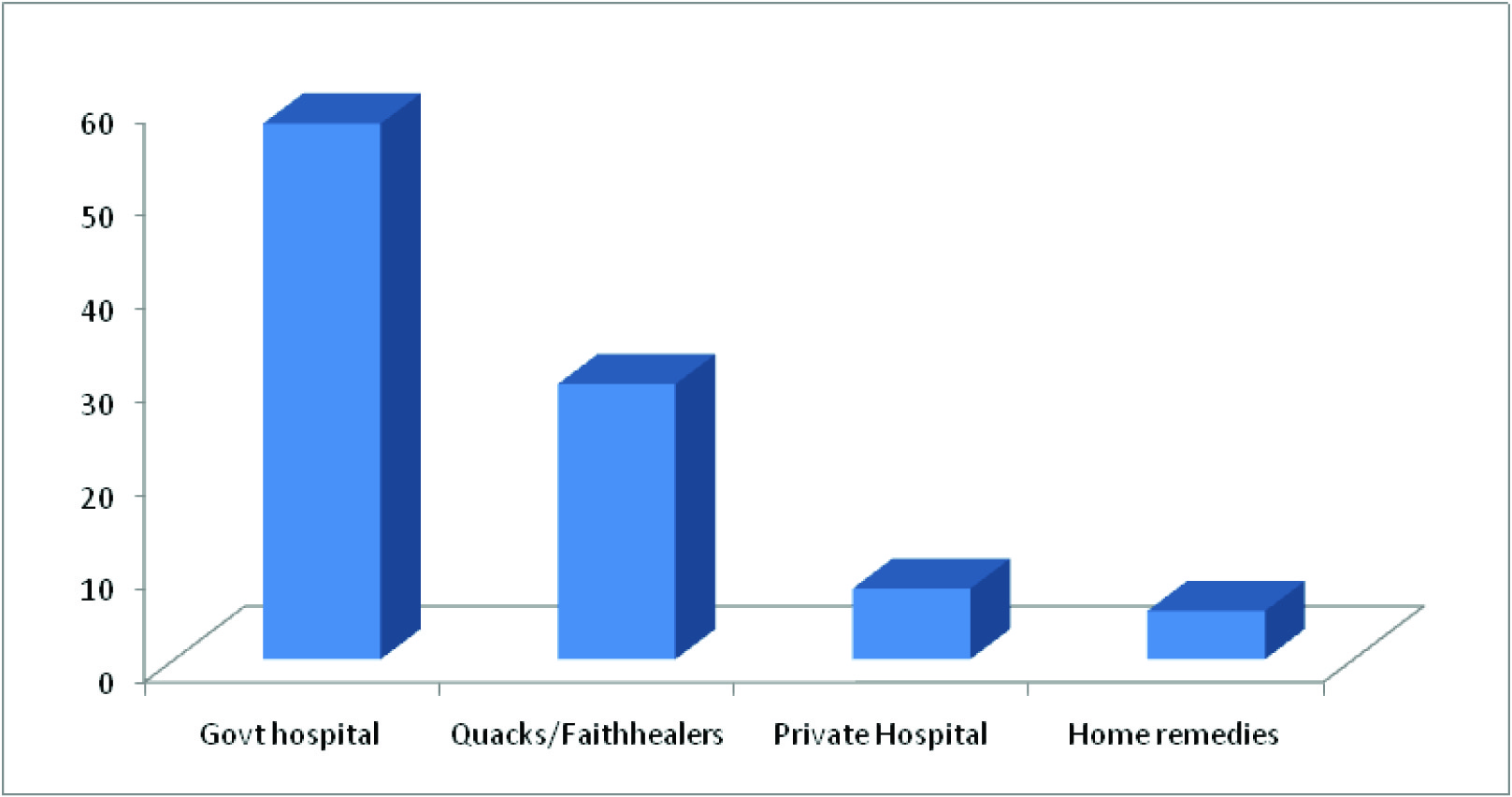
During the study period, a total of 500 under three children were surveyed for the pattern of illnesses. Diarrhea (47.9%) followed by ARI (22.21%), Pica (13%) and Worm Infestation (9.21%) were the commonest morbidities found in the study population [Table/Fig-1]. There were a total of 869 acute spells of sickness & hence, each child suffered with almost 3 illnesses per child. Morbidities were found to be common in males as compared to females [Table/Fig-2]. The overall prevalence of sparse hair was found to be 1.2%, dispigmentation of hair (0.6%), easy pluckability of hair (0.2%) & muscle wasting (0.8%) respectively. Vitamin A deficiency (conjunctival xerosis) was reported at 0.4%, while night blindness and bitot’s spot were not present. Vitamin B complex deficiency, mainly angular stomatitis, cheilosis and glossitis had a higher prevalence (10.8% of glossitis, 6.4% of angular stomatitis and 5.8% of cheilosis) [Table/Fig-3]. 85.6% of the study population was completely immunized and only 22(4.40) of the children did not receive any vaccine. Morbidity was found to be higher (75%) in children who were unimmunized as compared to those who were fully immunized (48.8%) [Table/Fig-4]. Further, it was seen that the preference to seek treatment in the govt. hospitals was higher (57.6%) than other facilities [Table/Fig-5].
Morbidity profile of study subjects
Sexwise morbidity pattern among the study subjects
| Variable | Distribution of children | Total |
|---|
| Male | Female |
|---|
| Diarrhoea** | 215(51.68) | 201(48.32) | 416 |
| ARI** | 108(55.96) | 85(44.04) | 193 |
| Undernourished | 153(51.34) | 145(48.66) | 298 |
| Measles | 32(51.61) | 30(48.39) | 62 |
| History of Worm infestation/ Perianal itching | 43(53.75) | 37(46.25) | 80 |
| History of Pica | 60(53.10) | 53(46.90) | 113 |
| Dental caries | 3(60) | 2(40) | 5 |
| Total | 614 | 553 | 1167 |
*History of Diarrhoea & ARI has been taken for the past 3 months #Multiple responses were obtained
Prevalence of nutritional deficiency signs
| Clinical Signs | No of Children | Frequency |
|---|
| Signs of Protein Energy Malnutrition -14(2.8) |
| a)Sparse hairs | 6 | 1.2 |
| b)Dispigmentation of hair | 3 | 0.6 |
| c)Easy pluckability of hair | 1 | 0.2 |
| d)Muscle wasting | 4 | 0.8 |
| Vitamin A deficiency-2(0.4) | | |
| a)Night Blindness + Bitot’s spots | 2 | 0.4 |
| Vitamin B-Complex deficiency - 115(23.0) |
| a)Angular Stomatitis | 32 | 6.4 |
| b)Cheilosis | 29 | 5.8 |
| c)Glossitis | 54 | 10.8 |
| Rickets-2(0.4) |
| Bowlegs +knock knees | 2 | 0.4 |
| Anaemia | 122 | 24.4 |
Distribution of morbidity on the basis of nutritional status & immunization
| Type of Subject | Total children | Morbidities |
|---|
| Present | Absent |
|---|
| Nutritional status |
| Well Nourished | 202 | 85(42.1) | 117(57.9) |
| UnderNourished | 298 | 178(59.7) | 120(40.3) |
| X2= 14.35 df=1 p= <0.001 |
| Immunization Status |
| Complete | 428 | 219(48.8) | 209(51.2) |
| Partial/Unimmunized | 50 | 54(75) | 18(25) |
| X2= 15.89 df=1 p= <0.001 |
Treatment seeking behavior during Illness
Discussion
Diarrhoeal diseases were number one morbidities in children during 1990s and Acute respiratory infections in 2000s as revealed by different authors whereas in the current study, diarrhea (47.9%) remains as number one morbidity followed by ARI (22.21%), Pica (13%) and Worm Infestation (9.21%) [6]. Our findings are in line with several other authors like Kapil et al., Grover et al., and Panda et al., where diarrhoeal diseases were found to be the major cause of morbidity in the children, whereas our findings lay in contrast with several other studies by Patnaik et al., Biswas T et al., & Raj et al., [6–11]. The prevalence of diarrhea (47%) was comparable to rural villages of South Pakistan (51%) but was much higher as reported previously from West Bengal ( 31.67%) [12–13]. The higher prevalence of diarrhea may be due to the harmful effects of poor hygiene and practice of open-field defecation. Direct comparison of findings between different studies is difficult because of differences in study design, study populations, timing & regional differences.
The mean number of episodes per child per year observed in the present study was higher than the figures of Gulati PV (2.44 episodes per child per year), and Muhe (2.34 episodes per child per year) [14–15]. The mean number of episodes observed is far less than that observed by Gupta KB (10.7 episodes /child/ year) & P Gladstone where a very high morbidity with an average of 11 illnesses each year was reported during the first three years of life [16–17]. The possible reasons for varying number of episodes in different studies could be differing geographic and climatic conditions.
In the current study, episodes of Diarrhoea, ARI & measles were more common in males as compared to females. Our findings are in contrast to a study by Goswami M et al., in Ahmedabad & by Marimuthu P et al., at Delhi slum where majority of the females were either suffering from or have ahistory of one or more illness within the previous two weeks [18–19].
Reflections of poor nutritional status were also observed through high prevalence of PEM, vitamin B complex, and other nutritional deficiencies among preschool children. Vitamin B complex deficiency, had a higher prevalence compared to other nutritional deficiency signs, which might be due to the influence of socio-economic and environmental factors. This may be because of the fact that diet was deficient in pulses and green leafy vegetables, and hence the deficiency of vitamins was apparent.
Malnutrition and Infection goes hand in hand. Various studies have shown that the immunological response in PEM is impaired, Immune mechanism of the body also goes down and hence child becomes more vulnerable for infection thus PEM and infection forms a vicious cycle. The present study also found a significant association between morbidity and nutritional status. Similarly, in Aligarh, presence of measles, vitamin deficiency and worm infestation were significantly associated with malnutrition [20]. Another study in Banaras by Kavita et al., also showed that illness like diarrhea, worms in stool, URTI, had higher incidence in PEM children as compared to Non-PEM children [21]. Further, during illness partial or complete restriction of solid foods in the diet, which if repeatedly followed with recurrence of episodes is likely to affect the nutrition of the child. The cumulative effect of all these factors associated with loss of appetite and increased requirement during illness leads to varying grades of PEM.
The immunization status of the study population was good. The coverage of the vaccines was in general comparable to that reported for migrant tribal children in slums of Orissa, but poorer compared to the studies from Chandigarh and Madhya Pradesh [22–24]. Morbidity was found to be higher (75%) in children who were unimmunized as compared to those who were fully immunized (48.8%) as the unimmunized children are at risk of developing these infections similarly, a significant association was found between ARI and Immunization by Pore at Solapur which is also quoted by various other authors [25–27]. It was observed that preference to seek treatment in the govt. hospitals was higher (57.6%) than other facilities. Treatment of the child by local indigenous practitioners was another preferred treatment observed in the study area which prolonged the course of illness.
Conclusion
Morbidities like diarrhea, respiratory diseases, anaemia, under nutrition, various vitamin deficiencies among under three children in the present study was very common.The underutilization of the Government Health facility was also quite evident. These preliminary findings indicate that there is a need to improve utilization of Primary health care services including the vital MCH services for better child health and survival. The regrettable side to the issue is that most of the morbidities are largely preventable by simple interventions like immunization, adequate nutrition promotion of hygienic practices, through proper health education to their parents. Community health workers should also be trained adequately so that they are able to pick up signs of illness and encourage people in the community to seek treatment. Micronutrient supplementation and health education of the caregivers through simple health packages would go a long way in alleviating the co-morbidities.
*History of Diarrhoea & ARI has been taken for the past 3 months #Multiple responses were obtained