Introduction: Laparoscopic cholecystectomy (LC) is conventionally performed under general anaesthesia (GA) in our institution. There are multiple studies which have found spinal anaesthesia as a safe alternative. We have conducted this study of LC, performed under spinal anesthesia to assess its safety and feasibility in comparison with GA.
Materials and Methods: Fifty patients with symptomatic gallstone disease and American Society of Anesthesiologists status I or II were randomised to have LC under spinal (n = 25) or general (n = 25) anesthesia. Intraoperative vitals, postoperative pain, complications, recovery, and surgeon satisfaction were compared between the 2 groups.
Results: In the SA group six patients (24%) complained of shoulder pain, two patients required conversion to GA (8%) as the pain did not subside with Fentanyl. None of the patients in the SA group had immediate postoperative pain at operated site. Only two (8%) patients had pain score of 4 at the operative site within eight hours requiring rescue analgesic. One patient had nausea but no vomiting (4%). All the patients (100%) in the GA group had pain at operated site immediately after surgery and their pain score ranged from 4-7, all patients received rescue analgesic before shifting to the ward. In the first 24h tramadol required as rescue in the GA group was 82±24 mg which was significantly higher than the SA group requiring only 30±33.16 mg. Although, the GA group had more patients experiencing postoperative nausea & vomiting it was not statistically significant.
Conclusion: SA as the sole anaesthesia technique is feasible, safe and cost effective for elective LC.
Introduction
Laparoscopic cholecystectomy (LC) has become the gold standard for the surgical treatment of symptomatic cholelithiasis and has gained worldwide acceptance [1]. It is a minimally invasive procedure with a significantly shorter hospital stay and a quicker convalescence compared with the classical open cholecystectomy [2].
LC is conventionally done under general anaesthesia (GA) and may be associated with postoperative pain and nausea and vomiting (PONV). Rodgers et al., published a meta-analysis showing that the use of neuraxial techniques for a variety of surgical procedures resulted in a decrease in mortality, venous thromboembolism, myocardial infarction, and several other complications [3]. Regional anaesthesia techniques have been used for performing LC as an alternative to GA. It has been used as a routine technique for otherwise healthy patients. Spinal anesthesia (SA) is a commonly used anaesthetic technique that has a very good safety profile. SA has several advantages over GA, like reduced postoperative pain, nausea, vomiting and smooth post anesthesia recovery period, as the patient is awake and oriented at the end of procedure. There are multiple reports that have been published regarding the feasibility of SA for LC in patients fit for GA [4-10].
The aim of this prospective, randomized prospective study was to evaluate the efficacy, safety and advantages of conducting LC under SA in comparison to GA.
Materials and Methods
The study was approved by the Ethical Committee of the M.S Ramaiah Medical College. Informed consent was obtained from all Sectionthe patients who had agreed to participate in the study. A detailed explanation of the procedure and risks involved was given. The inclusion criteria were: American Society of Anaesthesiologists Grade I and II patients belonging to the age groups of 20-70 y of either sex, admitted with uncomplicated symptomatic cholelithiasis. Exclusion criteria were patients with acute cholecystitis, gallbladder malignancy, previous upper abdominal surgeries, pregnancy and patient unfit or refusing SA.
After detailed preoperative evaluation and preparation for surgery, patients were randomly allocated to either the SA group or the GA group using a table of computer-generated random numbers. All patients were premedicated with oral 150 mg of Ranitidine on the night before and morning of surgery. On arrival in the preoperative room the patient`s non-invasive blood pressure(NIBP), oxygen saturation(SpO2), and heart rate(HR) were recorded.Intravenous(iv) cannulation was done with an 18 G catheter inserted in the forearm and patients received 500ml of Ringer lactate solution, 1mg Midazolam IV and 4mg Ondansetron IV. A 14F nasogastric tube was inserted routinely in all patients and they received prophylactic preoperative intravenous antibiotic ceftriaxone 1 gm/v.
In the SA group SA was performed with the patient in sitting position. After infiltration with 1% xylocaine, a 25 gauge lumbar puncture was done in the L2-L3 intervertebral space. Three ml of hyperbaric bupivicaine (0.5%) and 25 micrograms (mcg) of Fentanyl was injected intrathecally. The patient was then placed in the supine position for 5min. The sensory level of T4 dermatome level was accepted as to allow LC. A Trendelenburg position was given in patients who did not achieve a level of T4 at 5 minutes and sensory level was checked every minute till T4 level was achieved. At the end of 20min if adequate level was not achieved, GA was administered and the patient excluded from the study. As soon as the sensory block level reached T4 dermatome level, the surgery was started. HR, NIBP, and SpO2 were measured and recorded at five minute intervals during the surgery. A decrease in the mean arterial blood pressure(MAP) by more than 20% below the pre-anaesthetic level was managed by intermittent incremental iv boluses of Ephedrine 5mg. Intraoperative shoulder pain was treated with fentanyl 25mcg iv bolus repeated at five minute intervals, with a maximum of 50mcg. GA was induced on persistence of severe pain despite maximum dose of fentanyl.
In the GA group, after pre-oxygenation, induction was done with Propofol (2mg/kg), Fentanyl (2mcg/kg,) and Atracurium (0.5mg/kg).An appropriate size endotracheal tube was inserted after 3min of ventilation. Maintenance of anaesthesia was done with air oxygen mixture enriched with Isoflurane (0.6-1.5%) and controlled mechanical ventilation.
The patients were then placed in the supine, reverse Trendelenburg position with the arms fully abducted and a right up lateral tilt was given.A minimal possible tilt to facilitate exposure of the gallbladder of the patient was used (i.e. minimal use of both reverse Trendelenburg positioning and right shoulder elevation).Pneumoperitoneum was set at a pressure of 12mmHg, initial insufflation of Carbon Dioxide (CO2)was done at a low flow rate (2L/min) and gradually increased to 5L/min. A standard four-trocar technique of LC was followed. Open technique was used for the placement of the umbilical port for the creation of pneumoperitoneum. A zero-degree optical scope was used for the surgery. Dissection of the gallbladder was started at the triangle of Calot with the identification and clipping of both the cystic duct and artery. Mobilization of the gallbladder from the liver bed started at the triangle of Calot. Following removal of the gallbladder, a subhepatic drain was placed, as per our institutional practice.
The operation time was recorded and intraoperative incidents like right shoulder pain, hypotension, nausea and/or vomiting were recorded. Postoperative pain was assessed regularly using a visual analog scale from 0 to 10, with 10 being most severe, for 24h.Intramuscular Tramadol 50mg was used as rescue analgesic and the total dose administered during the first 24h postoperatively was recorded. If the pain did not reduce to a VAS < 4 in 45min, 1gm Paracetamol iv. infusion was given and repeated every six hours.The sub hepatic drain was removed at the end of 24h. Patients were for discharge after 48h. Follow up of the patients was performed at the end of the first and fourth postoperative week.
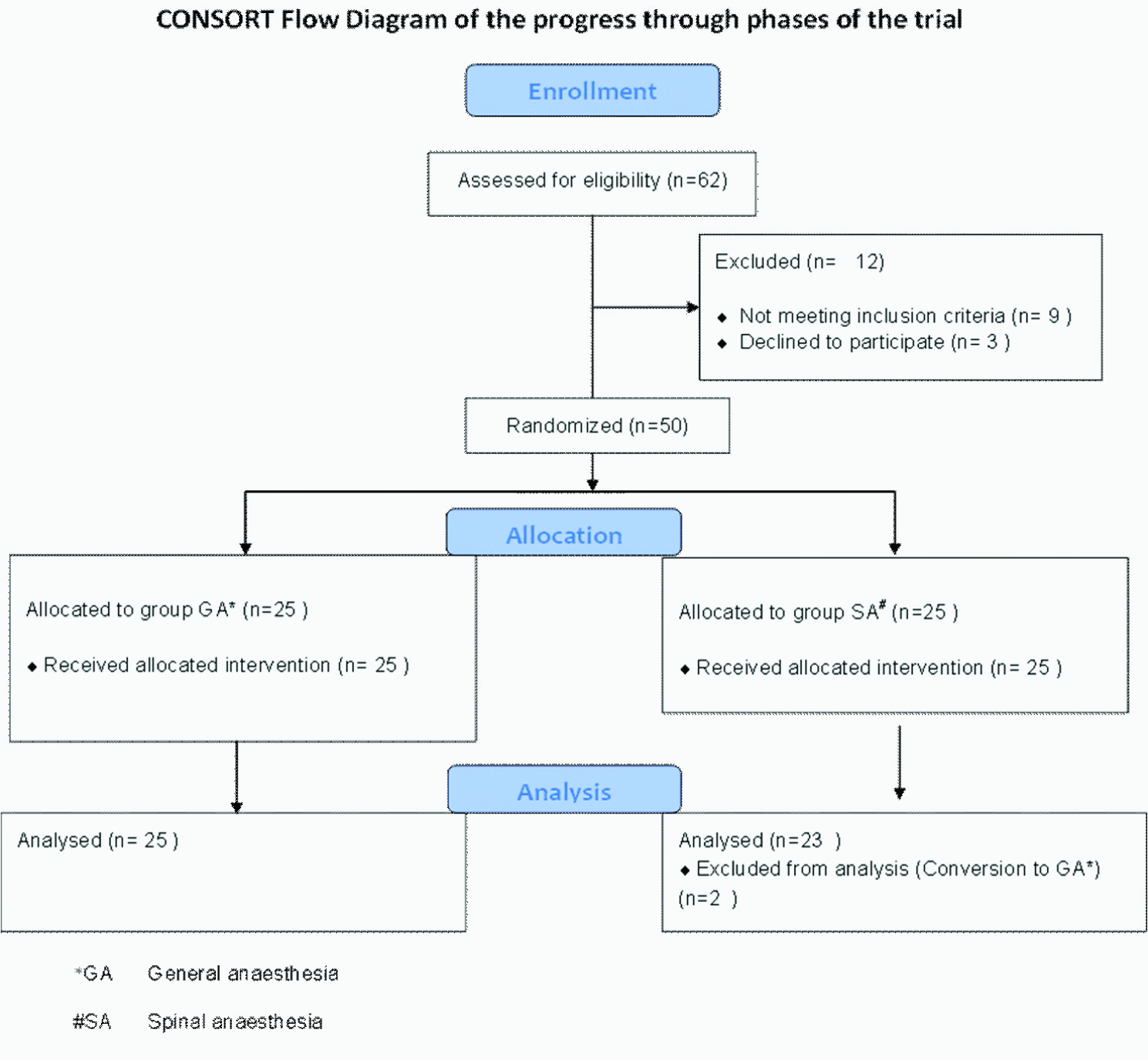
Consort flow diagram of the progress through phases of the trial
Demographics of patients in both groups studied SA: Spinal anaesthesia. GA: General anaesthesia
| SA Group | GA Group | p-value |
| Age (years) mean±standard deviation | 45±11.73 | 47.84±10.49 | 0.383 |
| Gender (n%) Male(36%) | 10 | 8 | 0.391 |
| Female(74%) | 15 | 17 | |
| Age in years | 61.95±7.78 | 64.44±10.22 | 0.383 |
Surgery duration & Surgeon score of operating conditions SA: Spinal anaesthesia. GA: General anaesthesia
| SA Group (n=23) | GA Group (n=25) | p-value |
| Duration of surgery | 97.2±34.08 | 81.95±20.97 | 0.093 |
| Surgeon score of operating conditions | 2.40±0.58 | 2.44±0.57 | 0.822 |
Spinal Anaesthesia group intraoperative events * excluded from further analysis
| Shoulder pain | 6 | 24% |
| Conversion to GA* | 2 | 8% |
| Hypotension | 9 | 36% |
| Nausea intraoperatively | 1 | 4% |
| Vomiting | 0 | |
| Immediate Post op pain | 0 | |
Pain scores and tramadol usage
SA: Spinal anaesthesia. GA: General anaesthesia
| VAS±SD | SA group (n=23) | GA group | p-value |
| Immediate postoperative period | 0 | 5±1.16 | < 0.001 |
| 1 hour post op | 0 | 4.48±1.31 | < 0.001 |
| 2 hour post op | 0 | 3.76±1.34 | < 0.001 |
| 4 hour post op | 0.45±1.35 | 4.16±1.22 | < 0.001 |
| 8 hour post op | 3.55±0.90 | 4.92±1.38 | < 0.001 |
| 24 hour post op | 3.80±0.97 | 3.48±0.94 | 0.28 |
| Total Tramadol used on first post op day (mg±sd) | 30±33.16 | 82±24 | < 0.001 |
Postoperative complication
SA: Spinal anaesthesia. GA: General anaesthesia.
| VAS±SD | SA group (n=23) | GA group | p-value |
| Postoperative nausea &vomiting | 4 | 7 | 0.49 |
| Postoperative spinal headache | 0 | 0 | - |
| Urinary retention | 2 | 0 | 0.48 |
| Wound sepsis | 0 | 0 | - |
Statistical analysis
Statistical analysis was done by student t-test. ANOVA and Chi-square test were performed for nonparametric values and corresponding p-value was computed using SPSS (Statistical Package for the Social Sciences (software version 17) for windows and p-value <0.05 was considered statistically significant.
Results
The study was conducted between October 2012 till March 2013. A total number of 50 patients were included in the study [Table/Fig-1]. In both the groups, all the procedures were completed laparoscopically, and there were no conversion to open cholecystectomy. Both the groups had similar demographic profile. In the SA group, 15 patients were females and 10 patients were males. The mean age was 45±11.73 y [Table/Fig-2]. In the SA group, nine patients had diabetes mellitus which was well controlled and analysisfive patients were hypertensives. The GA group had 8 males and 17 females, their mean age was SD 47.84±10.49 y. Seven patients were well controlled diabetics and six patients were hypertensives on treatment. The duration of surgery was 81.95±20.97 min and 97.2±34.08 min in the GA and SA groups which was not statistically significant. For each procedure the surgeon was asked to give a score of 1-3, regarding the surgical conditions and muscle relaxation; 1 was bad, 2 good and 3 being excellent. The scores were similar for both groups with a mean score of 2.4 [Table/Fig-3].
In the SA group six patients (24%) complained of shoulder pain, two patients required conversion to GA (8%) as the pain did not subside with Fentanyl and they were excluded from further analysis.The other four (16%) patients complained of mild shoulder pains which subsided with inj. Fentanyl. For one patient, mild shoulder pain persisted for 24h. None of the patients in the SA group had immediate postoperative pain at operated site. Only two (8%) patients had pain score of 4 at the operative site within eight hours requiring rescue analgesics. One patient had nausea (4%) but no vomiting which subsided with ondansetron 4mg iv [Table/Fig-4].
All the patients (100%) in the GA group had pain at operated site immediately after completion of operation and their pain score ranged from 4-7, all patients received rescue analgesic before shifting to the ward. In the first 24h tramadol required as rescue in the GA group was 82±24 mg which was significantly higher than the SA group requiring only 30±33.16 mg [Table/Fig-5]. Although, the GA group had more patients experiencing postoperative nausea & vomiting it was not statistically significant.Two patients in the SA group needed catheterisation. None of the patients had postoperative infections or headache [Table/Fig-6].
Discussion
The anaesthetic technique of choice for laparoscopic procedures is GA. Recent studies indicate regional anaesthesia for LC is safe, economical and has good postoperative pain control. But there are concerns associated with SA like raised intra-abdominal pressure resulting in regurgitation of gastric content. There is also a concern of hypotension during laparoscopic procedures done under SA due to the effect of reduced venous return peripheral vasodilatation due to SA and also consequent to increased intra-abdominal pressure and reversed Trendelenburg position [11,12] .
In our study, we had hypotension in nine cases (36%) we could be correct it with saline infusion and vasopressor boluses. Sinha et al., [8] noted an incidence of hypotension as 20.5% in their series. Tzovaras et al., found that intraoperative hypotension is a well-known adverse effect of spinal anesthesia it was easily managed and did not affect the planned procedure [5] .
The mean/median operative time for LC performed under SA in previous studies ranged from 16.4 to 47.4 min [1,4-7] . In our study there was no statistically significant difference in mean operative time between the SA and GA groups suggesting that the use of a low-pressure pneumoperitoneum and SA in LC did not interfere either the adequacy of the surgical view or access thus not prolonging the operative time significantly, Bessa et al., also found similar results [1] .
Although, recent studies have shown that laparoscopy in patients with regional anaesthesia may be tolerated well, shoulder tip pain can be a significant intraoperative problem. The reported incidence for intraoperative right-shoulder pain in previous studies requiring iv fentanyl administration ranged from 10 to 55.2% [6-10] . Referred pain to right shoulder is probably due to irritation of diaphragm by the CO2 pneumoperitoneum [13] . In the our study, six patients (24%) complained of shoulder pain out of which two patients (8%) required conversion to GA. Hamad et al., reported intraoperative right-shoulder pain 10% which was severe enough to necessitate conversion to GA which was similar to our study [4] , but Tzovaras et al., encountered right-shoulder pain in 10 patients (20%) [5] . Sinha et al., reported intraoperative right-shoulder pain in 12.3%patients but none of them required conversion to GA [8] . Yuksek et al., reported an incidence of intraoperative right-shoulder pain in 50%; it was severe enough to necessitate anaesthetic conversion in three patients (10.3%) and in five patients (17.2%), additional spraying of the diaphragm with 2% lidocaine solution was required for control of the pain [6] . Patients in SA group had lower pain scores in the first 24h, but after that the level of postoperative pain was similar in both groups. The additional analgesic requirement was in the GA group was more than double that of the SA group in first 24h in our study. Earlier studies have reported that LC done under SA results in significantly less early postoperative pain and analgesic requirement compared to that performed under GA [1,7] .
The reduced pain in the SA group may be due to a persistent neuraxial blockade by SA and also the use of a low-pressure pneumoperitoneum. A recent meta-analysis concluded that the use of a low-pressure pneumoperitoneum appears effective in decreasing pain after LC[14] .
Although, the incidence of PONV was not significant between both the groups the GA group had more patients with PONV compared to the SA group. Bessa et al., study had 22.2% of the GA group having PONV compared to only 6.9% of patients in the SA group.We inserted a nasogastric tube routinely in all our patients, but many studies have found that a nasogastric tube is not required in patients who have received SA [5-7] . Postoperative urinary retention requiring catheterisation was seen in two patients in the SA group. This is known to be related to regional anesthesia with rates of up to 20% in some series [15] .
No significant difference was noticed in operating time under SA or GA. Although, a low pressure pneumoperitoneum was used the surgeons did not find any difference in the operating conditions and muscle relaxation between both groups.Although we did not calculate cost per case SA on an average costs 1/5th of that of GA (`165 vs. `750 for two hours). LC under SA in 150 patients with low-pressure pneumoperitoneum was found to be a safe and cost-effective procedure by Goyal S et al., [10] .
Limitation
The main limitation of this study would be the small number of the cases and it will be tried to continue on the trial in further research protocols involving patients who are high risk for GA.
Conclusion
This study confirms the feasibility, safety and cost effectiveness of spinal anaesthesia as the sole anaesthesia technique for elective laparoscopic cholecystectomy. The patient outcomes are similar in both techniques this makes SA a cost effective option in developing countries.
[1]. SS Bessa, KM Katri, WN Abdel-Salam, SA El-Kayal, TA Tawfik, Spinal versus general anesthesia for day-case laparoscopic cholecystectomy: A prospective randomized study.J Laparoendosc Adv Surg Tech. 2012 22:550-55. [Google Scholar]
[2]. F Keus, JAF de Jong, HG Gooszen, CJHM van Laarhoven, Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis.Cochrane Database Syst Rev. 2006 4:CD006231 [Google Scholar]
[3]. A Rodgers, N Walker, S Schug, H McKee, A van Zundert, D Dage, Reduction of postoperative mortality and morbidity with epidural or spinal anesthesia: results from an overview of randomised trials. BMJ. 2000 321:1493-97. [Google Scholar]
[4]. JM Hamad, OA Ibrahim El-Khattary, Laparoscopic cholecystectomy under spinal anesthesia with nitrous oxide pneumoperitoneum: A feasibility study. Surg Endosc. 2003 17:1426-28. [Google Scholar]
[5]. G Tzovaras, F Fafoulakis, K Pratsas, S Georgopouloun, G Stamatiou, C Hatzitheofilou, Laparoscopic cholecystectomy under spinal anesthesia. A pilot study.Surg Endosc. 2006 20:580-82. [Google Scholar]
[6]. YN Yuksek, AZ Akat, U Gozalan, G Daglar, Y Yasar Pala, M Canturk, Laparoscopic cholecystectomy under spinal anesthesia.Am J Sur. 2008 195:533-36. [Google Scholar]
[7]. G Tzovaras, F Fafoulakis, K Pratsas, S Georgopoulou, G Stamatiou, C Hatzitheofilou, Spinal vs. general anesthesiafor laparoscopic cholecystectomy. Interim analysis of a controlled, randomized trial.Arch Surg. 2008 143:497-501. [Google Scholar]
[8]. AS Sinha, AK Gurwara, SC Gupta, Laparoscopic cholecystectomy under spinal anesthesia: A study of 3492 patients.Laparoendosc Adv Surg Tech A. 2009 19:323-27. [Google Scholar]
[9]. S Tiwari, A Chauhan, P Chaterjee, MT Alam, Laparoscopic cholecystectomy under spinal anaesthesia: A prospective, randomised study.J Min Access Surg. 2013 9:65-71. [Google Scholar]
[10]. S Goyal, S Goyal, S Singla, Laparoscopic Cholecystectomy Under Spinal Anesthesia with Low-Pressure Pneumoperitoneum - Prospective Study of 150 Cases.Arch Clin Exp Surg. 2012 1(4):224-28. [Google Scholar]
[11]. CN Gutt, T Oniu, A Mehrabi, P Schemmer, A Kashfi, T Kraus, Circulatory and respiratory complications of carbon dioxide insufflation.Dig Surg. 2004 21:95-105. [Google Scholar]
[12]. EA Hirvonen, EO Poikolainen, ME Pääkkönen, LS Nuutinen, The adverse hemodynamic effects of anesthesia, head-up tilt, and carbon dioxide pneumoperitoneum during laparoscopic cholecystectomy.Surg Endosc. 2004 14:272-77. [Google Scholar]
[13]. L Sarli, R Costi, G Sansebastiano, M Trivelli, L Roncoroni, Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shouldertip pain following laparoscopy. Br J Surg. 2000 87:1161-65. [Google Scholar]
[14]. KS Gurusamy, K Samraj, BR Davidson, Low-pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy.Cochrane Database Syst Rev. 2009 (2):CD006930 [Google Scholar]
[15]. G Jensen, F Mikkelsen, K Kehlet, Postherniorrhaphy urinary retention: effect of local, regional, and general anesthesia: a review.Reg Anesth Pain Med. 2002 27:612-17. [Google Scholar]