Dengue virus is a flavi virus transmitted by aedes mosquito. There are four closely related but antigenically distinct serotypes of Dengue viruses (DEN-1-4). Infection with any serotype causes a spectrum of clinical features ranging from asymptomatic infection, undifferentiated fever and classical dengue fever (DF) to life threatening manifestation like dengue haemorrhagic fever (DHF) to dengue shock syndrome (DSS). Globally dengue is an emerging disease that causes an estimated 50-100 million infections, 500,000 dengue haemorrhagic fevers and 22,000 deaths annually [1]. Since the symptoms of dengue virus infection are insufficient for clinical differentiation from other viral illnesses, definitive diagnosis relies on laboratory tests. A rapid and accurate diagnosis of dengue in the acute phase of illness is important for initiation of therapy as well as for early enhancement of epidemic control measures especially in low endemic areas. Detection of specific IgM antibody by ELISA forms the mainstay for diagnosis. However, IgM antibodies develop after 4 to 5 days of infection. Viral isolation is the gold standard for diagnosis and serotyping of dengue virus infection, but this method is time consuming and requires sophisticated laboratory [2]. Molecular diagnosis such as RT- PCR requires experienced personnel and specialized laboratory equipments. As an alternative the detection of NS1 antigen of dengue virus has been identified as highly conserved glycoprotein expressed on either membrane bound or secreted form [3].
Materials and Methods
Type of study - survey
One thousand and twenty serum samples were collected from clinically suspected cases of dengue fever during the outbreak in Angul district of Odisha during the month of August- September, 2011. Blood samples were collected from the patients of the epidemic affected area and sent to the Department of Microbiology, S.C.B Medical College, Cuttack, which is the referral hospital for eastern Odisha. Majority of the samples were collected during the acute phase of illness i.e. 1-5 days of fever. The samples were grouped into 3 categories according to the days of fever - 1-5,6-10, >10 d. Serum was separated from all the samples and subjected for NS1 Ag detection.
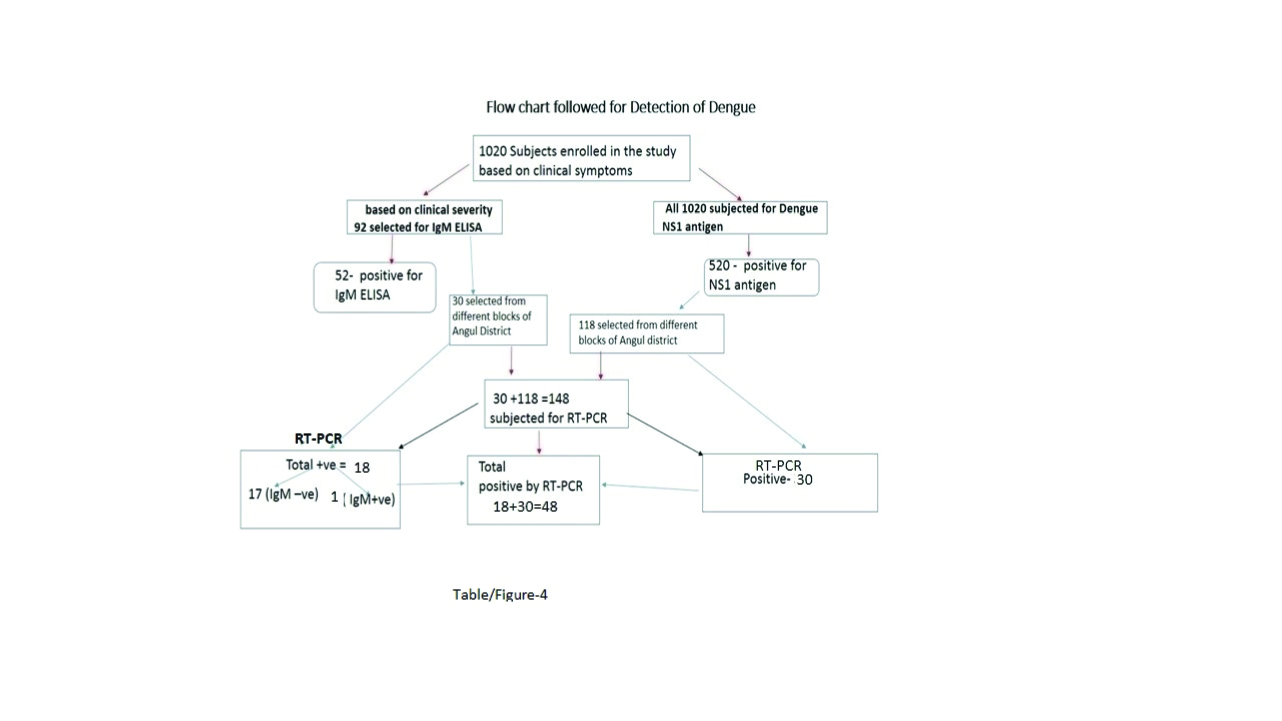
As IgM ELISA & genotyping by RT-PCR was not possible for all samples in our resource constraint laboratory, 92 out of 1020 samples were selected, based on their clinical severity of illness (fever, rash, bleeding manifestation, arthralgia), for further study of IgM ELISA and platelet count & 148 NS1 positive samples were selected from different Blocks of Anugul district for RT-PCR at NIV, Pune which also included 30 out of the 92 samples for Ig M ELISA [Table/Fig-1].
Flow chart followed for detection of dengue
Control- Twenty blood samples from healthy individuals were collected as control& subjected for detection of both NS1 Ag and dengue specific IgM.
NS1 Ag assay: The test was performed using NS1Ag MICROLISA (J. Mitra& Co, New Delhi) test kit as per manufacturer’s instruction.
Detection of IgM: The Dengue IgM capture ELISA (Panbio, Australia) was used & interpreted as per the recommendations of the manufacturers.
Platelet Count: EDTA blood samples were collected & the platelet count was done in the Department of Pathology, S.C.B Medical College, Cuttack and interpreted as normal, when the count was between 1, 50, 000- 4, 50, 000 and DHF, when the count was < 1, 00, 000/ cmm( WHO cutoff for platelet count for DHF).
Results
Out of the 1020 blood samples screened, 513 (50.2%) were positive for dengue NS1 Ag with a two tailed p-value of < 0.0001 (Z-statistics), among which majority were males 427(83.2%) between the age group of 21- 40 y [Table/Fig-2]. Among the 513 NS1Ag +ve cases 88% were detected during 1-5 days of fever.
Age and sex distribution of the NS1Ag positive cases. (N=513)
| Age Group | Male | Female | Total (%) |
|---|
| 0-10 | 4 | 5 | 9(1.7) |
| 11-20 | 52 | 9 | 61(11.8) |
| 21-30 | 169 | 34 | 203(39.5) |
| 31-40 | 111 | 21 | 132(25.7) |
| 41-50 | 70 | 13 | 83(16.1) |
| >50 | 21 | 4 | 25(4.8) |
| Total | 427(83.2) | 86(16.7) | 513(100) |
When detection of NS1Ag and IgM were taken into account together for diagnosis, 81.2% & 47.19% respectively were found to be positive during 1- 5 days, then 65.6% & 81.2% during 6-10 days & only 6.2%& 87.5% after 10days. Both tests were positive in 25% cases during 1-5 days and 56.8% were positive for only NS1Ag which were missed by IgM capture ELISA. However, after 10 days of fever, 81.2% were positive by IgM ELISA and all were negative for NS1Ag [Table/Fig-3]. The IgM positivity was 47.1% with a sensitivity & specificity of 30.6 & 100% within 5 days, increased to 81.2% (sensitivity-90.48% & specificity 36.6%) during 6-10 days & peaked to 87.5% (sensitivity -100 %, specificity -13.33%) after 10 days [Table/Fig-4]. All the 20 samples from controls were negative by both the assays. RT-PCR resulted 32.4% positivity out of the 148 selected NS1Ag positive samples. Among them 20% were +ve out of (5) IgM +ve & 68 % out of (25) IgM -ve cases. The genotypes 1,2 &3 were identified in 6,39&3 number of cases respectively [Table/Fig-4].
Comparison of NS1Ag detection and Ig M ELISA for diagnosis of dengue during different days of fever
| (N=92) Sample age | NS1 +ve IgM +ve | NS1 +ve IgM -ve | NS1 –ve IgM +ve | NS1 –ve IgM -ve | Total-58 (NS1 +v) | Total Ig M+ve |
|---|
| D1-5 (n=44) | 11(25%) | 25 (56.8%) | 0(0.0%) | 8 (18.2%) | 36 (81.2%) | 11 47.1%) |
| D6-10 (n=32) | 19 (59.3%) | 2(6.2%) | 7 (21.8%) | 4 (12.7%) | 21 (65.6%) | 26 (81.2%) |
| D10 (n=16) | 1(6.2%) | 0 (0%) | 13(81.2%) | 2(12.6%) | 1 (6.2%) | 14 (87.5%) |
Distribution of RT-PCR positivity in NS1 antigen positive cases
| NS1 Ag +ve cases 30+118=148 | +ve for genotype -1 | +ve for genotype -2 | +ve for genotype -3 | Total No(%) |
|---|
| NS1+ve IgM -ve (25) | 2 | 15 | 0 | 17 (68) n =25 |
| NS1+ve IgM+ve (5) | 0 | 0 | 1 | 1(20) n =5 |
| NS1+ve (118) | 4 | 24 | 2 | 30(25.4) |
| Total | 6 | 39 | 0 | 48(32.4) n=148 |
Discussion
Dengue is an endemic viral disease affecting tropical and subtropical regions around the world [4]. Dengue infection presents with non specific fever that mimics other viral illnesses. However, according to WHO case definition dengue fever (DF) is defined as acute febrile illness with two or more manifestations among headache, retro-orbital pain, myalgia, athralgia, rash, haemorrhagic manifestations and leucopenia. Dengue haemorrhagic fever (DHF) is defined as 2- 7 days of acute febrile illness with bleeding, thrombocytopenia and evidence of plasma leakage. When all the features of DHF are present along with circulatory failure then the patient is categorized as dengue shock syndrome (DSS) [5]. Bleeding manifestation was not a common feature in our study, majority of the patients presented with fever, headache, myalgia and generalized rash except four cases who presented with DHF and two cases with DSS which correlates well with other authors [6]. But others had reported higher incidence of bleeding manifestations in their study [7,8]. The major diagnostic methods currently available are viral culture, viral RNA detection by RT-PCR and serological tests such as IgM capture ELISA. Current strategy under National Vector Disease Control Program( NVBDCP) suggests that diagnosis of a particular flavi virus should always be made taking into account the clinical presentation, the performance of serological tests and the knowledge of the flavi virus circulating in that particular geographic region. Tests for antigen and antibody detection are widely used for confirmation of dengue infection. However, performance of tests depends upon specificity and sensitivity of the test kits used. High specificity is important if the tests are being used to confirm dengue as the cause of the outbreak whereas sensitivity is very important if the tests are to be used to support clinical diagnosis and for case management [9]. Following the bite of an infected aedes mosquito, dengue virus replicates quickly before the development of signs and symptoms. NS1 Ag circulates uniformly in all serotypes of dengue virus and circulates at high level during the 1st few days of illness [10]. This is the reason for high detection rate of NS1Ag in acute phase sera, there after decreases gradually and antibody detection becomes more prominent after 5 days.
In the present study 50.2% samples were found to be positive by NS1Ag detection with a highly significant p-value (<0.0001). Majority was in the age group of 21-40 & detected during 1-5 days with a mean day of 5. Similar male preponderance was observed by various authors in previously reported outbreaks [11,12]. Srivastav et al., reported only 26% NS1Ag positivity but Dutta and Wattal had reported higher percentage of NS1Ag positivity (71.42%) in acute phase sera [13,14].
Earlier studies found the presence of NS1Ag in 82-83% of patients with dengue infection from day 1 up to 9 to 18 days after the onset of fever [15,16]. We detected maximum NS1Ag positivity (81.2%) in 1 to 5 days of fever. But low sensitivity of NS1 protein tests was evidenced during a dengue type 2 virus outbreak in Santos, Brazil, in 2010 [17]. Among the 92 subjects selected for IgM capture ELISA, only 47.1% were positive during 1 -5 days of fever. But after 10 days IgM positivity was 87.5%. During 6-10 days, though 81.2% could be detected by Ig M in comparison to 65.6% +ve for Ns1 Ag, but this difference is not significant statistically. But after 10th day 81.2% were positive by IgM ELISA and all were negative for NS1Ag [Table/Fig-3]. The 4 cases of DHF and DSS were also positive for IgM ELISA with low platelet count. Aditi A et al., had reported IgM capture ELISA to be 98.4% specific and 96.4% sensitive for the diagnosis of dengue infection [4].
Our study found 90.4-100% sensitivity of Ig M ELISA after 6th day onwards but the specificity is low. During 1-5 days, 56.8% were positive for only NS1Ag which were missed by IgM capture ELISA because, development of dengue specific IgM depends on the time taken for an infected person’s immune response to produce antibodies. Thus IgM ELISA does not provide early diagnosis of dengue infection. Moreover, a single serological detection of IgM is merely indicative of recent infection and should not be interpreted as confirmatory [13]. In this context NS1Ag detection has the added advantage of giving good detection rates up to 7 days of illness.However, some authors emphasize the use of combination kit for detection of additional cases of dengue, which are negative for NS1 antigen but positive for IgM and/or IgG antibodies [18].
RT-PCR, though a sensitive and specific method, could detect only 32.4% of the 148 selected NS1Ag positive samples in our study. This low positivity may be due to failure of maintenance of stringent condition for storage and transportation of the samples. Moreover, RNA detection could be possible only in 20% of IgM +ve in contrast to 68% IgM -ve cases. The possibility for this may be due to neutralization of viral components after appearance of IgM antibodies. The predominant serotype identified was serotype – 2 (39/48) followed by serotype- 1(6/48) and serotype- 3(3/48). The major serotype reported from PGI, Chandigarh during the outbreak in the year 2007 was serotype-1, but in 2005 it was serotype-2 [11]. A study from Delhi had reported concurrent prevalence of all the serotypes during 2008 [19]. Major dengue epidemics have been observed in the Indian subcontinent since the 1980s & researchers from the Pune-based NIV found that Indian DENV-2 strains isolated from 1956 to 2005 belonged to only two of the six genotypes — American and Cosmopolitan [20].
Conclusion
NS1Ag is an effective method in comparison to MAC ELISA for diagnosis of dengue virus infection, especially within first five days of illness. The morbidity and mortality of dengue fever can be reduced by early diagnosis and symptomatic management. However, from sixth day onwards combination of MAC ELISA and NS1Ag assay would increase the sensitivity of diagnosis and after 10 days IgM ELISA should be the method of choice for diagnosis. RT-PCR is mandatory for genotyping to ascertain the cause of the current outbreak.