A Sequential Approach in Treatment of Endo-Perio Lesion A Case Report
Sharanappa Kambale1, Nagaveni Aspalli2, Anil Munavalli3, Nishant Ajgaonkar4, Roopa Babannavar5
1Senior Lecturer, Department of Conservative Dentistry & Endodontics, Vasantdada Patil Dental College and Hospital Kavalapur, Sangli, Maharashtra India.
2Reader, Department of Conservative Dentistry & Endodontics,AME’S Dental College, Raichur, Karnataka, India.
3Reader, Department of Conservative Dentistry & Endodontics, Vasantdada Patil Dental College and Hospital Kavalapur, Sangli, Maharashtra India.
4Postgraduate Student, Department of Conservative Dentistry & Endodontics, Vasantdada Patil Dental College and Hospital Kavalapur, Sangli, Maharashtra India.
5Senior Lecturer, Department of Conservative Dentistry & Endodontics,Jodhpur Dental College General Hospital, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sharnappa Kambale, Senior Lecturer, Department of Conservative Dentistry and Endodontics, Vasantdada Patil Dental College and Hospital, Tq- Miraj, Sangli-416306, Maharashtra, India. Phone : 9665697624,
E-mail: sharanappakambale@rediffmail.com
Endo-perio lesions primarily occur by way of the intimate anatomic and vascular connections between the pulp and the periodontium. Endodontic-periodontal combined lesion is a clinical dilemma because making a differential diagnosis and deciding a prognosis are difficult. An untreated primary endodontic lesion may become secondarily involved with periodontal breakdown, which clinically present unusual signs and symptoms. This may delay the diagnosis and hence the correct treatment. This case report describes diagnosis and treatment protocol for an endo-perio lesion of primary endodontic with secondary periodontal involvement.
Bone graft, Endo-periolesion, Root canal treatment
Case Report
Examination
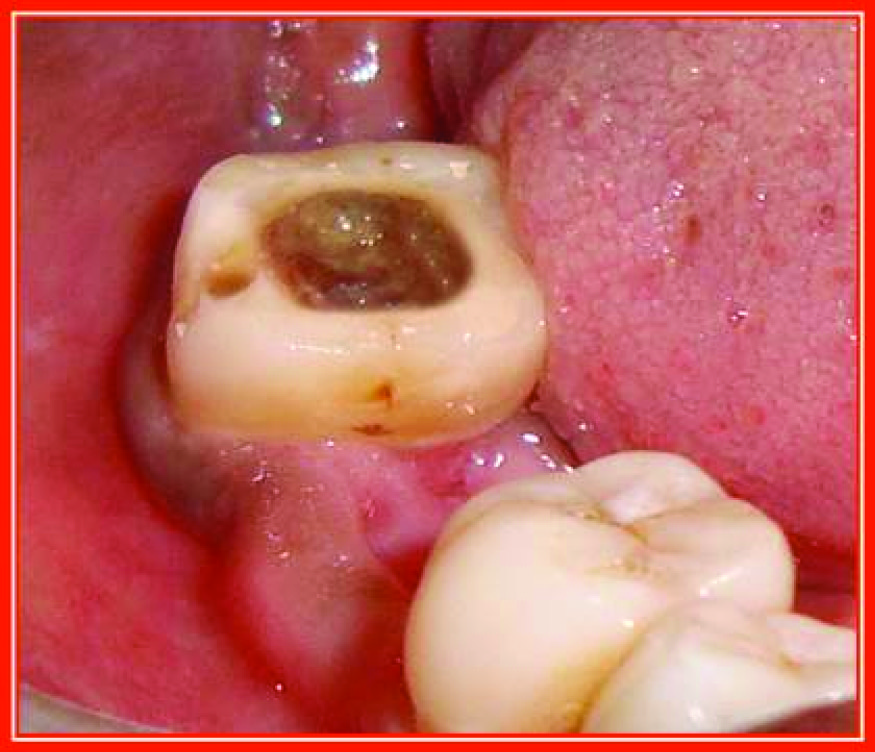
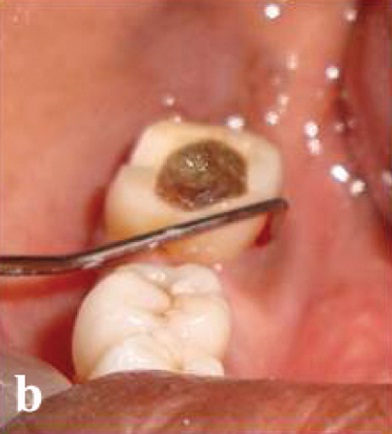
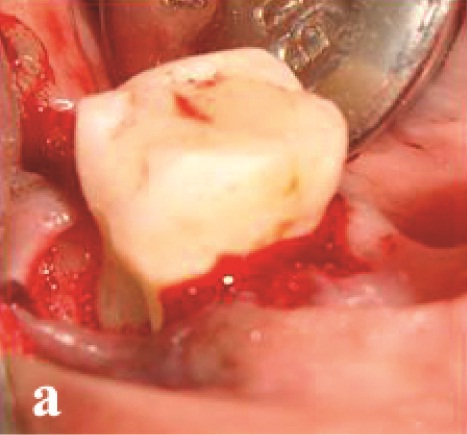
A female patient 32-year-old complained of pain in lower right back region of tooth since eight days. Medical history & dental history are not contributory. On intraoral examination, there was deep dental caries in association with 47 [Table/Fig-1], which was tender on both horizontal and vertical percussion .Tooth was nonvital on pulp testing & 46 was found missing. On periodontal examination – there was deep periodontal pocket 8 mm buccally and 10mm lingually in relation to 47 [Table/Fig-2a,2b]. Probing with nabers probe revealed grade III furcation defect as per Glickman’s Classification of furcation involvement[1].
Investigations
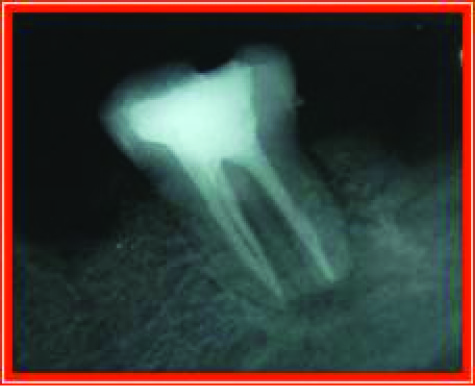
Radiograghic examination revealed radiolucency involving with enamel, dentin and pulp. It also involves furcation area and periapical region of both mesial and distal root, extruding along the lateral surface of root which is continuous with periodontal space. Tooth was mesially drifted slightly [Table/Fig-3]. Electric pulp testing (Parkel Electronics Division, Farmingdale, NY) was done to check for tooth vitality, which confirmed that the tooth was nonvital.
Diagnosis
From above mentioned finding we arrive to diagnose it is as an endo-perio lesion of primary endodontic with secondary periodontal involvement.
Treatment Planning
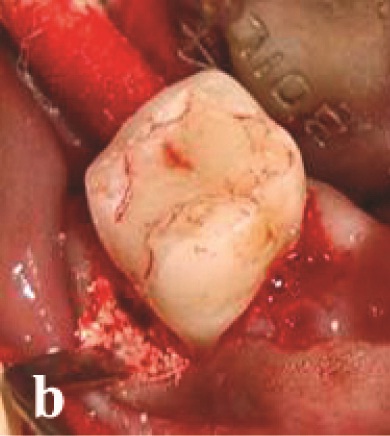
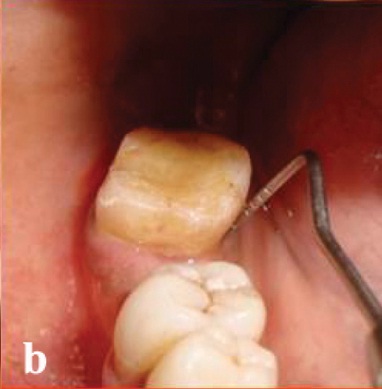
Observing the strategic importance of this tooth as it is last serving molar present, if extraction is carried out, than only two options remain i.e. Removable partial dentue RPD & Implant. RPD would be uncomfortable to the patients, and implant would be expensive. So a multidisciplinary approach was formulated to salvage the tooth. Initially endodontic therapy was performed followed by periodontal therapy. Endodontic treatment was taken up first and the patient was followed up for two months. At the end of second month, radiograph was taken with 47 which showed that the furcation involvement still prevailed [Table/Fig-4]. On clinical examination; it was observed that there was no change in the periodontal measurements. Therefore, periodontal regenerative surgery was planned for treatment of furcation defect. After taking care of asepsis and sterilization the surgery was planned. The area selected for surgery was anesthetized using xylocaine with adrenaline 1:80,000. First crevicular incision was placed & full thickness flap was elevated buccally & lingually. After reflection, thorough degranulation and debridement was done of defect area using Gracey’s curette # 13 and 14 [Table/Fig-5a]. After complete degranulation it was seen as an intrabony defect of vertical dimension of 8 mm. After root conditioning with tetracycline hydrochloride solution, adequate isolation of area was done with proper bleeding control and bone graft material (sterile hydroxyapatite and β tricalcium phosphate granules) (BioGraft-HA® NANO) was carried to the area with bone graft carrier and placed in increments with proper condensation [Table/Fig-5b]. The flap was secured with suture & periodontal dressing was given [Table/Fig-6], which was removed after seven days. Six months of postoperative therapy, the normal probing depth of 2 mm was achieved [Table/Fig-7a,7b].
Discussion
Pulp and periodontium have embryonic, anatomic and functional interrelationship. Simring and Golberg first described their relationship. One of the most common challenges in today’s clinical practice is to treat Endo-perio lesion. Simultaneous existence of pulpal problem and inflammatory periodontal diseases can complicate diagnosis and treatment planning and affect the sequence of care to be performed [2]. This is particularly true for patients of advanced periodontitis, tooth loss and pulpal diseases. Diagnosis is often challenging because this diseases have been primarily studied as separate entities and such primary diseases may mimic clinical characteristics of other diseases [3]. A thorough history and careful clinical and radiographic examination are required to identify and accurately assess the contribution of each lesion to patient’s problem and to determine the sequence that produces optimal results [4].
Endodontic treatment is highly predictable & when appropriately performed has high success rate.Periodontal lesion cannot as long as endodontic lesion is present; but effective endodontic treatment cannot eliminate periodontal pocket [5]. If majority of bony support has been lost from periodontitis, regardless of predictability of endodontic therapy, tooth may have hopeless prognosis. Regeneration, root resection and hemisection are indicated as a part of strategic treatment of multirooted teeth [6,7]. In this case first endodontic therapy was performed then periodontal therapy & bonegrafting was done for periodontal regeneration.
In this report the pulp vitality test which showed the nonvital nature of the tooth was a pivoting finding suggesting the primary endodontic involvement. Generally, in a case of combined endo-perio lesion, an adequate endodontic therapy would result in healing of the endodontic component, and the prognosis would finally depend on the efficacy of periodontal repair/regeneration initiated by either of the treatment procedures. In this case, following endodontic treatment the periodontal lesion did reduce to an extent on radiographic evaluation after two months but did not subside completely with no change in the clinical parameters. This confirmed a secondary periodontal involvement along with primary endodontic component.
When the aetiology is purely endodontic, calcium hydroxide can be used as an intracanal medicament. Because of its bactericidal, anti-inflammatory and proteolytic properties, it inhibits resorption and favors repair [3]. It is especially effective in endodontic lesions with extensive periapical pathology and pseudo pockets, because of its temporary obturating action which would inhibit periodontal contamination of the instrumented canals via patent channels of communication. This regimen usually will resolve the pseudo pocket within a few weeks. However, lesions which are not true combined lesions, little or no improvement would be seen with the periodontal perspective after endodontic treatment, leaving a very poor and often hopeless prognosis [5]. But with the advent of new regenerative materials however, successful periodontal treatment of such lesions has been possible [8].
As there was Grade III furcation defect with deep periodontal pocket 8mm buccally & 10 mm lingually in relation to 47, Hydroxyapatite (Ca10(PO4)6 (OH)2) and beta-tricalcium phosphate (Ca3(PO4)2) bone graft materials were used. These are biocompatible and osteoconductive materials that offer a chemical environment and a surface conducive to new bone formation [1]. These are brittle materials and have low fracture resistance. Different preparative methods lead to either a compact or porous material with interconnective macropores that are spatially and structurally equivalent to cancellous bone. Commercially available hydroxyapatite is resorbed very slowly, under normal physiological conditions, whereas beta-tricalcium phosphate is generally resorbed within 6 weeks after implantation. When used as a mixture, biodegradable hydroxyapatite/beta-tricalcium phosphate ceramics have the
ability to dissolve, break down, and allow new bone formation and
remodeling required to attain optimal mechanical strength without
interference [9]. Hydroxyapatite crystals and β-tricalcium phosphate
act as scaphold on which osteoblasts act, to form the bone and
preserves the space for regeneration. It took one month for epithelial
attachment to establish & complete bone formation will occur at the
end of 6th month after periodontal surgery.
Maintenance stage starts even before surgery and it is the responsibility of dentist to advise the importance of periodontal treatment. The success of treatment depends on the oral hygiene maintenance by the patient. Patient should be instructed about the oral hygiene for the better outcome of the treatment.
Preoperative clinical photograph
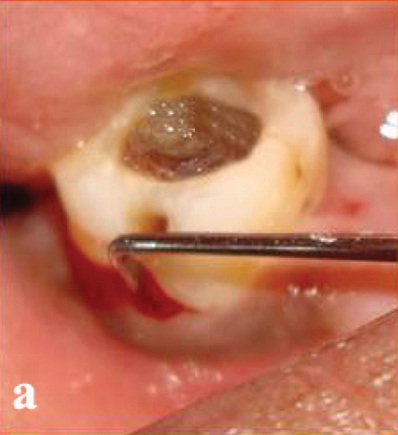
Periodontal probing on lingual aspect
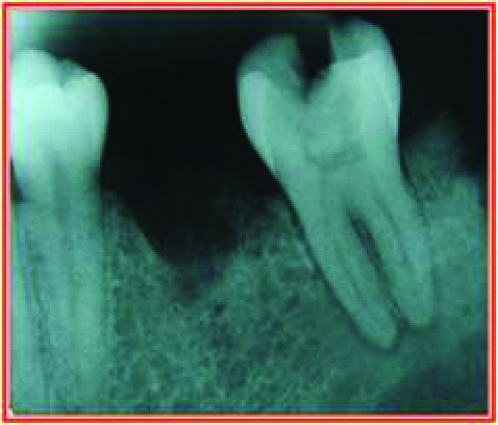
Completion of endodontic therapy


Post-operative period of six months
Conclusion
Diagnosis of teeth with combined endo-perio problems may be difficult to establish, hence, requiring proper history, and use of various diagnostic aides to obtain accurate diagnosis. Lesions with combined causes will require both endodontic & periodontal therapy. In addition, regenerative techniques, root resection & hemi sections offer alternative approaches, thus enhancing clinician’s ability to deal with these complex clinical problems.
[1]. I Glickman, Clinical periodontologySaunders Philadelphia 1953 [Google Scholar]
[2]. M Simring, M Goldberg, The pulpal pocket approach: retrograde periodontitis.J Periodontol. 1964 35:22 [Google Scholar]
[3]. SA Schwartz, MA Koch, DE Deas, CA Powell, Combined endodontic-periodontic treatment of a palatal groove: A case report.J Endod. 2006 32:573-8. [Google Scholar]
[4]. DD Peters, JC Baumgartner, L Lorton, Adult pulpal diagnosis: I-evaluation of the positive and negative responses to cold and electrical pulp tests.J Endod. 1994 20:506-11. [Google Scholar]
[5]. BF Paul, JW Hutter, The endodontic-periodontal continuum revisited: new insights into etiology, diagnosis and treatment.J Am Dent Assoc. 1997 128:1541-48. [Google Scholar]
[6]. H Ehnevid, LE Jansson, SF Lindskog, LB Blomlöf, Periodontal healing in relation to radiographic attachment and endodontic infection.J Periodontol. 1993 64:1199-204. [Google Scholar]
[7]. RT Czarnecki, H Schilder, A histologic evaluation of the human pulp in teeth with varying degrees of periodontal disease.J Endod. 1979 5:242-53. [Google Scholar]
[8]. S Peeran, M Thiruneervannan, K Abdalla, M Mugrabi, Endo-Perio Lesions.International Journal Of Scientific & Technology Research. 2013 5:268-74. [Google Scholar]
[9]. Bansal Evaluation of hydroxyapatite and beta-tricalcium phosphate mixed with bone marrow aspirate as a bone graft substitute for posterolateral spinal fusion.Indian J Orthop. 2009 43(3):234-39. [Google Scholar]