Pre-hypertension which refers to blood pressure in the range of 120 to 139 mm of Hg / 80 to 89 mm of Hg is highly prevalent in developing countries including India [1,2]. In recent years, much attention has been focused on subjects with prehypertension, as risk for the development of cardiovascular disease is higher in these subjects compared to those with normal blood pressure [3].
Hyperhomocysteinemia is considered as one of the major non conventional cardiovascular risk factors. Previous studies have reported elevated homocysteine levels in subjects with hypertension [4]. The ATTICA study (The ATTICA study is a cross-sectional population-based survey conducted in the Attica region during 2001 to 2002.) has demonstrated higher homocysteine levels in prehypertensive subjects compared to normotensive subjects [5].
C-reactive protein is a marker of systemic inflammation that has been associated with an increased risk of myocardial infarction and stroke. Inflammation has been hypothesised to play a role in the development of hypertension and cross-sectional studies have demonstrated higher C-reactive protein levels among individuals with elevated blood pressure [6]. Insulin resistance is a well-established entity in several cardiovascular disorders including hypertension. Recent reports have indicated the existence of insulin resistance in prehypertension.
Even though risk for cardiovascular disease is more in prehypertension, there are only limited data available about non conventional risk factors in these subjects. Various studies have documented insulin resistance and high hs-CRP in prehypertension. However, to best of our knowledge there are no Indian studies, which reported evaluated homocysteine, vitamin B12 and folate in prehypertension. So the present study was designed to evaluate homocysteine, C-reactive protein and insulin resistance in prehypertensive subjects. Further, we elucidated the association of serum homocysteine, vitamin B12, folate, hs-CRP and insulin resistance with blood pressure.
Materials and Methods
The study was conducted in Department of Biochemistry in collaboration with the Department of Medicine,Jipmer,Puducherry, India. Subjects were classified as normotensive and prehypertensive as per the recommendations of the Joint National Committee 7 report. Sixty prehypertensives and 32 normotensives in the age group of 25 to 45yrs with BMI <30 kg/m2 were enrolled in this study. Patients with history of diabetes, renal disease, endocrine dysfunction, coronary heart disease, infections, smokers, alcoholics, and those who are on any kind of medications were excluded from the study. A written informed consent was obtained from all patients. The study was approved by institutional ethical committee.
Blood pressure was measured using sphygmomanometer (Diamond, India) with subjects in sitting position, leg uncrossed and after five minutes of rest. Blood pressure was measured on both arms and higher of the two was taken into consideration. Blood pressure was measured three times after a rest of five minutes in between the measurements. The average of three values was used for study.
Blood Sample collection: Fasting blood sample (5ml) was collected; serum was separated and used for the estimation of glucose and lipid profile immediately. Rest of the sample was stored at -80oC for the analyses of other biochemical parameters. Serum glucose, total cholesterol, triglycerides and HDL-Cholesterol were estimated using reagent kits form Biosystem adapted to Olympus AU 400 autoanalyser USA. Homocysteine, vitamin B12, Folate and Insulin were estimated by chemiluminiscence method (ADVIA Centaur,Seimens) and hs-CRP was estimated by ELISA kit from Diagnostics Biochem, Canada. Insulin resistance was calculated using the Mathew’s formula HOMA-IR = Fasting glucose (mmol/L) x Fasting insulin (μU/mL) / 22.5 [7]. LDL - Cholesterol was estimated by Friedewald’s formula.
Statistical Analysis
Data are expressed as mean ± SD. Independent t-test was used to compare means of the various variables between controls and prehypertensive subjects. Pearson correlation was used to see the correlation of various variables with systolic blood pressure and diastolic blood pressure.
p-value <0.05 was considered as significant for all statistical tests. All analyses were performed with Graph pad prism version 5 by Graph pad software Inc California.
Results
The present study was undertaken to evaluate the homocysteine, vitamin B12, folate and insulin resistance in subjects with prehypertension.
There was significant difference in Systolic and Diastolic Blood pressure between the two groups. The general variables including anthropometric and biochemical parameters were comparable between both the two groups except the age which was higher in the pre-hypertension group than the control group [Table/Fig-1].
Comparison of various general variables in control and subjects with prehypertension
| Variables | Control (n=32) | Prehypertensives (n=60) | p-value |
|---|
| Age(years) | 28.53±4.87 | 37.00±5.67 | <0.05 |
| SBP(mm/Hg) | 110.7±6.07 | 127.5±5.19 | <0.01 |
| DBP(mm/Hg) | 64.75±6.6 | 77.65±4.77 | <0.01 |
| Height(cm) | 170.9±6.06 | 161.4±7.00 | NS |
| Weight(kg) | 69.81±6.12 | 63.8±6.0 | NS |
| BMI(kg/m2) | 23.12±1.99 | 24.51±2.12 | NS |
| Glucose(mg/dL) | 74.78±11.59 | 79.35±10.29 | NS |
Values are expressed as mean±SD, NS-Not significant. SBP-systolic Blood pressure,DBP-Diastolic Blood pressure
Total cholesterol, Triacylglycerol, VLDL-C and LDL-C were significantly increased in prehypertensive subjects when compared to control group, but there was no difference in HDL-C between the two groups [Table/Fig-2].
Comparison of lipid profile in control and subjects with prehypertension
| Variables | Control(n=32) | Prehypertensives (n=60) | p-value |
|---|
| T. Cholesterol(mg/dL) | 164.63±36.96 | 196.07±25.16 | <0.01 |
| Triacylglycerol(mg/dL) | 97.94±57.49 | 125.2±48.35 | <0.05 |
| HDL-C(mg/dL) | 36.53±5.58 | 36.67±8.71 | NS |
| VLDL-C(mg/dL) | 20.51±11.95 | 24.95±9.67 | <0.05 |
| LDL-C(mg/dL) | 107.59±34.90 | 134.45±25.10 | < 0.05 |
Values are expressed as mean±SD, NS-Not significant
Cardiovascular risk parameters, Homocysteine, hs-CRP, insulin and insulin resistance were significantly increased in prehypertensive subjects when compared to control group. But, there was no statistically significant difference in the levels of folate and vitamin B12 [Table/Fig-3].
Comparison of cardiovascular risk parameters in control and subjects with prehypertension
| Variables | Control(n=32) | Prehypertensives (n=60) | p value |
|---|
| Insulin(μU/mL) | 10.54±4.89 | 14.09±8.65 | <0.05 |
| Homocysteine(μmol/L) | 17.18±4.39 | 20.69±7.01 | <0.05 |
| Vitamin B12(pg/mL) | 223.91±77.29 | 259.15±70.72 | NS |
| Folate(ng/mL) | 6.13±3.60 | 5.31±2.51 | NS |
| hs-CRP(ng/mL) | 1438.09±1296.07 | 3748.0±1746.2 | <0.01 |
| HOMA-IR | 1.96±1.11 | 2.73±1.69 | <0.05 |
Values are expressed as mean±SD, NS-Not significant
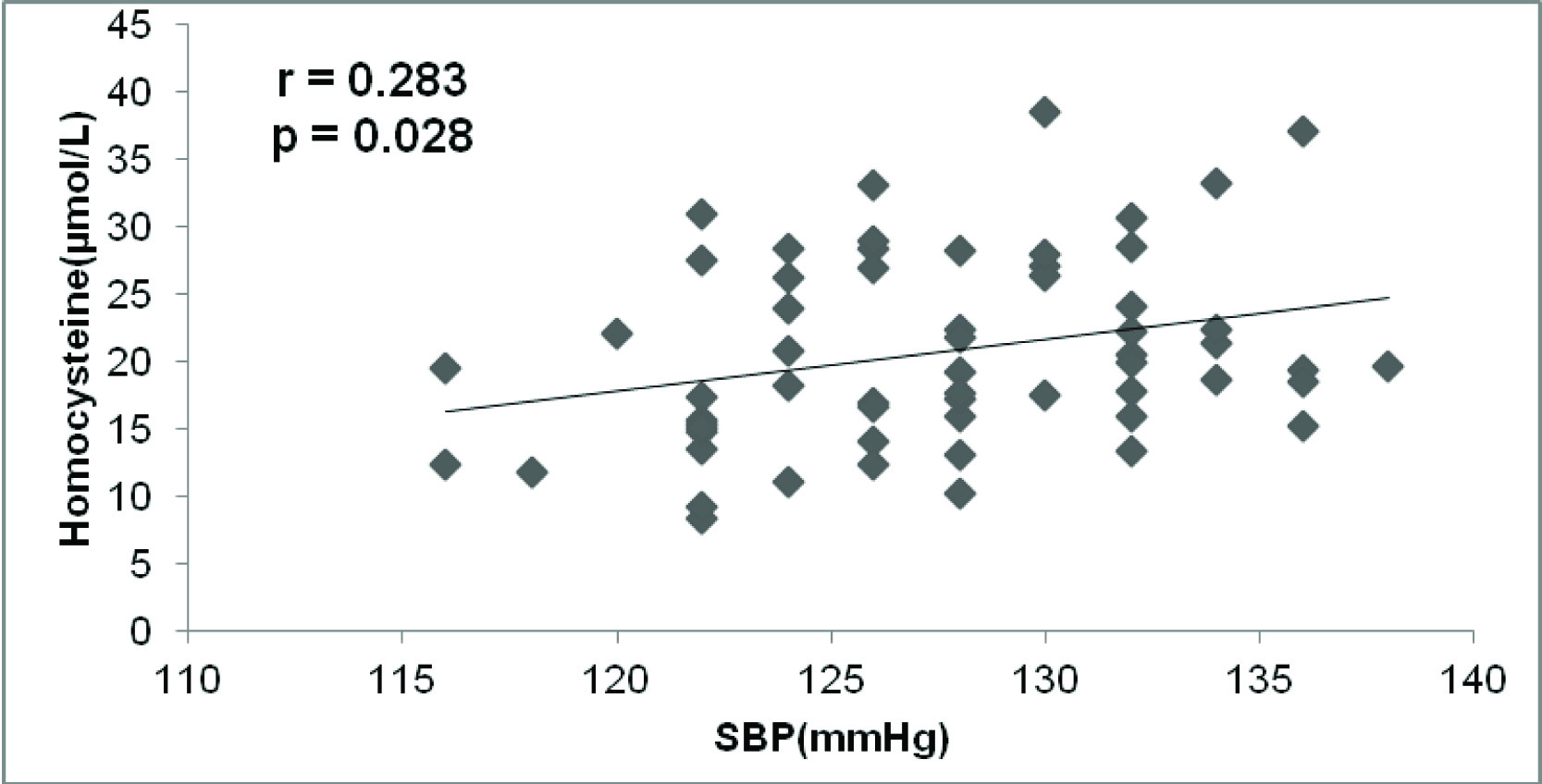
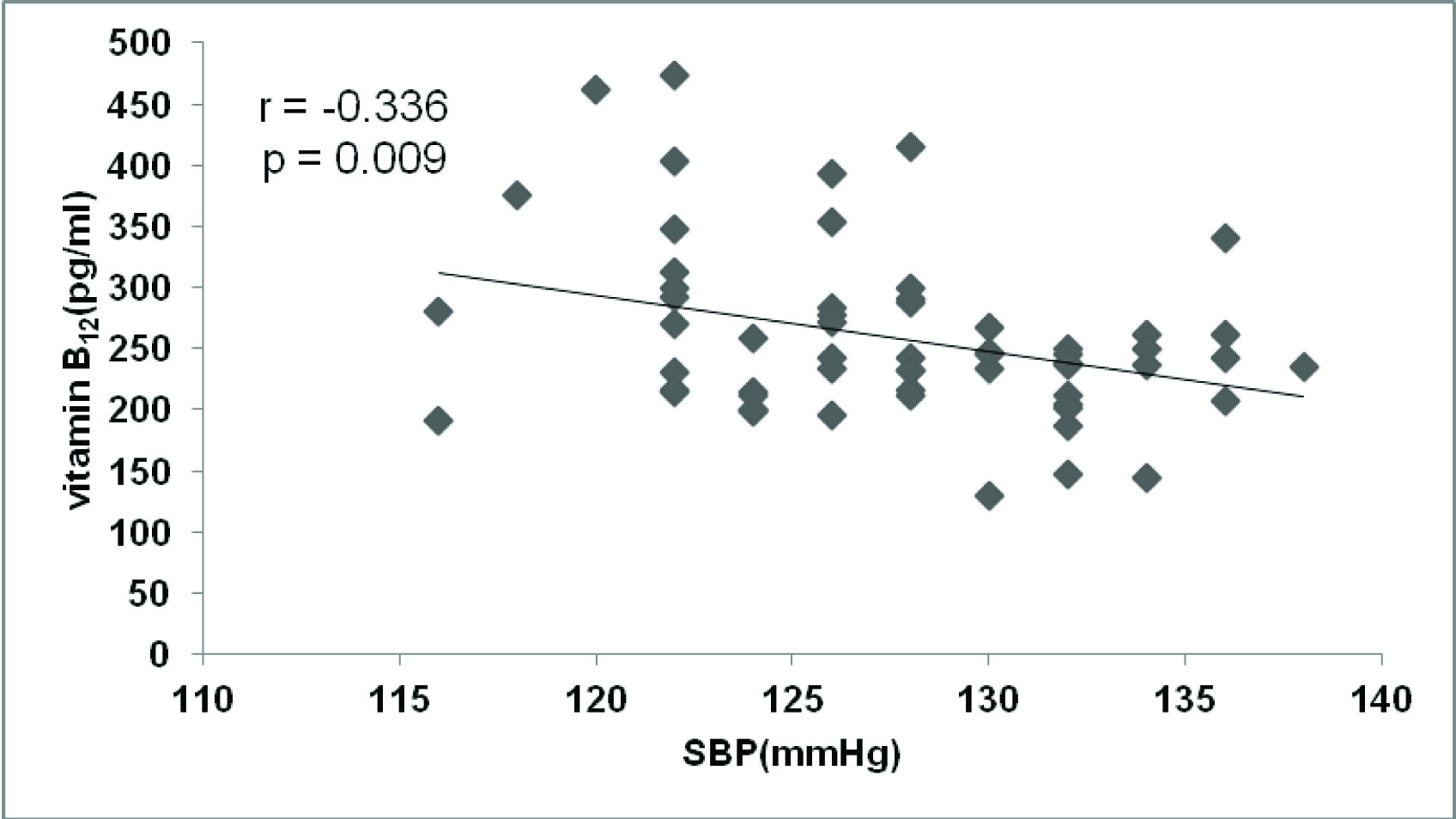
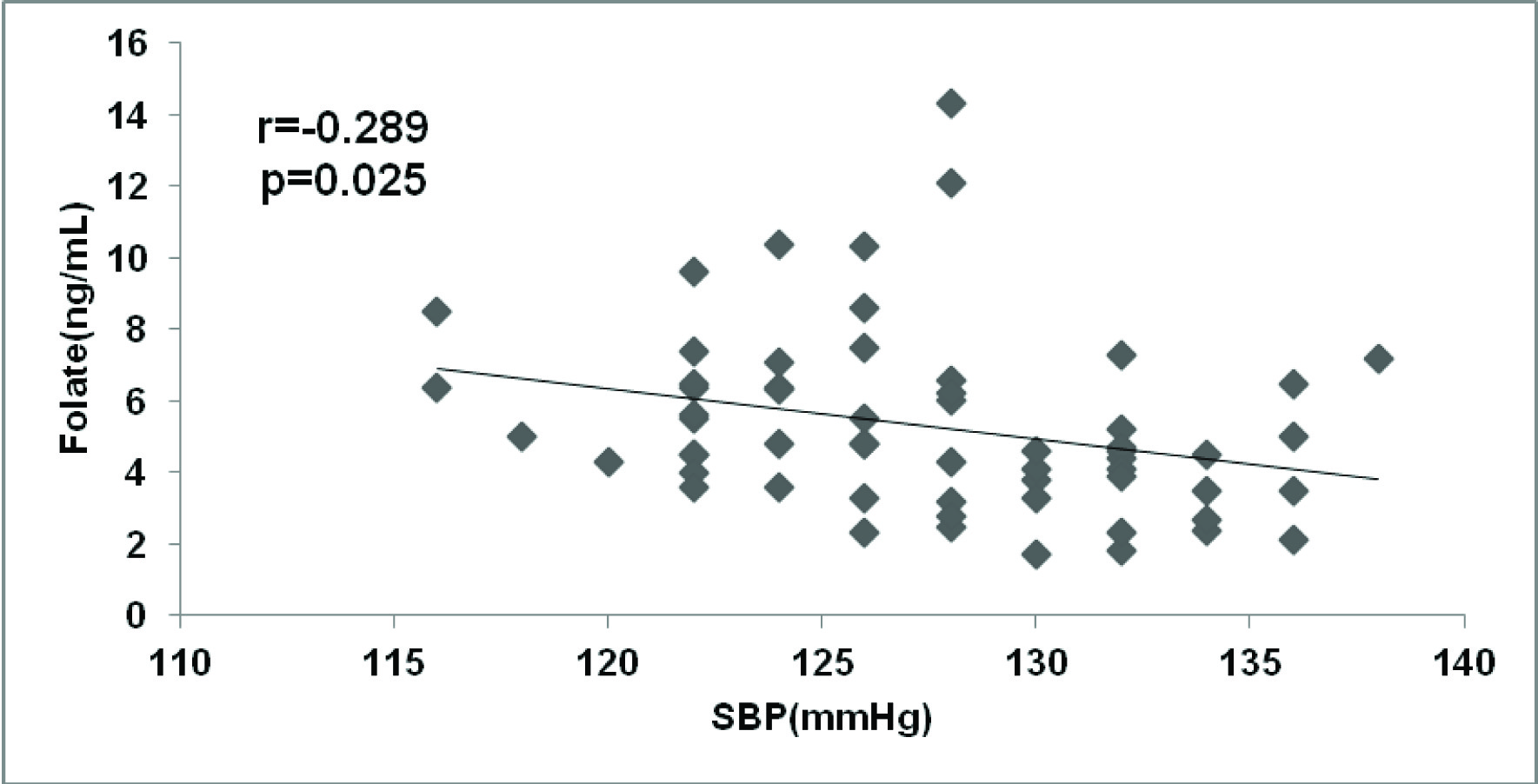
When correlation analysis was carried out, we found positive correlation of serum homocysteine and negative correlation of vitamin B12 and folate with systolic blood pressure [Table/Fig-4,5 and 6].
Correlation analysis between serum homocysteine and systolic blood pressure in subjects with prehypertension (n=60)
Correlation analysis between serum vitamin B12 and systolic Blood pressure in subjects with prehypertension (n=60)
Correlation analysis between serum folate and Systolic Blood pressure in subjects with prehypertension (n=60)
Discussion
Several investigators have demonstrated that the presence of predictive risk factors like hyperhomocysteinemia, insulin resistance, dyslipidemia and inflammation and its influence on the clinical occurrence of cardiovascular disease in subjects with elevated blood pressure [4,6].
In the present study, homocysteine was significantly elevated in prehypertensive subjects when compared to subjects with normal blood pressure, whereas vitamin B12 and folate levels were not altered.
Also there was significant association between homocysteine, folate and vitamin B12 with systolic blood pressure in the prehypertension group. Increased serum homocysteine and its association with Systolic Blood Pressure in our study is in accord with the study by Dinavahi R et al., who concluded the association of homocysteine with systolic and diastolic blood pressure in young African American women [8]. Thus, increase in homocysteine may lead to development of hypertension by increasing arterial stiffness or through oxidative stress induced endothelial dysfunction [9,10]. These findings were consistent with a previous study by Chrysohoou C et al.,[5].
C-reactive protein, an acute phase protein and marker of low grade systemic inflammation predicts cardiovascular mortality and morbidity in patients with pre-existing CVD and in apparently healthy subjects [11]. It has been postulated that increased level of hs-CRP precedes elevation in blood pressure [6]. Tanaka F et al., have documented that hs-CRP can be used as a marker for short-term risk of ischemic stroke among prehypertensive subjects [12]. In the current study hs-CRP levels were significantly increased in subjects with prehypertension. These findings were in accordance with previous studies by Saxena et al., [13] and Sathiyapriya et al.,[14].
A report by Sabanayagam C et al., [15] from two independent population based studies; the Singapore Prospective Study Programme (SP2) and the Singapore Malay Eye Study (SiMES) concluded that C- reactive protein is associated with prehypertension. This report supports our study. It has been hypothesised that higher levels of C-reactive protein may increase blood pressure by reducing nitric oxide production in endothelial cells, resulting in vasoconstriction and increased production of endothelin 1[14,16].
Insulin resistance is considered as a hall mark of several disorders including hypertension. A study by Sathiyapriya et al.,[17] has reported insulin resistance and hyperinsulinemia in prehypertension. In the present study insulin and insulin resistance were significantly increased in prehypertensive subjects compared to subjects with normal blood pressure. This finding is supported by Zhoa et al., who demonstrated that prehypertension is associated insulin resistance and suggested that it increases the risk for the development of hypertension [18]. The study by HWU et al., is also in agreement with our finding [19].
Insulin resistance is associated with dyslipidemia. In the current study total cholesterol, VLDL-C and LDL-C were significantly increased in prehypertensive subjects when compared to controls. This is in similar to the report by Nah and Kim who found increase in cholesterol and LDL-C [20]. It has been suggested that insulin resistance and/or subsequent hyperinsulinemia can elevate blood pressure by enhancing sympathetic nervous system activity and inducing vascular smooth muscle cell hypertrophy [17].
Conclusion
Hyperhomocystein- emia, insulin resistance and elevated hs-CRP levels are associated with prehypertension and may enhance cardiovascular risk in these subjects. Further studies are needed to investigate whether life-style modifications have any effect on reducing homocysteine, insulin resistance and hs CRP levels in subjects with prehypertension.
Limitations
Smaller sample size was one of the limitations of the study. The diet history of the subjects was not recorded, which may influence the vitamin B12 and folate concentrations which in turn affect the homocysteine level. And follow up was not done to evaluate what percent of pre-hypertensive subjects developed hypertension or other cardiovascular complications.
Values are expressed as mean±SD, NS-Not significant. SBP-systolic Blood pressure,DBP-Diastolic Blood pressure
Values are expressed as mean±SD, NS-Not significant
Values are expressed as mean±SD, NS-Not significant