The Role of Nasendoscopy in the Fabrication of a Palatopharyngeal Obturator – A Case Report
Bhavya M. Amin1, Meena A. Aras2, Vidya Chitre3, Praveen Rajagopal4
1Student,Goa Dental College and Hospital, Bambolim, Goa, India.
2Professor and Head, Department of Prosthodontics,Goa Dental College and Hospital, Bambolim, Goa, India.
3Professor, Department of Prosthodontics,Goa Dental College and Hospital, Bambolim, Goa, India.
4Assistant Professor, Department of Prosthodontics,Goa Dental College and Hospital, Bambolim, Goa, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bhavya M. Amin, Goa Dental College and Hospital, Bambolim – Goa -403002, India.
Phone: +919765950649,
E-mail: bhavya_amin@rediffmail.com
Defects confined to the hard palate can be managed with relative ease because it is a static shelf creating oro- nasal separation. Since the soft palate is a dynamic separator between the oral and nasal cavities, defects involving the soft palate require careful consideration. Instrumental visualization methods can aid the fabrication of obturators in patients with such defects and prevent problems of under or over obturation. This case report presents the prosthodontic management of a patient with a Veau class II cleft palate using a palatopharyngeal obturator in order to re-establish normal functions of deglutition and speech. Nasendoscopy was used as an adjunctive procedure to assess velopharyngeal function with the prosthesis.
Cleft palate, Nasendoscopy, Palatopharyngeal obturator
Case Report
A 43-year-old patient reported to the Department of Goa Dental College and Hospital with a chief complaint of difficulty in swallowing and speaking due to a defect in the roof of her mouth. Her speech was hypernasal, accompanied by facial grimacing and she complained of discharge through the nose while coughing. The patient mentioned having undergone a surgical procedure in childhood for repair of the defect; the details of which were unknown. She was also given obturator prosthesis 20y back. Due to extraction of carious teeth over the preceding 10 months of reporting to the department, the prosthesis lost retention and could not be worn.
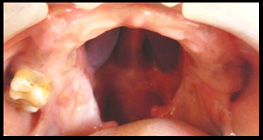
Intraoral examination revealed a Veau class II cleft palate, with the presence of maxillary right second and third molars and a partially edentulous mandibular arch [Table/Fig-1]. The patient was given the choice of an implant supported prosthesis which she refused due to economic reasons. It was hence decided to fabricate a palatopharyngeal obturator supported by a cast framework and an acrylic removable partial denture for the mandibular arch.
The conventional procedures of obturator fabrication were followed which involved making primary alginate impression, border moulding and secondary impression. With the impression in place, the patient was asked to swallow water to ensure that a seal was obtained and nasal regurgitation did not occur. The patient was also asked to say the word ‘beat’ with nares open and closed since it is a sound produced using the oral cavity as a primary resonating chamber. No change in the sound indicated that there was no air escape through the nose [1]. A metal framework was constructed with direct retainers on the maxillary second and third molars, meshwork Sectionon the ridge area, complete metal coverage on the palatal aspect and struts extending posteriorly to retain the acrylic bulb. After trial of the framework, a heat cured acrylic resin record base was fabricated over it. The bulb was hollowed out using the lost salt technique [2], thereby lightening the prosthesis and increasing its retention. The record base was tried intraorally and adjustments were done using pressure indicating paste. Jaw relations and try in were carried out in a conventional manner. The obturator prosthesis and mandibular partial denture were then acrylised and delivered to the patient. The ability to swallow without regurgitation, unimpeded breathing, comfort and improvement in speech was assessed. Speech improvement was not discernable. Further, the patient experienced mild discomfort in breathing and a gagging sensation probably due to increased posterior extent of the obturator in comparison to her previous obturator prosthesis. Due to the inability to determine pharyngeal wall movement by direct oral observation, it was decided to use a three dimensional visualization method that could help in obturator revision.
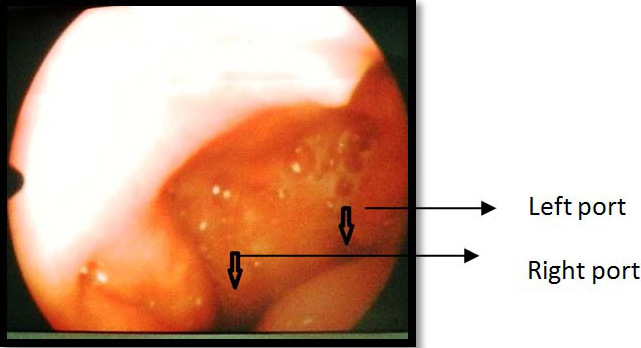
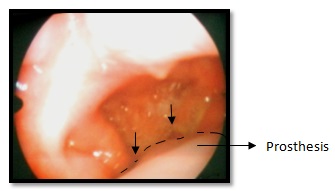
Nasal endoscopic evaluation was chosen as a visual aid to verify proper soft tissue-obturator contact during speech and swallowing and revise and areas of under or over obturation, if required. After explaining the procedure to the patient and obtaining her consent, the evaluation was carried out. A fiberoptic nasal endoscope of 3mm diameter, equipped with a camera, (Karl Storz Gmbh & Co, Germany) was used to evaluate velopharyngeal functioning. The nasal cavities were packed with gauze soaked in topical anaesthetic (4% xylocaine) for 10min prior to the procedure. After removal of the gauze, the flexible endoscope was inserted transnasally and its movement was guided by the examiner viewing the image through the scope. The moveable tip was angled and rotated so that at rest the velopharynx was in full view. The velopharyngeal port was observed during quiet breathing, swallowing and speech. The patient was asked to repeat sentences with pressure loaded consonants (‘Buy baby a bib’, ‘cherries and cheese’) and count from 60 to 69 to assess the velopharyngeal port during speech since these sounds show maximum velopharyngeal movement[3,4]. Through the examination it was apparent that there were patent portals to the right and left of the prosthesis during respiration [Table/Fig-2]; while during swallowing and speech, the obturator made contact with the lateral and posterior pharyngeal walls [Table/Fig-3]. The lateral walls showed active mesial movement when closing against the obturator. The portal towards the left pharyngeal wall was constricted compared to the right portal. The left lateral aspect of the obturator was relieved by few millimeters to create a wider portal and allow comfortable breathing. It was also decided in consultation with the ENT surgeon to reduce the posterior extent of the obturator by a few millimeters to prevent impingement of the obturator on the active pharyngeal walls during swallowing and eliminate the gagging sensation experienced by the patient [Table/Fig-4a-4b]. This objective assessment prevented unnecessary adjustments based on a subjective evaluation of the obturator which could lead to hypernasality due to underobturation. After the necessary modifications, the prosthesis was delivered to the patient [Table/Fig-5] and the services of a speech therapist were sought to improve the speech of the patient.
Discussion
Prosthetic rehabilitation of soft palate defects has traditionally relied on functional contouring of a prosthesis using functionally adapted impression materials. However, there are limitations to this process, particularly in its inability to visualize function as it relates to the prosthesis in a three-dimensional space [4]. It may be difficult to assess the effectiveness of the obturator by perceptual speech evaluation alone since most cleft palate patients do not have developed speech patterns, making it improbable that normal speech will be restored immediately with adequate obturation. The patient may acquire the ability to control nasal air emission and can restore resonance balance, but articulatory disorders may remain [1]. Hence a more objective evaluation that can provide direct visualization of the velopharyngeal sphincter and provide biofeedback is necessary.
Nasendoscopy is one such procedure that can contribute to the diagnostic process, providing information about the function and status of the velopharynx before, during and after treatment. It allows a detailed observation of the velopharynx and helps determine areas of under or over obturation, which can be modified as required. This reduces the number and length of sessions required to complete the prosthesis [4-6]. Though this procedure requires the additional supervision of an ENT specialist, it has the advantages of being easily tolerated by the patient, not requiring radiation as in fluoroscopic techniques and does not cause an interference with speech as in oral endoscopy [3,7-9]. In this case, the use of nasendoscopy was justified to ensure proper soft tissue – obturator contact.
Riski et al.,[6] described the use of nasal endoscopy in two cases for viewing the velopharyngeal port in order to determine the site at which the obturator should be increased or relieved. In both the cases, aerodynamic measures and nasal enodoscopic evaluation was used to reveal gaps between the obturator and pharyngeal walls during speech or to determine active movement of the pharyngeal walls against the obturator. In the first case, the gap seen between the obturator and lateral pharyngeal wall were closed using thermoplastic material which was moulded by production of pressure loaded consonants and swallowing; while active movement of the pharyngeal wall seen in the second case indicated relief of lateral walls of the obturator with simultaneous nasendoscopic evaluation.
Lam et al., [8] conducted a comparative study of nasendoscopy and multiview fluoroscopy in assessing velopharyngeal gap size and determining the relationship between these assessments and velopharyngeal insufficiency severity 177 subjects and concluded that both nasendoscopy and multiview videofluoroscopy assessments provide complementary information and are correlated. However, the “bird’s-eye view” provided by nasendoscopy has a stronger correlation with insufficiency severity than multi view videofluoroscopy.
Patent portals to the right and left of the prosthesis while breathing
Contact of the obturator with the pharyngeal walls on swallowing
Pharyngeal extent of obturator before nasal endoscopy

Pharyngeal extent of obturator after nasal endoscopic evaluation

Post operative view obturator following nasal endoscopy

Conclusion
The fabrication of an obturator and its success can be hampered by improper evaluation of the velopharyngeal dimensions and dynamics. Underobturation would lead to nasal reflux and hypernasality while overobturation causes hyponasal speech, tissue ulcerations and discomfort to the patient. Nasendoscopy, as a complementary tool in rehabilitation of velopharyngeal deficits, can greatly aid the clinician and improve the functional outcome.
[1]. J Beumer, TA Curtis, MT Marunick, Maxillofacial Rehabilitation: Prosthodontic and Surgical Considerations; Speech, Velopharyngeal Function, and Restoration of Soft Palate Defects.Ishiyaku Euro America, Inc; 1996 2nd EditionSt. Louis [Google Scholar]
[2]. H Aggarwal, SK Jurel, RD Singh, P Chand, P Kumar, Lost salt technique for severely resorbed alveolar ridges: An innovative approach.Contemp Clin Dent. 2012 3(3):352-55. [Google Scholar]
[3]. RJ Shprintzen, E Marrinan, Velopharyngeal insufficiency: diagnosis and management.Curr Opin Otolaryngol Head Neck Surg. 2009 17(4):302-07. [Google Scholar]
[4]. A Shyammohan, D Sreenivasulu, Speech Therapy with Obturator.J Indian Prosthodont Soc. 2010 10(4):197-99. [Google Scholar]
[5]. JM Rieger, JG Zalmanowitz, JF Wolfaardt, Nasopharyngoscopy in palatopharyngeal prosthetic rehabilitation: A preliminary report.Int J Prosthodont. 2006 19(4):383-88. [Google Scholar]
[6]. JE Riski, JA Hoke, EA Dolan, The role of pressure flow and endoscopic assessment in successful palatal obturator revision. Cleft Palate Journal. 1989 26(1):56-62. [Google Scholar]
[7]. VL Siegel – Sadewitz, RJ Shprintzen, Nasopharyngoscopy of the normal velopharyngeal sphincter: An experiment of biofeedback.Cleft Palate Journal. 1982 19(3):194-200. [Google Scholar]
[8]. DJ Lam, JR Starr, JA Perkins, CW Lewis, LE Eblen, J Dunlap, A Comparison of Nasendoscopy and Multiview Videofluoroscopy in Assessing Velopharyngeal Insufficiency.Otolaryngology–Head and Neck Surgery. 2006 134(3):394-402. [Google Scholar]
[9]. HE Turner, WN Williams, J Pinkham, Fluoroscopy and nasoendoscopy in designing palatal lift prostheses.J Prosthet Dent. 1991 66:63-71. [Google Scholar]