Multiple and Contemporary Coronary Thrombosis inspite of Low Platelet Function Response
Rocco Edoardo Stio1, Simone Calcagno2, Luigi Lucisano3, Mauro Pennacchi4, Gennaro Sardella5
1 Faculty, Department of Cardiovascular, Respiratory and Morphologic Sciences, Policlinico Umberto I, “Sapienza” University of Rome, Italy.
2 Faculty, Department of Cardiovascular, Respiratory and Morphologic Sciences, Policlinico Umberto I, “Sapienza” University of Rome, Italy.
3 Faculty, Department of Cardiovascular, Respiratory and Morphologic Sciences, Policlinico Umberto I, “Sapienza” University of Rome, Italy.
4 Faculty, Department of Cardiovascular, Respiratory and Morphologic Sciences, Policlinico Umberto I, “Sapienza” University of Rome, Italy.
5 Faculty, Department of Cardiovascular, Respiratory and Morphologic Sciences, Policlinico Umberto I, “Sapienza” University of Rome, Italy.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rocco Edoardo Stio, Viale del Policlinico 155, 00161 Rome, Italy.
Phone: +393920973677,
E-mail: rocco.stio@libero.it
We are reporting a clinical case of a 78-year-old male who had oppressive chest pain at rest, which regressed with the intake of sublingual nitrates. Coronary angiography showed a chronic total occlusion (CTO) of the left anterior descending (LAD) artery, a normal circumflex, a hypoplasic right coronary artery and a Cardiac Magnetic Resonance showing vital tissue in anterior wall. During the procedure of CTO-PCI on LAD, patient developed multiple and contemporary coronary thrombosis in spite of low platelet reactivity, which was assessed by using Multiplate. A manual thrombectomy was performed with a good final result only after drug eluting stents (DES) implantation.
Complications adult cath/intervention, Thrombectomy, Aggregometry
Case Report
A 78-year-old male, an ex-smoker, who had arterial systemic hypertension, hypercholesterolaemia as cardiovascular risk factors and recent necrotic haemorragic pancreatitis which was complicated by septic shock and an episode of ulcerative colitis, he was admitted in our Hospital. He experienced oppressive chest pain at rest which regressed with the intake of sublingual nitrates. The ECG at admission showed an aspecific alteration in antero-lateral leads and the stress test confirmed an ST segment depression in V1-V4, at the top. Echocardiogram showed antero-septal ipokinesia (EF 35%). The patient who was pretreated with Clopidogrel (300mg) and aspirin (100mg), underwent a coronary angiography [Table/Fig-1A] that showed a chronic total occlusion (CTO) of the left anterior descending (LAD) artery, a normal circumflex (LCX) and an hypoplasic right coronary artery (RCA). To better address CTO procedure, a Cardiac Magnetic Resonance was performed, which showed vital tissue in anterior wall. After 5 days, the procedure of CTO-PCI on LAD was attempted. The patient platelet function before the procedure was assessed by using Multiplate analyzer (Dynabyte, Munich, Germany) [Table/Fig-1B], that had shown a good response to antiplatelet agents (ADP test 130 AUC, ASP test 90 AUC, TRAP test 80 AUC).
Panel A: left coronary angiography. Panel B: Multiplate assessment. Panel C: Thrombus formation in proximal LAD. Panel D: Thrombus formation in distal LCX with ventricular fibrillation treated with DC-shock. Panel E: Thrombus formation in ostial LAD with ST elevation on the ECG. Panel F. Final PCI result
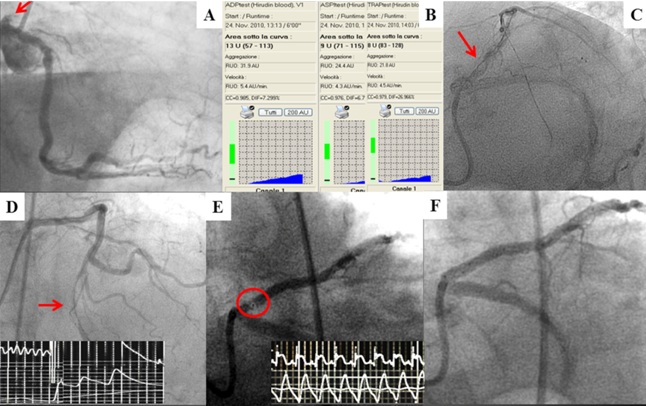
By gaining right femoral artery access, a guiding catheter (7 French, Amplatz L-1) was inserted into the left coronary artery and 5,000 units of heparin had been administered. A stiff wire was difficulty advanced distally in the LAD and multiple dilatations were performed using different sizes balloons. A following angiogram showed a partial vessel recanalization with a first thrombus formation in proximal LAD [Table/Fig-1C] and immediately, a manual thrombectomy, with use of micro-catheter 6 French, was performed, with white cloth extraction. At the same time, a spontaneous LCX occlusion occurred, with a contemporary ventricular fibrillation, which was treated with DC-shock [Table/Fig-1D]. Immediately, a wire was placed in distal segment of LCX and an intra-coronary infusion of abciximab bolus was administrated, with vessel recanalization and residual stenosis. A drug eluting stent was rapidly implanted there, with successful recanalization of LCX and a good distal flow. We continued the LAD PCI with DES implantation and a third thrombosis was observed in ostial LAD, with ST segment elevation [Table/Fig-1E]. A manual thrombectomy was still performed, without cloth extraction and finally, one DES in left main-LAD was implanted with an optimal final result [Table/Fig-1F]. Furthermore, to predict a clinical improvement, we decided to switch the antiplatelet therapy to Ticagrelor, obtaining a good AUC reduction as compared to Clopidogrel therapy results.
Discussion
Dual antiplatelet therapy, aspirin and a thienopyridine, reduces ischaemic cardiovascular events which follow percutaneous coronary interventions. However, despite this treatment, a residual risk of ischaemic events persists. Among other factors, enhanced platelet reactivity seen after giving thienopyridine therapy is associated with an increased risk of ischaemic cardiovascular events. A heterogeneous and variable patient response to Clopidogrel, which is attributed to a number of genetic, pharmacologic, and clinical factors, exists and novel P2Y12 antagonists can provide a normal response in terms of platelet aggregation [1] , with consequent greater ischaemic reductions [2,3]. Clinical use of platelet function tests is now possible with the development of user-friendly assays that do not require substantial technical training [4] and the prognostic value of point-of-care testing in patients with acute coronary syndrome (ACS) and those receiving coronary stents has been demonstrated in several prospective registries and trials which involve several thousands of patients [5,6]. Unfortunately, despite treatment with Clopidogrel, some patients continue to have cardiovascular events. This may be caused by a suboptimal response to the drug, with minimal inhibition of platelet aggregation or a high on-treatment platelet reactivity. Developments made in point-of-care platelet function testing allow the assessment of on-treatment platelet reactivity after giving thienopyridine therapy and thus, identification of poor responders.
A multiple contemporary thrombosis is a rare event in particular, in stable patients with low platelet reactivity; the occurrence of this event in spite of the low platelet reactivity, should be better investigated, as it gives rise to some concern about the significance of aggregometry response.
As it is well known, the prothrombotic statement, during percutaneous coronary interventions, can create thrombotic formations in coronary artery, probably due to guidewire advancement or due to balloon inflations. In fact, during the dilatations of the plaques, there is iatrogenic breaking-off of the fibrous cap, with consequent exposition of the lipid core. These events frequently occur in the target vessel, while they are rarer in non target vessel and are even more unusual if they are contemporary. Moreover, platelet function testing effectively identifies patients with high on treatment platelet reactivity (HTPR). Otherwise, its main drawback is its poor reproducibility and this creates many doubts in the interpretation of results.
Furthermore, we finally decided to change the antiplatelet therapy to Ticagrelor, despite the patient responding to the therapy with Clopidogrel, to reduce his ischaemic risk. The RESPOND trial [7] showed that Ticagrelor therapy overcame the non-responsiveness to Clopidogrel, and its antiplatelet effect was found to be the same in responders and non-responders. Nearly all Clopidogrel non-responders and responders who were treated with ticagrelor had platelet reactivities which were below the cut points which were associated with ischaemic risk. In addition, they found that switching from Clopidogrel to Ticagrelor not only overcame Clopidogrel non-responsiveness (mean increase in IPA of ≈40% in non-responders), but that it also provided additional platelet inhibitionin Clopidogrel responders (≈20% increase in IPA). Furthermore, the PLATO study [3] showed that treatment with Ticagrelor, as compared to that with Clopidogrel, in patients with acute coronary syndromes, significantly reduced the rate of death which occurred from vascular causes, myocardial infarction, or stroke, without a significant increase in the rate of major bleeding.
Conclusion
A multiple contemporary thrombosis is a rare event which develops during PCI, in particular, in stable patients. The occurrence of this event, in spite of a low platelet function, should be better investigated and it leaves many doubts about the significance of aggregometry use and its reproducibility. In our case, the multiple thrombosis occurred, probably, due to guidewire advancement, that had fractured the plaque.
[1]. Sardella G, Calcagno S, Mancone M, Palmirotta R, Lucisano L, Canali E, Pharmacodynamic Effect of Switching Therapy in Patients With High On-Treatment Platelet Reactivity and Genotype Variation With High Clopidogrel Dose Versus Prasugrel: The RESET GENE TrialCirc Cardiovasc Interv 2012 (5):698-704. [Google Scholar]
[2]. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromesN Engl J Med 2007 (357):2001-15. [Google Scholar]
[3]. Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Ticagrelor versus clopidogrel in patients with acute coronary syndromesN Engl J Med 2009 (361):1045-57. [Google Scholar]
[4]. Price MJ, Bedside evaluation of thienopyridine antiplatelet therapyCirculation 2009 (119):2625-32. [Google Scholar]
[5]. Brar SS, ten Berg J, Marcucci R, Price MJ, Valgimigli M, Kim HS, Impact of clopidogrel on-treatment platelet reactivity on stent thrombosis after percutaneous coronary intervention: results from a collaborative metaanalysis of individual participant dataJ Am Coll Cardiol 2011 58(19):1945-54. [Google Scholar]
[6]. Price MJ, Angiolillo DJ, Teirstein PS, Lillie E, Manoukian SV, Berger PB, Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention: a time-dependent analysis of the Gauging Responsiveness With a VerifyNow P2Y12 Assay: Impact on Thrombosis and Safety (GRAVITAS) TrialCirculation 2011 (124):1132-37. [Google Scholar]
[7]. Gurbel PA, Bliden KP, Butler K, Antonino MJ, Wei C, Teng R, Response to Ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: the RESPOND studyCirculation 2010 (121):1188-99. [Google Scholar]