Aesthetic Essentiality Regained Using Implant- A Case Report
B. Eswaran1, Rathika Rai2, Suprabha Rathee3, Babina Chirom4, Menaga V5
1 Senior Lecturer, Department of Prosthodontics, Thai Moogambigai Dental College and Hospital, Chennai, India.
2 Professor and HOD, Department of Prosthodontics, Thai Moogambigai Dental College and Hospital, Chennai, India.
3 Senior Lecturer, Department of Prosthodontics, Thai Moogambigai Dental College and Hospital, Chennai, India.
4 Post graduate student, Department of Prosthodontics, Thai Moogambigai Dental College and Hospital, Chennai, India.
5 Post graduate student, Department of Prosthodontics, Thai Moogambigai Dental College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. B.Eswaran, No. 20, Amirtha Illlam, Mohammed Hussain Colony, 3rd street, Kolathore, Chennai-600099, India.
Phone: 9841013245,
E-mail: dr.ashock@yahoo.co.in
The goal of implant therapy is to provide patients with a predictable, aesthetically and functionally satisfying treatment outcome with a low risk of aesthetic complications. Dental implants have been utilized by mankind for thousands of years, but only recently they have achieved widespread acceptance from the profession. Anterior sites are more likely related to aesthetic expectations and often represent a considerable challenge for involved clinicians and dental technicians, since various local risk factors have the potential to compromise the predictability of the result. In recent years, substantial efforts have been made to increase the appeal of implant therapy by shortening the overall treatment time and minimizing the number of surgical intervention. According to traditional protocol, a 12 month healing after extraction was suggested, but over the past few years alternative approaches have been proposed, such as immediate implant placement at the time of extraction or early implant placement following weeks of soft tissue healing. Common to all of these approaches is the requirement of adequate remaining bone volume. If there is no adequate bone volume, techniques like guided bone regeneration (GBR) are used for ridge augmentation before implant placement. The present case has utilized an endosteal root form implant and the advantage of guided bone regeneration technique in regaining aesthetic demands of the patient.
Autograft, Esthetics, Endosseous implants, Essix appliance, Guided bone regeneration (GBR), Guided tissue regeneration (GTR)
Case Report
A 16-year-old female patient was referred to the clinic for the management of complications due to missing 21[Table/Fig-1]. Periapical radiograph was taken to evaluate the closeness of permanent central incisor in that region. Intraoral periapical radiograph revealed the presence of an impacted supernumerary tooth and an impacted permanent central incisor above it [Table/Fig-2]. Diagnostic impressions were made using irreversible hydrocolloid (Alginate) and study models were obtained on the first appointment. Treatment plan was discussed and decided after consulting with an orthodontist and an oral surgeon. Orthodontic extrusion of the permanent incisor was merely impossible. It was planned that the supernumerary and the permanent central incisor would be extracted and the defect will be filled with bone grafts and covered using a resorbable membrane. After a period of three months an endosseous root form implant was planned to be placed at the extracted site and decided to be restored with a crown after healing period of six months.
Preoperative photograph showing missing 21

Periapical radiograph of the 21 region showing impacted supernumarary tooth and permenant central incisor

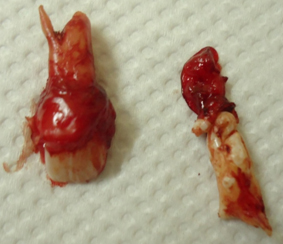
During second surgical appointment extraction procedures were carried out under local anaesthesia (Lignox2%with adrenalin 1:80000;INDOCO REMEDIES LTD). Infiltration anaesthesia was given in relation to 11,21,22 region. A crestal incision was given in the region of 21 and releasing incision in the labial mucosa on the distal aspect of 11and 22. A full thickness mucoperiosteal flap was reflected. The reflected buccal flap was sutured to the inner (non-keratinized) portion of the upper lip and left till the extraction procedures were completed. A 6x10 mm of the exposed buccal cortical bone in relation to the supernumerary teeth was removed as a single segment, using slow speed handpiece with copious amount of saline irrigation. The segment was stored in saline. After exposure of supernumerary teeth, it was luxated using periotomes and extraction of the tooth was done [Table/Fig-3]. Care was taken that the palatal bone remained intact. The impacted permanent tooth was luxated using periotomes and was carefully extracted using anterior extraction forceps, holding the exposed crown mesiodistally [Table/Fig-4,5]. The defect in the extracted site was planned to be filled with Osseograft/DMBM (Demineralized Bone Matrix) [Advanced Biotech Products Limited, Chennai, India.], a bone regeneration material. The bone grafts were mixed with crushed buccal segment which was stored, and then placed in the region of bone defect. The mixture of crushed autologous bone graft and bone regeneration material was placed only in relation to the defect created by extracted supernumerary tooth [Table/Fig-6]. Then these bone materials were covered with Sterile Bioresorbable Collagen Membrane for Guided Tissue Regeneration (GTR) [Advanced Biotech Products Limited, Chennai, India.], [Table/Fig-7]. After placement of the resorbable membrane, the mucoperiosteal buccal flap was approximated with the palatal mucoperiosteal tissues and interrupted mattress sutures were placed. An Essix appliance was given to the patient on the same day of surgery [Table/Fig-8]. Antibiotics and analgesics were prescribed for five days.
Photograph showing the defect after extraction of supernumerary tooth

Photograph showing the defect after extraction of permanent central incisor

Extracted central incisor and supernumaray tooth
Photograph showing placement of bone graft material in the defect site.

Photograph showing placement of bioresorbable membrane

Essix appliance with provisional acrylic teeth in the patient mouth.

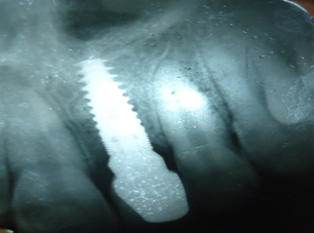
A radiographic evaluation of the surgical site was done after three months. It was planned that the implant would be placed at this time, but would be loaded only after an additional healing period of three months (six months of healing period). The width of the implant to be placed was determined using bone mapping on the sectioned cast of the patient [Table/Fig-9] and the length evaluation was done using the patient’s OPG. An implant of 3.75x11.50mm (ADIN)was selected. The implant placement was done under LA. A crestal incision was given at the implant site (21 region) and full thickness mucoperiosteal flap was reflected and sequential drilling of bone was done using surgical drills. The predetermined implant was wrenched into the place and primary stability of the implant was measured using torque wrench which was close to 30 Ncm. Cover screw was placed [Table/Fig-10], reflected flaps were approximated using sutures and a new Essix appliance was given. Patient was under antibiotics and analgesics for next three days. Implant was planned to be loaded after three months, so that the surgical site would acquire sufficient bone density. Three months after implant placement the presence of healthy soft tissue covering the implant was clinically confirmed. Also peri-implant bone evaluation was done using a radiograph [Table/Fig-11]. After a healing period of six months the implant was exposed,cover screw removed and healing abutment was placed. Patient was recalled after a week and gingival contour was evaluated. An implant level impression was made, and a crown was fabricated and cemented. Review of the patient was done on 2nd week, and after two months. Clinical evaluation of the soft tissue and radiographic evaluation was also done to asses bone level at the implant site after a year [Table/Fig-12] and the results were satisfactory [Table/Fig-13].
Bone mapping done to determine available width of the bone at the surgical site

Placement of endosseous root form implant in 21 region

Periapical radiograph taken three months after implant placement

Periapical radiograph taken after one year showing the bone level around the implant
Post operative photograph after a year

Discussion
Anterior tooth loss often compromises ideal bone volume in the aesthetic region. Reliable rehabilitation of the alveolar ridge with endosseous implants require proper quality and quantity of alveolar bone at the implant site, to achieve a sound long term results [1,2]. Immediate placement of an implant in the extraction socket is not always possible because of lack of bone. This region constitutes the most challenging part for the teeth replacement because of the role it plays on the aesthetics and phonetics. In the present case, immediate placement was not opted, as the defect which was produced after extraction was large enough to compromise primary stability of the implant. In an attempt to minimize the similar problem, various autogenic, allogenic or alloplastic bone substitutes have been proved successful [3–6].
Osseoinduction is the process where the presence of material promotes a bone healing response throughout the defined volume. The presence of bioactive framework or scaffold allows bone formation to be distributed more efficiently within the given space; in this case, an extraction site. Although the autografts are considered as gold standard for their optimal properties like osteogenecity, osteoinductivity and osteoconductivity, it is often impossible to harvest the neccessary amount of analogous bone blocks to reconstruct the extensive defects. The use of allografts and xenografts has been advocated to avoid these cited problems. Allografts have shown better results and lower resorption rate than xenografts and also have an additional advantage of unlimited availability, reduces patient discomfort by avoiding additional donor surgery site and time reduction [7–9]. In the present case, the allograft material was mixed with crushed fragmented autograft and was used to reconstruct the defect site, thus combining the advantageous properties of both the materials. Conversely, wound isolation by means of an occlusive membrane also was done to prevent the problem of soft tissue epithelial migration into the bone defects, favoring repopulation of the socket with cells with bone regenerating potential and leading to more complete bone fill. Isolation of underlying tissue may also concentrate growth factors and cellular elements necessary for healing [10,11]. In this case, the combination of bioresorbable membrane and osteoconductive bone grafts resulted complete bone fill at the implant site.
Provisional restoration was given using modified Essix thermoplastic co-polyester retainer on the same day of implant surgery [12]. An acrylic tooth was shaped to fit the missing tooth region on the cast of the patient. A 0.030inch of Essix plastic sheet is reduced to 0.015inch in thermoforming and was adapted over the acrylic teeth on the cast. After cooling, the adapted vaccuform sheet was trimmed from canine to canine and was tried in patient [13]. Provisionalisation by this method was comparatively easy than fabricating a removable appliance and it was of more comfort to the patient. As the patient had a deep bite, fibre reinforced resin composite Fixed Partial Denture was not suggested. The Essix appliance helped in maintaining the soft tissue contour in the 21 surgical site. It was comfortable and readily accepted by the patient. Plaque retention was seen during periodic visit, therefore good oral hygiene instructions were stressed.
After a healing period of six months, the entire site healed well, without apparent complications. The particulate mixture of allograft and autograft retained without loss in the extraction socket. The implant was exposed, cover screw was removed and the implant was checked for stability. The placed implant shows a good stability at an insertion torque of 45Ncm or greater. Healing abutment was placed and left for a week which helped in obtaining a gingival collar. The healing abutment was removed after a week and impression copings were attached and an implant level impression was made. The implant abutment was shaped according to the available space and was sent to the laboratory for fabrication of cement retained porcelain fused to metal crown. The crown was tried in patient’s mouth and was cemented using zinc oxide eugenol cement after patient’s acceptance. Time consumption for restoration can be attributed as one of the limitations in this case, yet aesthetic expectations of the patient was fulfilled using modified Essix appliance, hence overcoming the limitations to an extent.
Conclusion
One year follow up of this clinical case clearly demonstrates the success of graft material which was a mixture of autogenous and allogenous bone graft, in combination with resorbable membrane. Correspondingly, modified essix appliance can be tried as an easy alternative for provisionalisation and in regaining the patient’s aesthetics.
[1]. Sharma P, Anandakrishna GN, Kaur P, Dahiya V, Implant Esthetic Restoration in Ridge Deficiencies in Cases of Trauma: A Case ReportJ Oral Implantol 2013 5:621-24. [Google Scholar]
[2]. Alberktsson T, Johansson C, Osteoinduction, Osteoconduction and osseointegrationEuro Spine J 2001 10:S96-101. [Google Scholar]
[3]. Mc Allister BS, Haghighat K, Bone Augmentation TechniquesJ Peridontol 2007 78:377-96. [Google Scholar]
[4]. Villanueva-Alcojol Laura, Monje Floranico, Gonzalez-Garcia Raul, Moreno Carlos, Monje Alberto, Characteristics of newly formed bone in sockets augmented with cancellous porous bovine bone and a resorbable membrane; micro computed tomography, histologic, and resonance frequency analysisImplant Dent 2013 22(4):380-87. [Google Scholar]
[5]. Bartee BK, Extraction site reconstruction for alveolar ridge preservation. Part 2:Membrane assisted surgical techniqueJ Oral Implantol 2001 27:194-97. [Google Scholar]
[6]. Triplett RG, Schow SR, Autologous bone grafts and endosseous implants: complementary techniquesJ Oral Maxillofac Surg 1996 54:486-94. [Google Scholar]
[7]. Araujo Pryscyla P.T., Kerlison P, Oliveira, Sheyla C.L.Montenegro, Adriana F.P.Carreiro, Jose S.P.Silva, Adriano R.Germano. Block Allograft for Reconstruction of Alveolar Bone Ridge In Implantology: A Systemic ReviewImplant Dent 2013 22:304-08. [Google Scholar]
[8]. Menoni A, Bernardello F, Spinato S, Zaffe D, Full arch Vertical Reconstruction of an Extremely Atrophic Mandible With “Box Technique” A novel Surgical Procedure: A Clinical and Histologic Case ReportImplant Dent 2013 22:1-7. [Google Scholar]
[9]. Wallace Stephen C, Guided Bone Regeneration for Socket Preservation in Molar Extraction Sites:Histomorphic and 3D Computarized Tomography AnalysisJ Oral Implantol 2013 4:503-09. [Google Scholar]
[10]. Barboza EP, Stutz B, Ferreira VF, Guided bone regeneration using non expanded polytetrafluoroethylene membranes in preparation for dental implant placements.-A report of 420 casesImplant Dent 2010 19:2-7. [Google Scholar]
[11]. Lekovic V, Carmargo PM, Klokkevold PR, Preservation of Alveolar Bone in Extraction Sockets Using Bioabsorbable MembranesJ Periodontol 1998 69:1044-1049. [Google Scholar]
[12]. Kan Joseph Y. K., Rungcharassaeng K, Lozada J, Immediate Placement and Provisionalization of Maxillary Anterior Single Implants: 1-Year Prospective StudyMaxillofacial Implants 2003 18:31-39. [Google Scholar]
[13]. Blake M, Therese Gravey M, Fleming P, The use of an orthodontic thermoplastic retainer as a provisional anterior restoration: A case reportClinics in Dental practice 2003 1:27-30. [Google Scholar]