Pencillium keratitis in an Immunocompetent Patient from Pune, Maharashtra, India
Chanda Ratnakar Vyawahare1, Rabindra Nath Misra2, Nageswari Rajesh Gandham3, Kalpna Mohan Angadi4, Retina Paul5
1Assistant Professor, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune, India.
2HOD and Professor, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune, India.
3Professor, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune, India.
4Associate Professor, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune, India.
5Senior Resident, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chanda Ratnakar Vyawahare, Assistant Professor, Department of Microbiology, Pad.Dr.D.Y.Patil Medical College, Hospital and Research Center (DY Patil Vidyapeeth Pune) Pimpri, Pune-18, India.
Phone: 9503994493,
E-mail: Patilsv78@gmail.com
The incidence of fungal keratitis is less common than bacterial and viral keratitis. However, it remains a diagnostic and therapeutic challenge. Delayed clinical diagnosis is common mainly because of lack of suspicion. Further slow growth of fungus increases the time for confirmed laboratory diagnosis. After accurate diagnosis, patient’s management remains inadequate due to lack of availability of antifungal agents and its poor corneal penetration. Multitude of genera of molds and yeast have been identified in fungal keratitis. Due to their ubiquitous nature and easy isolation from the environment, their role in true pathogenesis is difficult to ascertain. Worldwide, incidence of fungal keratitis is rising at present. The predisposing factors comprises trauma, use of contact lenses and topical steroids. Filamentous fungi and dematiaceous fungi are the frequently encountered etiological agents of fungal keratitis. Dimorphic fungi are reported less frequently. Fungal keratitis tends to occur more frequently in young males and usually in winter and monsoon. Penicillium genera includes several species. By far Penicillium marneffei (P. marneffei) infection is most common, mainly associated with AIDS. A number of infections caused by species other than P. marneffei have been reported as well. Here we report a case of Penicillium keratitis in a young, HIV negative male farmer.
Penicillium keratitis, Fungal keratitis, Penicillium marneffei
Case Report
A 15-year-old boy, farmer by occupation, presented to the Out Patient Department of Paediatrics, Dr. D.Y. Patil Medical College hospital and research centre Pimpri-Pune Maharashtra, India on 9/8/2012 with complaints of diminished vision, opacity in the right eye and watering from the same eye for the last one year. Patient gave history of trauma to the right side of face including his right eye by rotating fan during the field work. He showed to local physician at village but he neither had the prescription nor was he able to tell the treatment he had taken. After this incidence patient suddenly developed the above symptoms. There was no history of any sticky discharge or photophobia, no history of diabetes mellitus (DM) and hypertension. Serodiagnosis for HIV and HBsAg were negative. Since the last 2 days, he developed severe pain and redness in the right eye[Table/Fig-1].
On ophthalmic examination, his vision in right eye was reduced perception to light. Ciliary as well as conjunctival congestion was present. Nebular leucomatous opacity was present between 4-6 0’clock positions on the cornea. Ulcer was present, 4-6mm, irregular with punched out edges. It also showed vascularisation and Striate Keratopathy (SK’S) i.e. corneal oedema with descemets folds. Fluorescent staining of cornea showed corneal ulceration. Examination of left eye was normal. A corneal scraping was performed and sent to Department of Microbiology for diagnosis.
Microbiology Methods
Scraping obtained from the corneal ulcer showed presence of fungal hyphae on 10% potassium hydroxide mount (KOH) [Table/Fig-2]. Gram stain and Zehil-Neelson stain of the scraping did not reveal any bacteria. Culture of corneal scraping for bacterial aetiology did not show growth. Culture on sabourauds dextrose agar (SDA) after one week showed fungal growth. The growth was whitish colored initially, then it became downy-wooly to granular yellowish-green and progressed to dark green colour with white collar. Diffused bright brick red pigment into the medium was observed [Table/Fig-3].
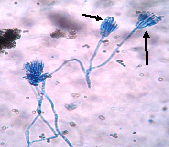
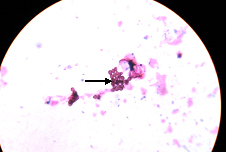
Microscopy of the fungal growth with Lactophenol cotton blue (LPCB) showed chains of single cell conidia borne on philaides, produced on metulae, with a brush like appearance [Table/Fig-4]. It was identified as Penicillium spp. Diffusible red pigment is produced by few species of the genus Penicillium like P. marneffei, P. rubrum, P.purpurogenum, P. janthinellum and P. citrinum. However Penicillium marneffei is the only known Penicillium species that exhibits temperature-dependent dimorphic growth. At temperatures below 37°C, the fungus grows as mycelia with the formation of septate hyphae, bearing conidiophores and conidia typical of the genus Penicillium. For the demonstration of dimorphism of the fungus, it was cultured on nutritionally enriched medium, Brain Heart Infusion Agar (BHIA) and incubated at 37OC for the growth of yeast phase. It showed the formation of yeast- like cells with the formation of fission arthroconidium cells demonstrated by Gram staining method [Table/Fig-5] and confirmed this species as Penicillium marneffei.The mold-to-yeast conversion or phase transition, which is thermally regulated, is a diagnostic characteristic of P. marneffei. In contrast to P. marneffei, the other Penicillium species are not dimorphic. Patient was started on antifungal treatment with topical amphotericin-B 0.15% and natamycin 5% suspension every hour with cyclopentolate 1%, sodium chromoglyacate 2%, ocular lubricant and 0.03% flurbiprofen and discharged. He was asked to visit the OPD after a week, however he did not report and was lost for followup.
Right eye showing corneal opacity

Direct microscopy - KOH mount of corneal scraping showing numerous fungal septate hyphae
Growth on SDA- Culture showing typical wooly downy to granular yellowish-green and then dark green in colour with distinctive red diffusible pigment of Penicillium marneffei

Lactophenol cotton blue (LPCB) showed the chains of single cell conidia born on philaides, produced on metulae, with a brush like appearance
Grams staining from brain heart infusion broth (BHI) for yeast phase; showed the presence of yeast-like form with the formation of fission arthroconidium cells.
Discussion
Fungal keratitis remains a diagnostic and therapeutic challanges [1-3]. Difficulties are related to establishing a clinical diagnosis, isolation of causative agent in laboratory for confirmation and successful treatment. Delayed diagnosis is mainly due to lack of suspicion by the clinican [3-6]. There is also a management challenge because of poor corneal penetration and limited availability of antifungal agents. Sharma S et al., reported 44% of all corneal ulcers were caused by fungi from South India [3]. In this decade, fungal keratitis is a foremost blinding disease in India. A high incidence of 63% has been reported by Basak SK et al., from West Bengal [7]. Gopinath et al., reported males are affected more frequently and often follow trauma to cornea especially by organic vegetative matter or objects contaminated with soil [4,8,9]. Topical applications of steroids and/or use of contact lens are additional factors responsible for fungal keratitis. Patients with systemic factors like DM, immunocompromised states like HIV are also at risk of fungal keratitis. In the present case the patient is an agricultural worker, and he had a history of trauma to the eye by working fan. He is not suffering from DM hypertension and was immunocompetant. Incidence of keratitis due to penicillium is very low. Hence we report this case. In 1972, 5 cases of penicillium keratitis were reported by Reddy et al.,[10].
Incidentally from last decade incidence of Penicillium keratitis is being frequently reported from India. Ritu Arora et al., from New Delhi reported Penicillium keratitis in vernal keratoconjunctivitis [11]. Study of basak SK west bengal, eastern, India on eidemiology and microbiological diagnosis of suppurative keratitis isolated 10.1% cases due to Penicillium [7]. Similarly a study of mycotic corneal ulcer in upper Assam, India was found to have 15.2% cases due to Penicillium spp. [12]. After 4-years this present case of keratitis due to Penicillium which we identified upto a species level i.e Penicillium marneffei, by confirming their microscopic finding, pigment production and dimorphism is being reported. Though keratitis due to Penicillium spp. are reported in other studies, our case of keratitis due to Penicillium marneffei is in an agricultural worker who is immunocompetant. This is a very rare case report from Maharashtra, India. Here trauma to the eye by working fan during the farm work seems to be the main contributing factor leading to injury and inoculation of fungus. The present case indicating that Penicillium keratitis can occur in an immunocompetant individual.
Conclusion
The role of diagnostic mycology is significant in the management of fungal keratitis. Culture confirmation of fungal infections to the species level is decisive for institution of appropriate antifungal therapy. In the present case, high clinical suspicion and accurate microbiological diagnosis aided towards successful management of patient.
[1]. JP Whitcher, M Srinivasan, MP Upadhyay, Corneal blindness: a global perspective. Bull World Health Organ 2001 79:214-21. [Google Scholar]
[2]. TP O’Brien, Keratitis. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of Infectious Diseases 2000 5th EditionNew YorkChurchill Livingstone:1257-66. [Google Scholar]
[3]. S Sharma, M Srinivasan, C George, The current status of Fusarium species in mycotic keratitisin South IndiaJ Med Microbiol 1993 11:140-7. [Google Scholar]
[4]. U Gopinathan, P Garg, M Fernandes, The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India.Cornea. 2002 21:555-9. [Google Scholar]
[5]. SV Jadhav, NR Gandham, RN Misra, MT Ujagare, M Sharma, M Sardar, Prevalence of fungal keratitis from tertiary care hospital from western part of India.Int. Journal of Microbiology Research 2012 4(4):204-7. [Google Scholar]
[6]. L Ajello, RJ Hay, Medical Mycology (1998). In: Topley & Wilson’s Microbiology and Microbial infections.Arnold, London 1998 [Google Scholar]
[7]. SK Basak, S Basak, A Mohanta, A Bhowmick, Epidemiological and microbiological diagnosis of suppurative keratitis in Gangantic West Bengal,Estern IndiaIndian J Opthalmol. 2005 53:17-22. [Google Scholar]
[8]. MP Upadhyay, PC Karmachaya, S Koirala, Epidemiologic charectristics,predisposing factors and etiologic diagnosis of corneal ulceration in NepalAm J Opthalmol 1991 15:92-99. [Google Scholar]
[9]. AA Dunlop, ED Wright, SA Howlader, Suppurative corneal ulceration in Bangladesh: A study of 142 cases examining the microbiological diagnosis, clinical and epidemiological features of bacterial and fungal keratitisAust N Z J Opthalmol 1994 22:105-110. [Google Scholar]
[10]. PS Reddy, OM Satyendran, M Satapathy, HV Kumar, PR Reddy, Mycotic keratitisIndian J Opthalmol 1972 20:101-8. [Google Scholar]
[11]. R Arora, S Gupta, UK Raina, DK Mehta, M Taneja, Penicillium Keratitis in Vernal Keratoconjunctivitis.Indian J Opthalmol 2002 50:215-6. [Google Scholar]
[12]. R Nath, S Baruah, L Saikia, B Devi, AK Borthakur, J Mahanta, Mycotic corneal ulcer in upper AssamIndian J Opthalmol 2011 59:367-71. [Google Scholar]