Introduction
CRP is a pentameric plasma protein with homologs in vertebrates and many invertebrates that participate in the systemic response to inflammation. It is a pattern recognition molecule, that is extremely sensitive and non-specific acute-phase marker for inflammation, produced in response to many forms of injury other than binding to specific molecular configurations that are typically exposed during cell death or found on the surfaces of pathogens [1]. It is regulated by cytokines like interleukin-6 (IL- 6), interleukin-1β (IL-1β) and tumour necrosis factor-α (TNF-α) [2,3]. These in turn cause systemic changes including hepatic release of a range of plasma proteins, activation of complement proteins and various metabolic changes [Table/Fig-1] [4].
Synthesis of C-reactive protein Kravitz et al.,[4]
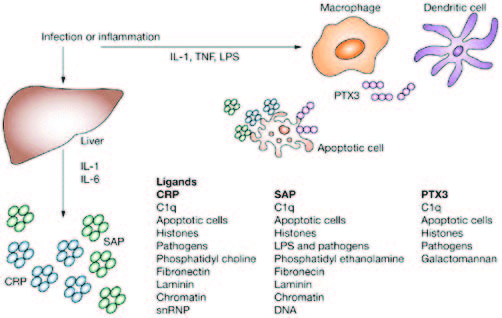
CRP levels have an association with smoking, obesity, triglycerides, diabetes and periodontal disease [5]. It is proposed that changes in cellular and molecular components of peripheral blood can be found in subjects with periodontitis because of inflammatory changes of the periodontal tissues [6]. According to Panichi et al., [7] CRP is currently considered a key biomarker of systemic inflammation, and although it is mainly synthesised by hepatocytes in the liver in response to inflammation and tissue damage, it can also be produced locally by arterial tissue [Table/Fig-2].
Acute phase response Panichi et al.,[7]
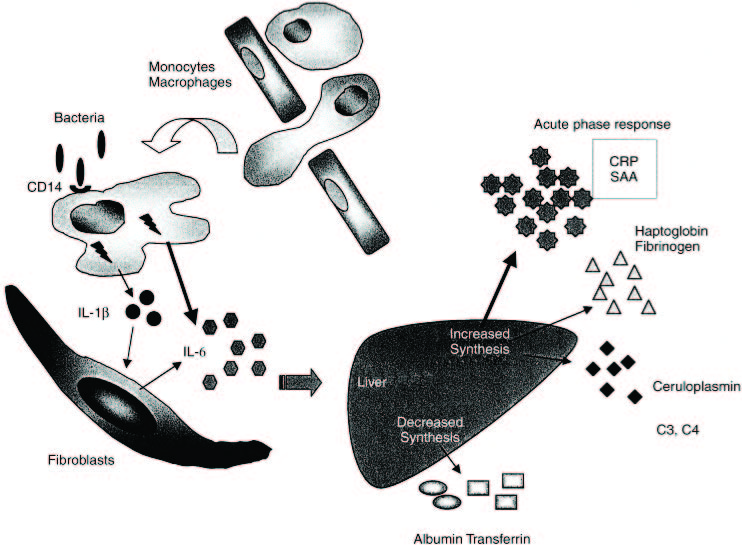
CRP and other acute phase molecules are usually present at relatively low levels in plasma, but may be raised dramatically within 72hrs of tissue injury or with infection. CRP opsonizes bacteria for complement-binding and activates complement when complexed [8]. The normal CRP levels vary between populations, with mean values between 1.0 to 3.0 mg/l. However, using ultrasensitive methods, it is possible to detect CRP levels as low as <1.0 mg/l.
The acute-phase reaction represents an early and highly complex reaction of the organism to a variety of injuries such as bacterial, viral or parasitic infection, mechanical or thermal trauma, ischaemic necrosis or malignant growth [2]. This induces a complex series of non-specific, systemic, physiological and metabolic responses leading to increased synthesis and secretion of plasma proteins. This phenomenon is termed as ‘acute phase response’ [9]. These changes are called ‘acute’ because most are observed within hours or days following the onset of infection or injury, although some acute phase changes also indicate chronic disease [3]. The presence of certain acute phase changes in an otherwise healthy individual can alert the physician to hidden diseases. The purpose of these responses is to restore homeostasis and to remove the cause of its disturbance.
C - Reactive Protein
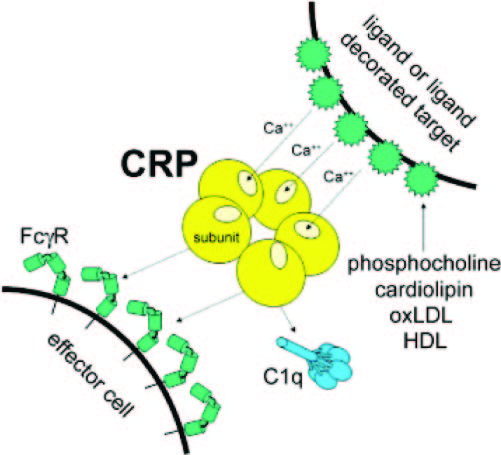
CRP was first reported by Tillett and Francis in 1930 and was named so because it was discovered as a substance in the serum of patients with acute inflammation that reacted with the C-(capsular) polysaccharide of Pnuemococcus [10]. It was initially thought that CRP might be a pathogenic secretion as it was elevated in people with a variety of illnesses including cancer however, discovery of hepatic synthesis demonstrated that it is a native protein [11,12]. It is normally present in ng/ml quantities but may increase dramatically to hundred of μg/ml within 72hrs following tissue injury. CRP is a trace protein in overtly normal, healthy individuals, the median value being 0.8 mg/l, with an interquartile range of 0.3 to 1.7 mg/l [9]. CRP plays a key role in the host’s defense against infection [13]. In the presence of calcium, CRP specifically binds to polysaccharides such as phosphocholine moieties present on the cell surface of many pathogenic microbes. Its binding activates the classical complement pathway and opsonises (prepares) ligands for phagocytosis. It also neutralises the pro-inflammatory platelet-activating factor and down-regulates polymorphs [8].
Methods of Measuring CRP Levels
CRP can be measured using immuno-turbidimetric or immuno-electrophoretic assays or latex slide agglutination method. The high-sensitivity CRP (hs-CRP) assay uses labeled monoclonal or polyclonal anti-CRP antibodies in an enzyme-linked immunosorbent assay (ELISA) or an immune-fluorescent assay. Laser nephelometry can also be used to detect hs-CRP levels [9]. Applications of routine CRP level measurement.
Can be done for i) Screening for organic disease, ii) Monitoring of extent and activity of disease: infection, inflammation, malignancy and necrosis. iii) Detection and management of recurrent infection.
Interpretation of Clinical Serum CRP Measurements
CRP is a non-specific marker and measurement of CRP alone cannot be diagnostic of any condition. Thus, its value needs to be correlated with clinical and laboratory findings. Clinically, CRP can be measured in serum in 2 ways i) routine CRP which measures level above 3mg/L in adults and ii) High sensitivity (hs-CRP) measuring range up to 3mg/L especially in neonatal medicine, screening as a prognostic marker in adults with respect to atherothrombotic disease and osteoarthritis [9].
Periodontal Disease and CRP Protein
Periodontitis is defined as the inflammatory disease of the supporting tissues of the teeth caused by specific microorganisms or groups of specific microorganisms, resulting in progressive destruction of the periodontal ligament and alveolar bone with pocket formation, recession or both [14]. This condition occurs in response to a predominantly gram-negative bacterial infection originating from dental plaque. However, the disease typically remains asymptomatic for decades and can be detected only by clinical examination with a periodontal probe or with intra-oral radiographs. It is only recently that researchers have begun to identify local and systemic inflammatory process that encourages a pathological response to an initial commensal microflora [15]. Increased levels of acute-phase proteins have been noted with gingival inflammation and periodontitis, reflecting the locally stressed environment [1].
Since CRP is an acute-phase reactant produced by the liver in response to diverse inflammatory stimuli, recent studies have shown that their levels are elevated in periodontal disease. However, not all studies have reported an association between destructive periodontal disease and CRP. These reports may possibly reflect differences in destructive periodontal disease severity or disease progression in different study populations. CRP value <10mg/L were considered normal, while acute bacterial infections have been reported in 80% to 85% of patients with CRP values >100mg/L [16]. Historically, CRP values >10 mg/l were regarded as diagnostic for a bacterial infection, while values <10 mg/l were neglected. This may be because CRP assays in the past were not very accurate and sensitive as in present and thus were less efficient in detecting the levels of CRP <10mg/l. So, these days’ high-sensitivity assays for CRP have come into widespread use, allowing laboratories to determine CRP levels in serum as low as 0.15 mg/l.
Hage & Szalai [17] reported that CRP can bind phosphoethanolamine and phosphocholine of disrupted bacterial and host cell membranes as well as chromatin, small nuclear ribonucleoproteins, laminin and fibronectin in the presence of calcium. CRP, when bound to these ligands can activate the complement cascade. CRP receptors also exist on macrophages, monocytes and neutrophils and thus bound CRP can target bacterial and damaged host cells for phagocytosis and help direct and amplify the subsequent local inflammatory response to infection, trauma and necrosis [Table/Fig-3]. In acute inflammation serum CRP levels exceed 100 mg/L, and the level decreases in chronic inflammation.
Host response of CRP Hage et al.,[17]
In a very early study conducted by Boucher et al., [18], it was apparent from the results that CRP appears in the serum of patients with some forms of inflammatory oral disease. The highest incidence of positive CRP tests and the strongest CRP test reactions were observed in patients with acute alveolar abscesses. This study was one of the earliest studies to determine a relationship between the levels of CRP and oral diseases. In the present days, the levels of CRP have been correlated with many systemic conditions.
Recent evidence has indicated that patients with severe periodontitis have increased serum levels of CRP, when compared with unaffected control population [5]. But they fall short in indicating that periodontitis was the cause for the observed serum CRP levels as CRP levels fluctuate with various confounding factors like aging, high blood pressure, alcohol use, smoking, low levels of physical activity, chronic fatigue, coffee consumption having elevated triglycerides, insulin-resistance diabetes, taking estrogen, eating a high-protein diet, suffering from sleep disturbances and depression [19].
Various studies have proved a positive association between the presence of chronic periodontitis and high serum CRP levels [15, 20–24] because it is biologically plausible that inflammatory mediators (IL-1, IL-6 and TNF-α) are released under conditions of periodontitis and present the capacity to stimulate the hepatocytes to produce CRP. In the similar manner, it can be expected that, in the presence of chronic periodontitis, higher serum CRP levels would be found.
ABL is not always related to current inflammation in the periodontium; however, it represents the degree of periodontal destruction directly. Radiographs underestimate bone loss compared to direct bone measurements, and panoramic radiography is slightly less accurate than bitewing radiography. Saito et al., [25] surveyed 179 Japanese men of the same age group. They observed that ABL around posterior teeth was associated with elevated level of CRP. In another study, Persson et al., [26] found the hs-CRP level to be above 10.0 mg/l in all the subjects in which evidence of significant alveolar bone loss was present indicating periodontitis. Thus, the level of CRP tends to increase with the periodontal destruction marked by ABL.
The results of Salberz et al., [27] have confirmed that aggressive periodontitis is significantly related to elevated CRP levels as the generalised aggressive periodontitis (3.72 mg/l) group had significantly elevated levels of CRP compared to the localised aggressive periodontitis (2.57 mg/l) and non-periodontitis (1.54 mg/l) groups. Their result is consistent with the interpretation that the surface area or volume of the periodontal lesion is the most important determinant of serum CRP levels in aggressive periodontitis patients. The potential effect of smoking was illustrated by Fredriksson et al., who found a median CRP concentration of non-smoking patients with periodontitis of 2 mg/l (mean age 52 years), compared to a median of 0 mg/l for non-smoking matched controls and a median CRP of around 2 mg/l regardless of their periodontal status [22]. Also, Noack et al., related periodontal status in adults to circulating CRP allowing for smoking, age and obesity, and reported that there was a significant relationship between severity of periodontitis and circulating CRP [20]. The potential role of smoking in influencing these data is currently uncertain.
Recent trials have indicated that treatment of periodontal infections, whether by intensive mechanical therapy, drug therapy or extraction, can significantly lower serum levels of CRP. To support this concept, D’Aiuto et al., [28] conducted a study where he observed a median decrease in serum CRP of 0.5 mg/l 6 mnths after completion of periodontal therapy. The authors concluded that control of periodontitis can be achieved with non-surgical periodontal therapy, significantly decreasing the serum mediators and markers of acute phase response. Since CRP is an acute phase protein, once the cause for elevation of CRP is eliminated CRP levels fall drastically.
In contrast to the above study, Ide et al., [29] conducted a study to find out whether the circulating acute phase protein levels decreases following the treatment of periodontal disease, but failed to observe a reduction in circulating CRP following non-surgical periodontal therapy. Possible explanation why CRP remains elevated even after SRP is that as SRP is insufficient to control periodontal disease progression in all periodontitis subjects. And it may not be possible to eliminate all the microorganisms from deep inaccessible pockets. Removal of deposits and microorganisms from these locations may require surgical intervention and/or the use of antimicrobial agents.
To fully confirm that elevation in CRP is due to periodontal infection, it is essential to see whether periodontal treatment is effective in reducing CRP level. Following successful periodontal basic therapy, bacterial load is significantly reduced, while antibody titers to the specific pathogens are improved. As a result of these changes, local inflammation significantly decreases and there is a significant improvement of the clinical parameters. We need to know whether this improvement in clinical parameter have any role in reducing the elevated CRP levels in periodontitis patients.
Further, in periodontitis patients elevated serum CRP is associated with high levels of infection with periodontal pathogens [30,31] Dye et al., [32] reported a high serum titre to Porphyromonas gingivalis and the presence of periodontal disease which are independently related to high CRP levels. In contrast, the titre of A. actinomycetecomitans was not related to the high CRP levels. Similar results for P. gingivalis were also observed by Pitiphat et al., [33]. These data have received considerable attention as they prove to be showing the association of the periodontal disease and the increased level of CRP.
Tuter et al., conducted a study to detect CRP in gingival crevicular fluid (GCF) but he failed to show any relation between CRP and the clinical parameters [34]. However, according to Kumar et al., CRP level is more significant in GCF and confirms the underlying inflammatory component of the disease activity in chronic periodontitis. Nonsurgical periodontal treatment was effective in reducing the levels of CRP in GCF, and the levels of GCF biomarkers specific for three aspects of periodontitis – degree of inflammation, collagen degradation and bone turnover – correlated with the clinical features of periodontal disease [35].
As the goal of modern health care continues to shift from an attitude of treatment to one of prevention, investigations will increasingly be directed toward elucidating predisposing factors that lead to atherosclerosis and developing appropriate early intervention. Periodontal diseases may represent one such factor. Periodontitis itself is endemic in many countries, despite the fact that treatment modalities have proven successful over the long term and preventive measures are well understood. It will be incumbent on all dental professionals to take appropriate measures to both counsel patients in the prevention of periodontal diseases and, where necessary, arrange treatment for affected individuals to receive appropriate care in a specialist setting [36].
Conclusion
From the present evidence it can be concluded that chronic periodontitis results in higher systemic levels of CRP. The elevated inflammatory factors may increase inflammatory activity in atherosclerotic lesions and potentially increasing the risk for cardiovascular events. Periodontitis is treatable; moreover, it is preventable. Experimental conformation of this shows that another widely prevalent and preventable contributor to the burden of cardiovascular disease would be added to the options available of the clinicians and public health practitioners for the control of the epidemic of cardiovascular disease. Dr. Gordon Douglass, President of the American Academy of Periodontology had stated that, “I foresee patients receiving routine CRP testing in their dentist or periodontist’s office in the near future”. This could help early diagnosis of disease sooner rather than later.
[1]. Black S, Kushner I, Samols D, C-reactive ProteinJ Biol Chem 2004 279:48487-90. [Google Scholar]
[2]. Ebersole JL, Cappelli D, Acute-phase reactants in infections and inflammatory diseasesPeriodontol 2000 23:19-49. [Google Scholar]
[3]. Bennett JC, Plum F, The acute phase response. Cecil textbook of Medicine Edition 20thSaunders. Philadelphia 1996 2:1535-37. [Google Scholar]
[4]. Kravitz MS, Shoenfeld Y, Autoimmunity to protective molecules: is it theperpetuum mobile (vicious cycle) of autoimmune rheumatic diseasesNat Clin Pract Rheumatol 2006 2:481-90. [Google Scholar]
[5]. Gomes-Filho IS, Coelho JMF, Cruz SS, Passos JS, Freitas COT, Farias NSA, Chronic periodontitis and C-reactive protein levelsJ Periodontol 2011 82:969-78. [Google Scholar]
[6]. Lopez R, Baelum V, Hedegaard CJ, Bendtzen K, Serum levels of C-reactive protein in adolescents with periodontitisJ Periodontol 2011 82:543-49. [Google Scholar]
[7]. Panichi V, Migliori M, Pietro SD, Taccola D, Andreini B, Metelli MR, The link of biocompatibility to cytokine productionKidney Int 2000 58:S96-103. [Google Scholar]
[8]. Gani DK, Lakshmi D, Krishnan R, Emmadi P, Evaluation of C-reactive protein and interleukin-6 in the peripheral blood of patients with chronic periodontitisJ Ind Soc Periodontol. 2009 13(2):69-74. [Google Scholar]
[9]. Weatherall DJ, Ledingham JGG, Warrell DA, The acute phase response and C-reactive protein. Oxford textbook of Medicine 1996 Edition 3rdNew YorkOxford university press:1527-33. [Google Scholar]
[10]. Tillett WS, Francis T, Serological reactions in pneumonia with a nonprotein somatic fraction of pneumococcusJ Exp Med 1930 52(4):561-71. [Google Scholar]
[11]. Pepys MB, Hirschfield GM, C-reactive protein: a critical updateJ Clin Invest 2003 111(12):1805-12. [Google Scholar]
[12]. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM, C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitusJAMA 2001 286(3):327-34. [Google Scholar]
[13]. Marnell L, Mold C, Du Clos TW, C-reactive protein: ligands, receptors and role in inflammationClin Immunol. 2005 117:104-11. [Google Scholar]
[14]. Newman MG, Takei HH, Klollevold PR, Carranza FA, Classification of diseases and conditions affecting the periodontium. Clinical Periodontology 2006 Edition 10thPhiladelphiaSaunders:103-04. [Google Scholar]
[15]. Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS, Acute-phase inflammatory response to periodontal disease in the US populationJ Dent Res 2000 79(1):49-57. [Google Scholar]
[16]. Craig RG, Yip JK, So MK, Boylan RJ, Socransky SS, Haffajee AD, Relationship of destructive periodontal disease to the acute-phase responseJ Periodontol 2003 74:1007-16. [Google Scholar]
[17]. Hage FG, Szalai AJ, C-Reactive Protein Gene Polymorphisms, C-Reactive Protein Blood Levels, and Cardiovascular Disease RiskJ Am Coll Cardiol 2007 50(12):1115-22. [Google Scholar]
[18]. Boucher NE, Hanrahan JJ, Kihara FY, Occurance of C-reactive protein in oral diseaseJ Dent Res 1967 46:624 [Google Scholar]
[19]. Graziani F, Cei S, Tonetti M, Paolantonio M, Serio R, Sammartino G, Systemic inflammation following non-surgical and surgical periodontal therapyJ Clin Periodontol 2010 37:848-54. [Google Scholar]
[20]. Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, Nardin ED, Periodontal infections contribute to elevated systemic C-reactive protein levelJ Periodontol 2001 72:1221-27. [Google Scholar]
[21]. Ebersole JL, Machen RL, Steffen MJ, Willmann DE, Systemic acute-phase reactants, C-reactive protein and haptoglobin in adult periodontitisClin Exp Immunol. 1997 107:347-52. [Google Scholar]
[22]. Fredriksson MI, Figueredo CMS, Gustafsson A, Bergstrom KG, Asman BE, Effect of periodontitis and smoking on blood leukocytes and acute-phase proteinsJ Periodontol. 1999 70:1355-60. [Google Scholar]
[23]. Loos BG, Craandijk J, Hoek FJ, Wertheim-van Dillen PME, van der Velden U, Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patientsJ Periodontol 2000 71:1528-34. [Google Scholar]
[24]. Slade GD, Ghezzi EM, Heiss G, Beck JD, Riche E, Offenbacher S, Relationship between periodontal disease and C-reactive protein among adults in the atherosclerosis risk in communities studyArch Intern Med 2003 163:1172-79. [Google Scholar]
[25]. Saito T, Murakami M, Shimazaki Y, Oobayashi K, Matsumoto S, Koga T, Association between alveolar bone loss and elevated serum C-reactive protein in Japanese menJ Periodontol. 2003 74:1741-46. [Google Scholar]
[26]. Persson GR, Pettersson T, Ohlsson O, Renvert S, High-sensitivity serum C-reactive protein levels in subjects with or without myocardial infarction or periodontitisJ Clin Periodontol. 2005 32:219-24. [Google Scholar]
[27]. Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA, C-reactive protein levels in patients with aggressive periodontitisJ Periodontol 2006 77:933-39. [Google Scholar]
[28]. D’Aiuto F, Parkar M, Andreaou G, Brett PM, Ready D, Tonetti MS, Periodontitis and atherogenesis: causal association or simple coincidenceJ Clin Periodontol 2004 31:402-11. [Google Scholar]
[29]. Ide M, McPartlin D, Coward PY, Crook M, Lumb P, Wilson RF, Effect of treatment of chronic periodontitis on levels of serum markers of acute-phase inflammatory and vascular responsesJ Clin Periodontol. 2003 30:334-40. [Google Scholar]
[30]. Gabay C, Kushner I, Acute-phase proteins and other systemic responses to inflammationN Engl J Med 1999 340:448-54. [Google Scholar]
[31]. Reeves G, C-reactive proteinAust Prescr 2007 30:74-76. [Google Scholar]
[32]. Dye BA, Choudhary K, Shea S, Papapanou PN, Serum antibodies to periodontal pathogens and markers of systemic inflammationJ Clin Periodontol 2005 32:1189-99. [Google Scholar]
[33]. Pitiphat W, Savetsilp W, Wara-Aswapati N, C-reactive protein associated with periodontitis in a Thai populationJ Clin Periodontol 2008 35:120-25. [Google Scholar]
[34]. Tuter G, Serdar M, Kurtis B, Walker SG, Atak A, Toyman U, Effects of scaling and root planing and subantimicrobial dose doxycycline on gingival crevicular fluid levels of matrix metalloproteinase-8, -13 and serum levels of HsCRP in patients with chronic periodontitisJ Periodontol. 2010 81:1132-39. [Google Scholar]
[35]. Kumar S, Shah S, Budhiraja S, Desai K, Shah C, Mehta D, The effect of periodontal treatment on C-reactive protein: A clinical studyJ Nat Sc Biol Med 2013 4:379-82. [Google Scholar]
[36]. Ramamoorthy RD, Nallasamy V, Reddy R, Esther N, Maruthappan Y, A review of C-reactive protein: A diagnostic indicator in periodontal medicineJ Pharm Bioall Sci 2012 4(2):422-26. [Google Scholar]