Neuromyelitis Optica with NMO-IgG/Anti-AQP4 Antibody Positive: First Case Reported from Uttarakhand India
Manish Mittal1, Garima Mittal2
1 Associate Professor, Department of Neurology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
2 Assistant Professor, Department of Microbiology Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Mittal, Associate Professor, Department of Neurology, Himalayan Institute of Medical Sciences Jolly Grant, Dehradun, Uttarakhand, India. Phone : 0091-135-2471577, 0091-9759075607, E-mail : drmittal@yahoo.com
Neuromyelitis optica (also known as Devic’s disease) is an idiopathic, severe, demyelinating disease of the central nervous system that preferentially affects the optic nerve and spinal cord. The presence of a highly specific serum autoantibody marker (NMO-IgG) further differentiates neuromyelitis optica from multiple sclerosis and has helped to define a neuromyelitis optica spectrum of disorders. We present a case of 37-year-old man who has initially presented with transverse myelitis from which he recovered partially after treatment but later presented with bilateral optic neuritis. MRI brain revealed hyperintensity in bilateral optic nerves, periventricular area and also in the thalamic region. Diagnosis was confirmed by positive NMO – IgG/anti-AQP4 antibody.
Multiple sclerosis, Neuromyelitis optica
Case Report
A 37-year-old man from Uttarakhand, farmer by occupation was admitted to our hospital in June 2013 with complaints of weakness in bilateral upper limb and lower limb of six days duration. There was also difficulty in passing urine since four days. On examination patient had quadriplegia with sensory loss below C5 dermatome. MRI cervical spine revealed expansile hyperintense lesions in cervical cord from C4-C6 (i.e. 3 cervical segments) on T2-weighted image [Table/Fig-1]. So, he was put on five days methylprednisolone therapy to which he responded by improvement in limb weakness and started walking with support.
MRI showing hyperintensity in cervical cord on T2W Image

However, patient presented again in neurology OPD after four months with complaints of acute painless bilateral loss of vision. On examination visual acuity was reduced to light perception and papillary reaction was sluggish. Fundus examination was normal. There was no significant past history of any neurological disorder or allergy to any substance. Laboratory work-up revealed normal hematocrit, white blood cell counts, platelets and ESR. Kidney function, thyroid function and random glucose tests were in normal limit. Patient was negative for Hepatitis B surface antigen and hepatitis C antibodies.
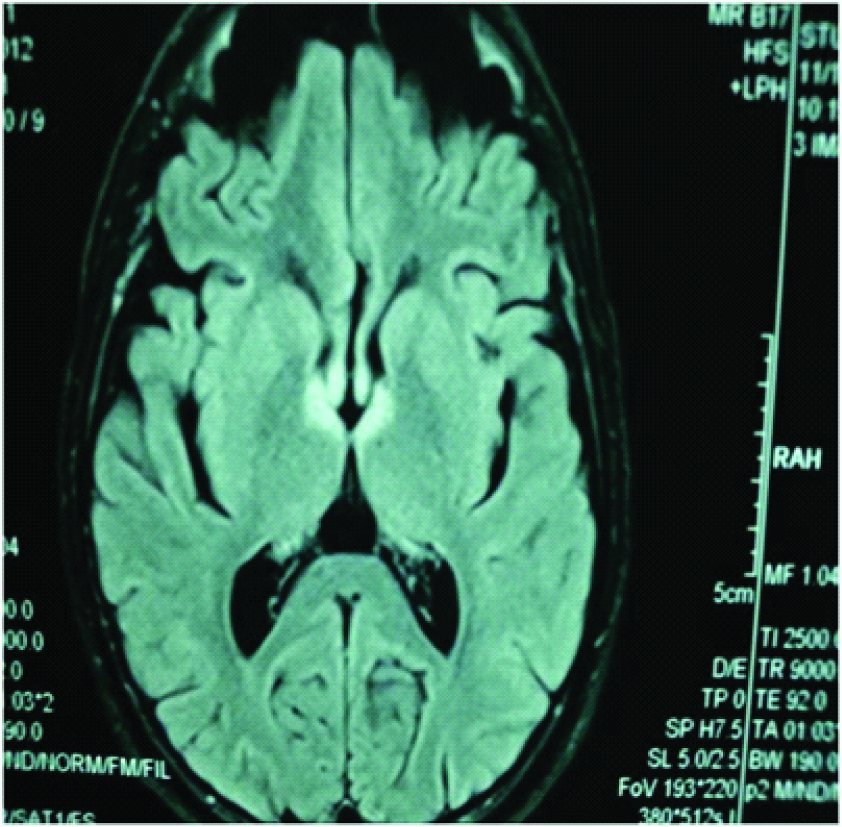
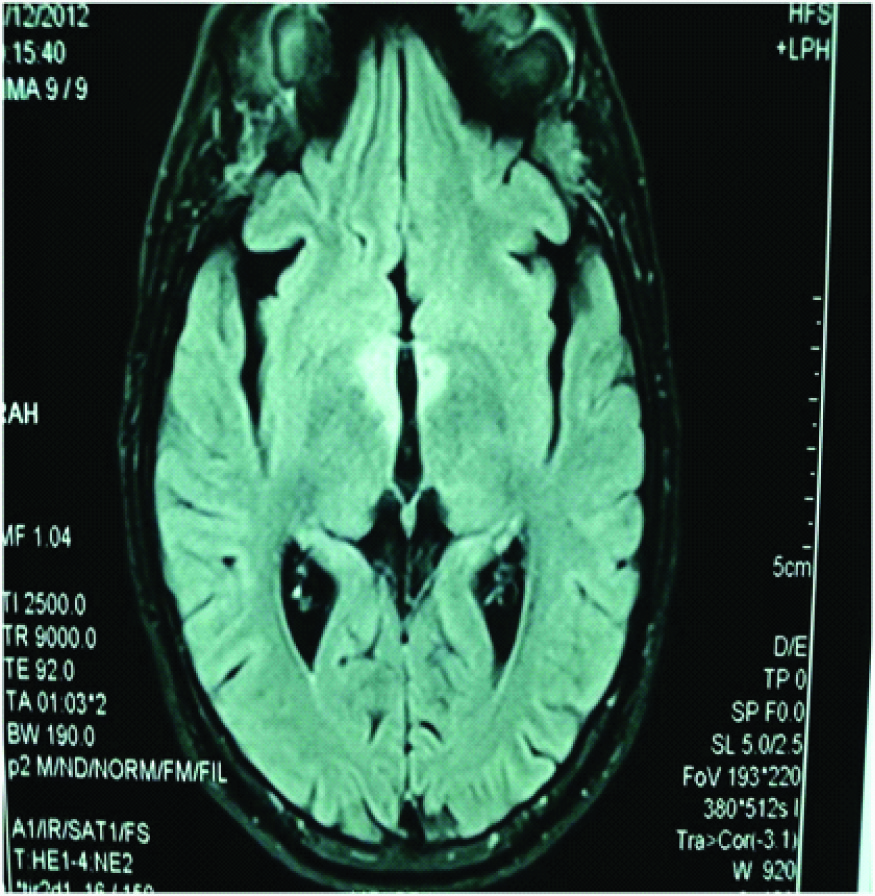
On neuroimaging, MRI brain showed hyperintensity in bilateral optic nerves, periventricular area [Table/Fig-2] and also in the thalamic region[Table/Fig-3]. For confirmation of diagnosis the serum sample was sent to Amrita Institute, Cochin to look for NMO – IgG/anti-AQP4 antibody status. After about a week results for this highly specific antibody came positive.
MRI brain showing hyperintensity in bilateral optic nerves and periventricular area
MRI brain showing periventricular hyperintensities in thalamic region
A diagnosis of Neuromyelitis optica was made and the patient was treated initially with intravenous methylprednisolone followed by oral prednisolone 40mg once daily and Azathioprine 75mg daily. Patient responded to the treatment and discharged after seven days. On follow-up patient showed only partial recovery of his vision loss.
Discussion
Neuromyelitis optica (NMO), also known as Devic’s disease or Devic’s syndrome, is an autoimmune, inflammatory disorder in which a person’s own immune system preferentially attacks the optic nerves and spinal cord producing optic neuritis and myelitis [1]. It is presumed to be an antibody-mediated disorder, the target antigen being the water channel aquaporin-4 (AQP4) on astrocyte cell membranes [2].
NMO is considered as a clinical variant of multiple sclerosis (MS). Whereas MS is a CD4+ T-cell mediated autoimmune disease, NMO is a humorally mediated autoimmune disease. The serum autoantibody marker, neuromyelitis optica-immunoglobulin G (NMO-IgG), appears specific for NMO [3] Whereas, in a study from south India, only one of the eight patients with NMO with demyelinating disease was positive for NMO IgG [4].
First described in 1894, its incidence worldwide is around five per one lakh. The disease is much rarer in India. Singhal BS [5] has reported 14 cases from 1957-83. Pandit et al., recently reported that 10% (8/78) of a south Indian cohort of patients with demyelinating disease satisfied the criteria for NMO [6]. It is more common in Japan & East Asia. The name Devic’s disease, Devic’s syndrome, Neuromyelitis Optica is used interchangeably. It occurs in patients of varied ages (1 – 73yrs).
The criteria used for diagnosis were those suggested By Wingerchuk DME et al., [7] which requires two absolute criteria plus at least two of three supportive criteria being –
Absolute criteria
Optic neuritis
Acute myelitis
Supportive criteria
Brain MRI not meeting criteria for MS at disease onset.
Spinal cord MRI with contiguous T2-weighted signal abnormality extending over 3 or more vertebral segments, indicating a relatively large lesion in the spinal cord.
NMO – IgG/anti-AQP4 seropositive status.
Our patient has initially presented with transverse myelitis from which he recovered partially after treatment but later presented with bilateral optic neuritis. Differential diagnosis of such opticospinal presentation are Multiple Sclerosis, ADEM, Neuromyelitis optica, Lymphoma, SLE, Sjogren’s and Herpes zoster [8]. Our case fulfilled the McDonald’s criteria of multiple sclerosis as there were two attacks disseminated in time and space with clinical evidence of two or more lesions. However, lesion appearance and location was not suggestive of multiple sclerosis and is typically seen in NMO. In NEO, lesions are seen in optic nerve, spinal cord, periventricular and thalamic regions as aquaporin channels are rich in these locations. Both the above mentioned absolute criteria and all three supportive criteria for the diagnosis of NMO were seen in this patient.
Conclusion
Exciting developments have occurred in the last two years in NMO. However, improvement in patient outcomes will still depend on early diagnosis, aggressive management of relapses and early effective immunosuppression. In developing country like ours it is difficult to do extensive work-up to rule out all the causes of demyelinating disorders. So emphasis should be made on proper history and examination along with minimal investigations to make the diagnosis.
[1]. Tirkey NK, Mandavi S, Gupta S, A Young Female Patient of Neuromyelitis Optica presenting with Hypocalcemic TetanyJAPI 2011 59:583-85. [Google Scholar]
[2]. Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR, IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channelJ Exp Med 2005 202:473-77. [Google Scholar]
[3]. Wingerchuk DM, Neuromyelitis opticaThe International MS Journal 2006 13:42-50. [Google Scholar]
[4]. Pandit L, Neuromyelitis optica antibody (NMO-IgG) status in Indian patients with multiple sclerosis and allied demyelinating disordersNeurology Asia 2008 13:175-78. [Google Scholar]
[5]. Singhal BS, Multiple sclerosis–Indian experienceAnnals of academic medicine 1985 14(1):32-36. [Google Scholar]
[6]. Pandit L, Transverse myelitis spectrum disordersNeurol India 2009 57:126-23. [Google Scholar]
[7]. Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG, Revised diagnostic criteria for neuromyelitis opticaNeurology 2006 66:1485-89. [Google Scholar]
[8]. Merle H, Smadja D, Cordoba A, Optic neuromyelitis and bilateral acute retinal necrosis due to varicella zoster in a patient with AIDSJ Fr Ophthalmol 1998 21:381-86. [Google Scholar]