Primary Retroperitoneal Inter-aorto-Caval Paraganglioma of the Organ of Zuckerkandl
Vaibhav Vikas1, Zeeshanuddin Ahmed2, Onkar Singh3, Sudhir Singh Pal4, Mool Chand Songra5
1Resident, Department of Surgery,Gandhi Medical College,Bhopal, M.P., India.
2Resident, Department of Surgery,Gandhi Medical College,Bhopal, M.P., India.
3Resident, Department of Surgery,Gandhi Medical College,Bhopal, M.P., India.
4Associate Professor, Department of Surgery,Gandhi Medical College,Bhopal, M.P., India.
5Professor and Head, Department of Surgery,Gandhi Medical College,Bhopal, M.P., India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. Vaibhav Vikas, 62 AP Colony, Gaya- 823001, Bihar, India.
Phone: 09770033669, Email: vaibhav.vikas@gmail.com
Tumour that arise from chromaffin cells at extra-adrenal locations are termed paragangliomas which are rare tumour. The organ of Zuckerkandl located along aortic bifurcation is the most common site of their occurrence. Herein, we report a case of 20-year-old male with large abdomino-pelvic paraganglioma of the organ of zuckerkandl with multiple pedicles to abdominal aorta. On exploratory laparotomy it revealed a large retroperitoneal mass with variable consistency with surfaces covered with tortuous vessels. This mass was adhered to the retroperitoneum with multiple arterial pedicles to abdominal aorta. Histopathologic evaluation revealed features of extra-adrenal paraganglioma with characteristic Zellballen appearance. Postoperative course was uneventful.
Paraumbilical, Raynaud’s phenomenon, Zellballen
Case Report
A 20-year-old male presented to us with abdominal pain over left hypochondriac, umbilical and left paraumbilical areas for past one year which was vague constant dull aching, sometimes radiating to the back. On clinical examination a globular mass of size approximately 10 x 10 cms was found occupying the part of the left paraumbilical and left lumbar region. Mass had restricted mobility in all directions with no relation to the respiration. Margins were well-defined all around with smooth surface. Mass became less palpable on straight leg raising test suggestive of intra-abdominal location. On shift test-mass did not change the position suggesting its retroperitoneal location. Liver, spleen and kidneys were not palpable. No lymphadenopathy was present and there was no evidence of free intraperitoneal fluid (ascites). Other systemic examination was normal. Provisional diagnosis of retroperitoneal lump was made and patient investigated further.
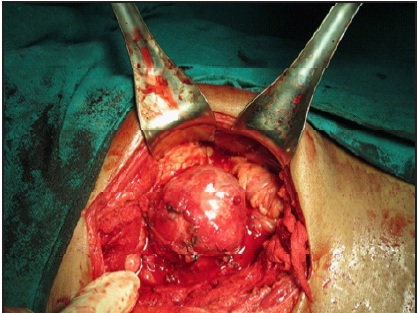
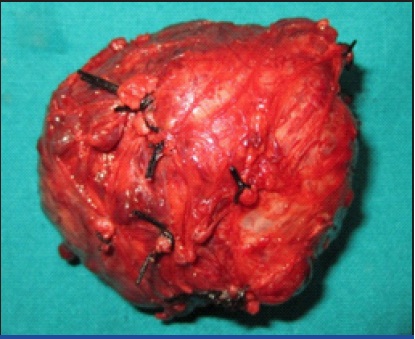
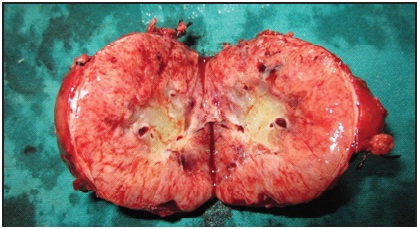
The patient was normotensive and otherwise healthy. Routine blood tests were normal. Computed tomography of abdomen with contrast revealed a retroperitoneal mass arising from the wall of abdominal aorta, lying anterior to aorta and inferior vena cava. Both adrenal glands were normal. After complete anaesthetic workup, laparotomy was done by transperitoneal approach which revealed a variable consistency-more of solid component retroperitoneal tumour of size 8cm x 8cm x 8cm with 3-4 arterial pedicles to aorta [Table/Fig-1]. Surface of tumour was smooth with no peritumoural adhesions. It was lying inferior to the pancreas without any surface contact. The tumour was resectable. The tumour shrunk after ligation of vascular pedicles. Complete excision of the tumour along with 0.5 x 0.5 cms of anterior wall of abdominal aorta was done after ligating and dividing the pedicles [Table/Fig-2,3]. Defect of aorta was primarily closed with prolene suture after applying vascular clamps. Tumour bed was formed of lower most part of inferior vena cava and abdominal aorta approximately 2-3 cms proximal to its bifurcation. Histopathologic examination of specimen revealed features of extra-adrenal paraganglioma with characteristic Zellballen appearance. Immunohistochemical staining of the permanent section specimen, were positive for chromogranin, synaptophysin, and S100 which confirmed the neuroendocrine origin of this neoplasm.
Intra-operative view of retroperitoneal mass
Completely resected tumour
Completely resected tumour
Discussion
About 2/3rd of paragangliomas are located in the head and neck region, and most of these are parasympathetic in origin. Sympathetic paragangliomas on the other hand, occur in head and neck region in only 5% of cases; 10% being found in the thorax, 10% in pelvis (mainly bladder and prostate), while most commonly (in 75% of cases) are located in the abdomen. The most common location of sympathetic paragangliomas in the abdomen is the organ of Zuckerkandl which is located in the retroperitoneum anterolateral to distal abdominal aorta in between the origin of inferior mesenteric artery and aortic bifurcation [1,2,3] like in our case. A similar case report on Interaorta- caval located tumor was reported by Mustafa Kemal Demirag et al. which was located retroperitoneally on the inferior part of the duodenum [4].
Most paragangliomas present in third to fifth decade of life. These tumour may be discovered incidentally or become evident because of symptoms produced secondary to either mass effect or production of excessive catecholamines [3]. Tumour that do not produce catecholamines typically present with abdominal pain or mass [5]. Functional paragangliomas are mostly localized in the abdominal and pelvic cavity. The classical features of catecholamine excess include episodic hypertension, headache, palpitations and sweating. This typical constellation of signs and symptoms is demonstrated in only one-third patients of catecholamine producing paragangliomas. Other less obvious presentations include hyperglycemia, panic attacks, fever, weight loss, myocardial infarctions, osteolytic bone metastases, and Raynaud’s phenomenon. About half of the patients have paroxysmal hypertension (48%) while sustained elevation of blood pressure is found in 29-50% patients. However, 2-13% patients may be normotensive. Among hormone producing tumour,smaller tumour are more likely to have functional presentation. In larger sized tumour much of the catecholamines produced by the tumour undergo intratumoural metabolization [2,3,6].
The levels of by-products of catecholamine metabolism (metanephrines, vanillylmandelic acid and 5-hydroxyindoleacetic acid) can be measured in urine which carry sensitivity of 87-90% and a specificity of 99% for diagnosis [3]. On computerized tomography (CT) scan paragangliomas appear as hypervascular masses with areas of intralesional haemorrhages and necrosis (salt and pepper appearance) [2,6]. CT has 90% sensitivity for localization of extraadrenal tumour [4]. Magnetic resonance imaging characteristically shows paragangliomas as hyperintense masses on T2 weighted images and is more sensitive (93-100%) than CT in detecting extraadrenal tumour [3]. MRI should be performed if CT is negative in a patient with biochemically proven disease [6]. Further, I131-MIBG has a high yield for initial localization [3,7]. Most of retroperitoneal paragangliomas are benign [3]. Malignant paragangliomas may spread hematogenously, lymphatically, and through local invasion: the most common site of metastasis being regional lymph nodes, bone, lung, and liver [3,8]. However, malignant potential in paraganglioma cannot be reliably predicted before development of metastasis or recurrent disease [3].
The traditional treatment of paraganglioma is surgical resection[2]. In view of malignant potential complete excision is always advisable in absence of vascular invasion, regional lymph node or liver metastasis as in our case.
Conclusion
Any retroperitoneal mass with diagnostic difficulty preoperatively and not being able to locate the organ from which it is arising, can be thought of paraganglioma and complete biochemical workup is always advisable to rule out paraganglioma.
[1]. R DeLellis, R Lloyd, P Heitz, Pathology and Genetics. Tumours of Endocrine Organs (IARC WHO Classification of Tumours). Lyon 2004 FranceIARC Press [Google Scholar]
[2]. GI Disick, MA Palese, Extra-adrenal Pheochromocytoma: Diagnosis and Management.Curr Urol Rep 2007 8:83-8.PubMed PMID: 17239321 [Google Scholar]
[3]. JA Lee, QY Duh, Sporadic ParagangliomaWorld J Surg 2008 32:683-87.PubMed PMID: 18224469. [Google Scholar]
[4]. Mustafa Kemal Demirag et al. Inter-aorta-caval Located Tumor: A Case ReportAnn Thorac Cardiovasc Surg. 2011 17:310-12. [Google Scholar]
[5]. GA Kaltsas, GM Besser, AB Grossman, Endocrine Reviews 2004 25(3):458-511.PubMed PMID: 15180952 [Google Scholar]
[6]. EE Elder, G Elder, C Larsson, Pheochromocytoma and functional paraganglioma syndrome: no longer the 10% tumourJ Surg Oncol 2005 89(3):193-201.PubMed PMID: 15719371 [Google Scholar]
[7]. I Ilias, K Pacak, Current approaches and recommended Algorithm for the diagnostic localization of pheochromocytomaJ Clin Endocrinol Metab 2004 89:479-91.PubMed PMID: 14764749 [Google Scholar]
[8]. SE Rha, JY Byun, SE Jung, HJ Chun, HG Lee, JM Lee, Neurogenic tumour in the abdomen: tumour types and imaging characteristics.Radiographic. 2003 23:29-43.PubMed PMID: 12533638 [Google Scholar]