Extended Open Transgastric Necrosectomy (EOTN) as a Safer Procedure for Necrotizing Pancreatitis
Prasad Sasnur1, Ravindra Nidoni2, Ramakanth Baloorkar3, Vikram Sindgikar4, Bharat Shankar5
1Assistant Professor, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur, Karnataka, India.
2Senior Resident, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur, Karnataka, India.
3Associate Professor, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur, Karnataka, India.
4Assistant Professor, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur, Karnataka, India.
5Junior Resident, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravindra Nidoni, Senior Resident, Department of General Surgery, BLDEU’s Shri. B. M. Patil Medical College, Bijapur – 586103, Karnataka, India.
Phone: 09964282803.,
E-mail: ravi3071@gmail.com
The treatment of infected necrotizing pancreatitis has evolved from time to time and the success of surgical intervention depends on the timing of necrosectomy. Bacterial infection occurs in 40–70% of patients with necrotizing pancreatitis. Infection is the main risk factor for mortality among patients with pancreatic necrosis. Timely intervention is generally required for pancreatic necrosis but is now deferred until four weeks after disease onset in order to permit encapsulation and demarcation of the necrotic material. Demarcation facilitates necrosectomy and reduces complications related to the drainage and debridement procedures. The approach to pancreatic necrosectomy has evolved from primary open necrosectomy to minimally-invasive radiologic, surgical and endoscopic procedures. Direct endoscopic necrosectomy is a minimally-invasive technique that was introduced in recent years for the treatment of walled-off necrosis. The pancreas is approached through the posterior wall of stomach and debridement is done.
Necrosectomy, Necrotizing pancreatitis, Transgastric necrosectomy
Introduction
Severe necrotising pancreatitis occurs in 15–20% of patients with acute pancreatitis with the potential for considerable morbidity and significant mortality [1].Early in the course of acute pancreatitis multiple organ failure is the consequence of various inflammatory mediators that are released from the inflammatory process and from activated leukocytes attracted by pancreatic injury [2]. During the late course, systemic septic complications are dominant. Around 80% of deaths in acute pancreatitis are caused by septic complications [3]. Over the course of time, these patients may develop walled off pancreatic necrosis (WOPN) which is characterized by a thickened wall between the necrotic area and adjacent viable tissue. Within the necrotic region, a variable amount of liquefactive necrosis may occur with the resultant collection being a variable mixture of solid and fluid components [4]. For infected necrosis,intervention is generally required but the interventions themselves may cause substantial morbidity [5,6]. The treatment of infected necrotizing pancreatitis has undergone fundamental changes in recent years. Whenever possible,intervention is postponed until the necrosis is demarcated [5,6]. Demarcation facilitates necrosectomy and reduces complications related to the drainage and debridement procedures [6]. EOTN can be a routine procedure for the pancreatic necrosectomy with less morbidity and mortality.
Methods
Total five patients underwent EOTN for necrotizing pancreatitis from January 2013 to May 2013 in BLDEU’s Shri. B. M. Patil medical college, Bijapur, India.
Patient Selection
1) Contrast CT suggesting pancreatic necrosis with demarcation on 4th week.
2) Necrosis in proximity to the posterior wall of stomach with inflammatory adhesion to the capsule of pancreas.
3) Symptomatic.
Technique
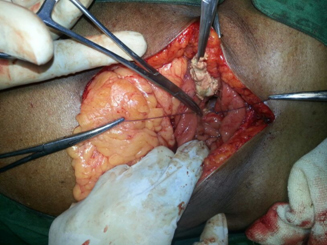
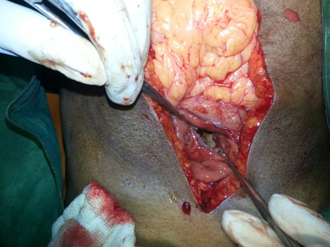
To perform EOTN, the anterior gastric wall is opened opposite the proposed opening in the posterior gastric wall. If possible, the posterior gastrostomy should lie within the area of inflammatory adherence to decrease dependence on a suture anastomosis between the posterior stomach wall and the walled off necrosed pancreas. Preoperative planning based on CT or other imaging data should also take into account such factors as location, bulge, wall thickness, and the proximity of intervening structures. Electrocautery is then used to make at least a 8 cm incision in the combined wall along the transverse axis of the stomach. The necrosed pancreas is carefully debrided [Table/Fig-1]. Hemostasisis achieved. Interrupted non absorbable sutures are placed along the line of opening by suturing the pancreatic capsule with the posterior wall of the stomach to ensure apposition and seal of the gastric and pancreatic walls [Table/Fig-2]. A large bored nasogastric ryeles tube is placed into the cavity created following debridement to irrigate in the postoperative period. The anterior gastrostomy is then closed and the abdominal wall reconstructed. A drain is placed near the stomach wall. The patient is not fed for 3 to 5 days to allow the cavity to collapse and heal prior to filling it with food.
Showing debridement of necrosed pancreas through Posterior gastrostomy.
Showing the stoma between pancreatic capsule and posterior wall of stomach after thorough debridement of necrosed pancreas.
Results
All the five patients recovered well following surgery. There was no single mortality. Unlike patients who underwent open transperitoneal necrosectomy no patient developed complications like pancreatic ascites, enterocutaneous fistula, abscess, bleeding. The mean postoperative hospital stay was 11 days. The general condition and nutrition improved well.
Discussion
The treatment of infected necrotizing pancreatitis has evolved from time to time. The ultimate goal of any treatment approach are to eventually remove all devitalized pancreatic and peripancreatic tissue and evacuate all purulent materials, and to provide continuous drainage to facilitate resolution of the infective process [7,8]. The current options include transperitoneal necrosectomy with multiple tube drainages, endoscopic transgastric necrosectomy, CT guided percutaneous retroperitoneal drainage. Open necrosectomy through the gastrocolic ligament into the lesser sac with multiple tube drainage is the traditional treatment which was commonly used. But it has high mortality and morbidity rates. The enterocutaneous fistula is common because of exposure of pancreatic juices from the remaining functioning pancreas to the already inflamed bowel wall and is commonly noted in gastrocolic approach. The pancreatic fistula is due to exposure of debrided pancreas and its ducts to the peritoneal cavity. The MODS which is a major cause of death following open necrosectomy is due to exposure of toxic collections to the highly absorptive peritoneal surface. These lethal complications can be reduced by adopting transgastric approach where the toxic fluid and the pancreatic secretions are drained into stomach instead of peritoneal cavity.
Endoscopic necrosectomy is a technically challenging procedure that is only be performed by experienced therapeutic endoscopists in high volume urban centres [5]. It requires high level of skills along with sophisticated endoscopic instruments. Apart from technically difficult it has complications like perforation, bleeding and embolism [5]. It is technically not feasible if there is minimal liquefaction of the pancreatic necrosis, with predominant solid debris [5]. In such cases, when interventions are required, the main treatment option is surgical. Many studies have reported the requirement of multiple debridements if endoscopic necrosectomy is adopted [5].
EOTN is a simple procedure which can be performed in all general surgery centres. It has all the advantages of endoscopic necrosectomy as the toxic fluid and the pancreatic secretions are diverted into stomach instead of general peritoneal cavity and hence the morbidity and mortality are less when compared to other open surgical techniques. The other advantage of EOTN is, it gives direct full length visualisation of the necrosed pancreas for debridement.
Conclusion
Extended Open transgastric necrosectomy (EOTN) is a simple procedure which has additional advantages over the other procedures with minimum complications and can be performed at any surgical centre.
[1]. CE Forsmark, J Baillie, AGA Institute technical review on acute pancreatitis.Gastroenterology. 2007 132(5):2022-44. [Google Scholar]
[2]. HG Beger, B Rau, J Mayer, U Pralle, Natural course of acute pancreatitis.World J Surg. 1997 21:130-35. [Google Scholar]
[3]. B Gloor, CA Muller, M Worni, ME Martignoni, W Uhl, MW Buchler, Late mortality in patients with severe acute pancreatitis.Br J Surg. 2001 88:975-79. [Google Scholar]
[4]. TL Bollen, MG Besselink, HC van Santvoort, HG Gooszen, MS Van Leeuwen, Toward an update of the Atlanta classification on acute pancreatitis: review of new and abandoned terms.Pancreas. 2007 35(2):107-13. [Google Scholar]
[5]. Ang Tiing Leong, Current Status of Direct Endoscopic Necrosectomy.Proceedings of Singapore Healthcare. 2012 21(3):179-86. [Google Scholar]
[6]. Hines Joe, W Graham, Donald Endoscopic Transgastricvs Surgical Necrosectomy for Infected Necrotizing Pancreatitis.JAMA. 2012 307(10):1053-61. [Google Scholar]
[7]. B Rau, W Uhl, MW Buchler, HG Beger, Surgical treatment ofinfected necrosis.World J Surg. 1997 21:155-61. [Google Scholar]
[8]. RA Kozarek, TJ Ball, DJ Patterson, PC Freeny, JA Ryan, LW Traverso, Endoscopic transpapillary therapy for disrupted pancreaticduct and peripancreatic fluid collections.Gastroenterology. 1991 100:1362-70. [Google Scholar]