Left Atrial Thrombus in a Neonate with Normal Heart after Sustained Supraventricular Tachycardia
Amirtha Ganesh B1, Ravi Cherian Mathew2
1Professor, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
2Post Graduate, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amirtha Ganesh B, Professor, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Puducherry-607402, India.
Phone: 9443461648,
E-mail: amirtha2001@rediffmail.com
Left Atrial Thrombus is uncommon in neonates. We present a neonate who had Paroxysmal Supraventricular Tachycardia (PSVT), whose echocardiography revealed a large left atrial thrombus which resolved later with treatment. Supra Ventricular Tachycardia (SVT) is not an uncommon event in infants with an incidence of 1:2500.
Echocardiography, Left atrial thrombus, Neonates, Supraventricular tachycardia
Case Report
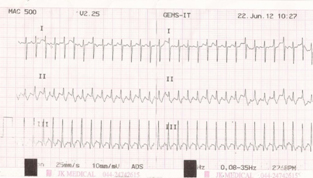
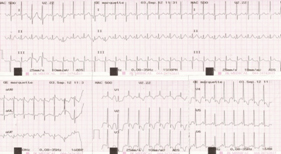
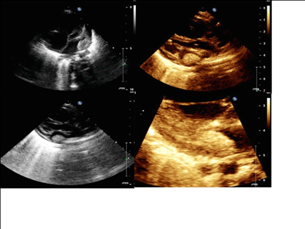
A 28-day-old female preterm neonate, appropriate for gestational age with a birth weight of 1.9 kg reported to our hospital with a history of difficulty in breast feeding, excessive cry, increased precordial activity and increased rate of breathing. On examination the baby was tachypneic with heart rate of 270/min. Electrocardiogram (EKG) revealed the same regular tachycardia with a heart rate of 270/min [Table/Fig-1]. SVT was terminated with adenosine bolus. EKG after termination of tachycardia showed Sinus Rhythm with delta wave with short PR [Table/Fig-2]. Echocardiography revealed a large mobile hyperechoic mass (9 mm x 6 mm) from Left Atrial Appendage (LAA) extending to body of left atrium with some hypoechoic areas inside which was typical of a thrombus rather than a tumour [Table/Fig-3]. Ventricular function was normal, Atrial function couldn’t be assessed. Blood Coagulation parameters revealed Low Protein C Levels (46.7%) and Protein S antigen of 64.2%. Baby was initiated on Enoxoparin 1.5 mg/kg beta-blockers and aspirin.
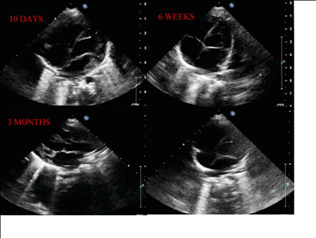
There were no further episodes of SVT and serial echocardiography revealed resolving thrombus. Patient was started on Warfain at 0.5mg/kg. Follow up echocardiography was done at 3rd month and 6th month [Table/Fig-3]. Repeat ECHO at 6th month revealed complete resolution of the thrombus [Table/Fig-4]. After 8 months repeat Protein C antigen was normal (102.4%) and Protein S antigen (97.3%). Beta blockers were stopped as repeat EKG after 6 months showed no Delta waves.
Discussion
SVT in not an uncommon event in infants with an incidence of 1:2500 [1]. Left Atrial thrombus was unexpectedly documented in a neonate after a prolonged SVT episode. Differential diagnosis of a Left Atrial Mass includes cardiac tumours and thrombus.
Cardiac tumours reported in neonates include Rhabdomyoma, Fibromas and Myxomas. Rhabdomyoma are usually located with in the ventricles or the interventricular septum and very rarely in the atrial septum and is usually multiple.
Fibromas diagnosed in infancy are usually large solitary, nonencapsulated mass occupying the intramural position with in the LV septum or free wall, or atria. They cause conduction abnormalities. While myxomas are intracavitary pedunculated masses attached to the fossa ovalis and most commonly located in the right atrium.
In our case the freely mobile hyperechoic mass with hypoechoic areas inside indicating spontaneous lysis, extending from LAA into left atrium cavity. This morphology and its origin typically fits into left atria thrombus and makes other tumour masses unlikely. In neonates thrombosis of the left atrium is very uncommon and rare in LAA. Right Atrial Thrombus has been reported in infants on Central venous catheters but can pass to the Left atrium through
patent foramen ovale. Left Atrial thrombi have been reported after
surgeries in congenital heart disease
In our case left atrial thrombus could be due to Atrial Stand still secondary to SVT.There were no signs of left ventricle dysfunction by echocardiography at any stage. There are no specific guidelines to manage the case like this. The patient was initiated on Enoxaparin and subsequently warfarin. There are no absolute contraindications of Aspirin and Warfarin use in neonates. Guidelines indicated for the same was under specific conditions (ACCP ACC/AHA guidelines) and the side effects and safety were weighed against its usefulness [2,3]. No visible side effects were noted in the neonate during the aspirin and warfarin treatment period. There was a significant resolution of thrombus in the serial echocardiography done during the hospital stay and the patient symptomatically improved. Review after 6 months showed complete resolution of the thrombus. Anticoagulants were stopped after 6 months and repeat prothrombotic factors were normal. Beta-blockers were stopped after 1 year as there were no recurrence.
Narrow QRS tachycardia at 270/min
ECG after termination of SVT showing delta wave
Complete resolution of thrombus at 6 months
Conclusion
This is a rare case with left atria thrombus after an episode of SVT in a neonate with wolf-parkinsons white syndrome. The rarity of the case is left atria Thrombus in an early Infant with Structurally Normal Heart after an episode of SVT. With complete resolution after six months and doubtful contribution of Protein C levels.
[1]. Russo Giulia, Trappan Antonell, A Benettoni, Unusual Left Atrial Appendage thrombus in a neonate with normal heart after sustained supraventricular tachycardia.Int J Cardiol. 2008 131(1):e17-17. [Google Scholar]
[2]. ML Buck, Anticoagulant with warfarin in infants and children.Ann Pharmacother. 1996 30(11):1316-22. [Google Scholar]
[3]. E Schapkaitz, GG Sherman, BF Jacobson, S Haas, HR Buller, V Davies, Paediatric Anticoagulation Guidelines.S Afr J Med. 2012 102(3):171-75. [Google Scholar]