Endodontic Management of a Haemophilic Patient- A Clinical Perspective
Pooja Gupta Dudeja1, Krishan Kumar Dudeja2, Manisha Lakhanpal3, Sartaj Ali4
1Associate Professor, Department of Conservative Dentistry,ESIC Dental College and Hospital, Sector-15, Rohini, Delhi, India.
2Professor, Department of Prosthodontics,Krishna Dental College and Hospital, Ghaziabad, U.P., India.
3Reader, Department of Oral Medicine, Diagnosis and Radiology ,ITS-CDSR, Muradnagar, Ghaziabad, U.P., India.
4Medical Officer, Haemophilia Day Care Centre,Maulana Azad Medical College & Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pooja Gupta Dudeja, Associate Professor, Department of Conservative Dentistry, ESIC Dental College and Hospital, Sector-15, Rohini, Delhi-110 089, India.
Phone: +91-9910327579, +91-9899443032,
E-mail: guptapooja2001@rediffmail.com
Haemophilia and other bleeding disorders remain an enigma to the dentists world over. They not only challenge the skills of dental specialists but also raise the question of how these individuals should be managed emotionally as well as psychologically. The high incidence of dental problems in haemophiliacs is most likely caused by the fear and apprehension not only on the part of the patients but also dentists of inducing bleeding during treatment which can even be life threatening in certain cases. With proper care, diligence and meticulous treatment planning, there is no dental treatment that cannot be performed in such patients. Mild haemophiliacs can be easily managed and can effectively undergo even surgical endodontics without factor replacement therapies. However, severe haemophilia can pose significant health hazard and needs thorough preparation to meet any exigencies arising during the treatment. This case report describes how one such severely haemophilic patient with pain and swelling in the left submandibular region was managed with nonsurgical endodontic treatment in mandibular molar teeth and also discusses the importance of correct methods of diagnosis and various treatment considerations in such patients.
Comprehensive management, Correct diagnosis, Endodontic considerations, Factor VIII, Haemophilia A, Prevention
Case Report
A 16-year-old boy reported at ESIC Dental College and Hospital, Rohini, Delhi with the chief complaint of pain and swelling in lower left back teeth region since 3-4 days. Medical history revealed that the patient was suffering from Haemophilia A. The patient also gave H/o paralysis of left side of body in the year 2000.
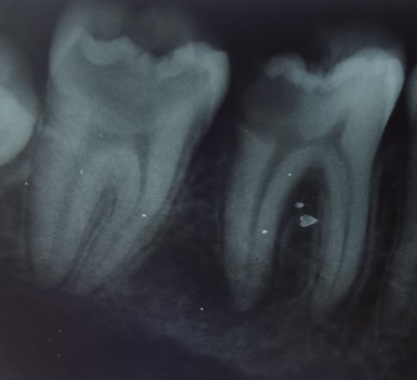
Extra-oral examination revealed swelling over left submandibular region. Intraoral examination revealed carious exposed teeth #36 and #37 [Table/Fig-1]. The teeth were tender on percussion. Radiographic examination revealed periradicular radiolucency surrounding both roots of tooth #36. Pulp responsiveness tests (Heat test and electric pulp test) showed that pulp was responsive in tooth #37 and nonresponsive in tooth #36.
Patient’s haematologist was consulted and it was found out that the patient was a severe haemophiliac with factor VIII concentration less than 1%. The patient first reported with gum bleed at the age of one year and six months and was diagnosed with haemophilia at the age of three years. There was associated family history of haemophilia (maternal cousin suffered from it).
The patient till date had received factor about 60 times in life and had been hospitalized at least 10 times. He also suffers from haemophilic arthropathy in knee and elbow. All the episodes of bleeding were of spontaneous nature, so the haemophilia was of severe type. The patient suffered from approximately 20-25 bleeds per year.
Treatment alternatives were discussed with the patient and informed written consent was obtained prior to procedure. Oral tranexamic acid (500 mg) was prescribed four times a day starting one day prior to the procedure. The patient got I.V infusion of factor VIII one night before so as to build up the level to 50%.
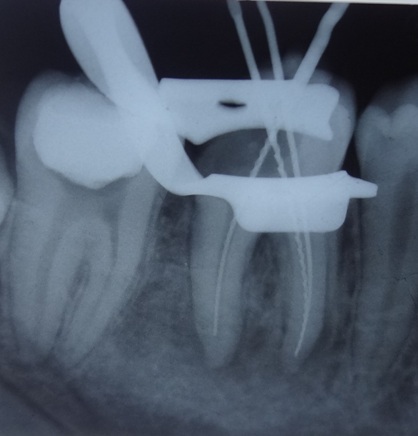
Rubber dam was applied [Table/Fig-2] and access openings were made without local anaesthesia. Tooth #37 was vital, formoacresol was used as a mummifying agent to control and eliminate bleeding from the canals. Working length was estimated and biomechanical preparation of the canals was done taking care to restrict the length within the canal. Root canal obturation and subsequent post-obturation restorations (ketac silver, 3M ESPE) were completed uneventfully [Table/Fig-3].
Local tranexamic acid was applied at the site of procedure whenever there was even slight injury to gingiva. The patient was advised to continue tranexamic acid (500 mg) tablets for five days and was prescribed Cap. Amoxycillin, 500mg eight hourly, Tab Acetaminophen, SOS, and Cap. B- Complex once a day for seven days. The entire duration of treatment was uneventful for the patient. Clinical and radiographic examination at two years recall showed the patient to be completely asymptomatic and comfortable [Table/Fig-4].
Discussion
The most important aspect in managing patients with bleeding disorders is their diagnosis. The first step in diagnosis is taking proper medical and dental history of the patient. Many coagulation disorders are inherited; therefore, eliciting a complete and careful family history is also very important [1]. A complete past and present drug history is also significant [2]. General physical examination of the patient should be done to identify any signs of a bleeding
problem. Purpurae of the skin, several large or deep bruises, evident
haematomas, joint swellings, unexplained nose and gum bleeds all
indicate an underlying bleeding disorder [3].
Laboratory tests
Once the suspicion of a bleeding disorder is raised, the next step is blood investigations. The tests done to evaluate the status of primary haemostasis include:
1. Complete blood count/ platelet count
2. Bleeding Time
These tests evaluate the platelet count and morphology, and function and health of the capillaries [4]. The tests done to evaluate the status of 20 / secondary haemostasis are [Table/Fig-5] [5,6].
• Next step in the diagnosis is Factor assay. This is done to identify whether Factor VIII or Factor IX is deficient. It is of two types:
• QUALITATIVE: This assay tells us which factor (VIII or IX) is deficient but does not tell the level of the deficient factor.
• QUANTITATIVE: This analysis tells the exact %age of deficient factor depending on which the treatment is given.
Management of Haemophilia-A
Management of Haemophilia A requires increasing Factor VIII levels, replacing Factor VIII [7] and inhibiting fibrinolysis. Desmopressin (DDAVP) is a vasopressin receptor agonist that raises factor VIII levels by 3-4 folds by encouraging the body to produce endogenous factor VIII. The dose given is either 0.3 ug/Kg I.V or S.C 30-60 minutes prior to surgical procedure or 300 ug intranasally [8].
For replacement of factor VIII, Cryoprecipitate/ Freeze dried plasma concentrates and Factor VIII concentrates developed by recombinant technology are viable options [9].
Anti-fibrinolytic agents like Tranexamic acid and Epsilon Aminocaprioic Acid (EACA) can be used to protect the formed clot. Tranexamic acid is given systemically in a dose of 1g (30mg/ Kg) orally, four times a day starting atleast one day preoperatively especially for surgical procedures [10]. EACA is a potent inhibitor of initial clot dissolution but Tranexamic acid is 10 times more potent than EACA with fewer side effects.
Endodontic considerations
If done carefully, endodontic treatment usually does not pose any significant risk of bleeding. It is usually preferred over extraction wherever possible. Nerve blocks like inferior alveolar block, lingual infiltration are usually contraindicated until and unless the factor levels are raised above 30% by replacement therapy, else extravasation of blood in the oropharyngeal area or in the pterygoid plexus can be life threatening. Acetaminophen and narcotics are preferably used for postoperative pain while aspirin or any other non steroidal antiinflammatory drug warrants haematological consultation because of their effect on platelet aggregation [11].
Rubber dam should be used to prevent laceration of soft tissue by rotary instruments. But notches should be placed on buccal and lingual surfaces with a bur to ensure proper placement of clamp without injuring the gingiva [12]. It is imperative that the working length of root canals is maintained during endodontic treatment. Sodium hypochlorite should be used for irrigation in all cases followed by use of calcium hydroxide paste to control bleeding [13]. Apex locators should be preferably used for measuring working length of the canal to minimise the need for intra oral periapical (IOPA) radiographs as repeated placement of film can lead to injury and bleeding in the lingual mucosa. Even cotton rolls may cause mucosal bleeding and should be wetted before removal. High speed vacuum evacuators and saliva ejectors can also cause trauma to the floor of mouth and thus lead to haematoma formation. They should be placed by resting them on a gauze swab in the floor of the mouth [11,12,14]. Intracanal injection of local anaesthetic solution containing adrenaline or topical application (paper points) of adrenaline (1:1,000 ratio) can be used to minimise bleeding.
Preoperative IOPA radiograph showing carious exposed teeth #36 and #37
Working length radiograph of tooth #36 with rubber dam in place
Post-obturation radiograph of teeth #36 and #37

Two years recall radiograph

Tests done to assess 2° haemostasis in haemophilia
| S. No. | Test | Status in Haemophilia A |
| 1. | Prothrombin time (PT) | Not Affected |
| 2. | Activated Partial Thromboplastin Time (APTT) | Increases |
| 3. | Thromboplastin Generation Test (TGT) | Increases |
Conclusion
With proper planning and due care, there is no treatment that cannot be performed in haemophiliac patients. The treating dentist should carefully understand the case, take proper history and then execute the treatment. Rather, patient should be educated about the importance of maintaining oral hygiene, use of methods for prevention like fluoride containing toothpaste, floss and inter-dental brushes to prevent dental caries and periodontal disease and pit and fissure sealants to decrease the need for extensive restorative dentistry, which will go a long way in reducing the need for treatment and even emergency visits in such patients.
[1]. PB Lockhart, J Gibson, SH Pond, J Leitch, Dental management considerations for the patient with an acquired coagulopathy. Part 1: Coagulopathies from systemic disease.Br Dent J. 2003 195(8):439-45. [Google Scholar]
[2]. JG Meechan, M Greenwood, General medicine and surgery for dental practitioners. Part 9: haematology and patients with bleeding problems.Br Dent J. 2003 195(6):305-10. [Google Scholar]
[3]. A Gupta, JB Epstein, RJ Cabay, Bleeding disorders of importance in dental care and related patient management.JCDA. 2007 73(1):77-83. [Google Scholar]
[4]. M Greenberg, M Glick, Burkitt’s Oral Medicine – Diagnosis and Treatment 2002 8810th EditionPhiladelphiaJB Lippincott Company [Google Scholar]
[5]. JN Kumar, RA Kumar, R Varadarajan, N Sharma, Speciality dentistry for the haemophiliac: Is there a protocol in place?Indian Journal of Dental Research. 2007 18(2):48-54. [Google Scholar]
[6]. SK Chaudhuri, Concise Medical Physiology. 2004 5th EditionNew Central Book Agency (P) Ltd. [Google Scholar]
[7]. A Coppola, MD Capua, MN Dario, D Minno, MD Palo, E Marrone, Treatment of haemophilia: a review of current advances and ongoing issues.Journal of Blood Medicine. 2010 1:183-95. [Google Scholar]
[8]. NJ Kumar, A Kumar, Varadarajan Kumar, N Sharma, Endodontics for the haemophiliac, a multidisciplinary perspective.J Conserv Dent. 2007 10:59-63. [Google Scholar]
[9]. CS Manno, The promise of third-generation recombinant therapy and gene therapy.Semin Hematol. 2003 40(3):23-8. [Google Scholar]
[10]. JG Vander Bom, Prophylactic treatment for severe haemophilia: Comparison of an intermediate dose to a high dose regimen.Haemophilia. 2002 8(6):753-60. [Google Scholar]
[11]. BE Evans, The role of the dentist in the comprehensive management of haemophilia.Southeast Asian J Trop Med Public Health. 1979 10:285-94. [Google Scholar]
[12]. BE Evans, Consideration in the dental treatment of the haemophiliac patient.J Dent Guid Counc Handicap. 1976 15:3-7. [Google Scholar]
[13]. Guidelines for Dental Treatment of Patients with Inherited Bleeding Disorders. Dental Committee, World Federation of Haemophilia. [Google Scholar]
[14]. BE Evans, LM Aledort, Haemophilia and dental treatment.J Am Dent Assoc. 1978 96:827-34. [Google Scholar]