Primary Cutaneous Actinomycosis:A Case Report
Mohua Bose1, Ranadeep Ghosh2, Kheya Mukherjee3, Loknath Ghoshal4
1Associate Professor, Department of Microbiology, Murshidabad Medical College, Berhampore, West Bengal, India.
2Associate Professor, Department of Microbiology, Nilratan Sircar Medical College, Kolkata, West Bengal, India.
3Associate Professor, Department of Microbiology, Nilratan Sircar Medical College, Kolkata, West Bengal, India.
4PAssociate Professor, Department of Dermatology, Nilratan Sircar Medical College, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohua Bose, Associate Professor, Murshidabad Medical College, Berhampore, West Bengal, India. Phone : 09433185404,
E-mail: mohuabapi@yahoo.com
Actinomycosis is a subacute or chronic suppurative bacterial infection caused by filamentous gram positive, anaerobic to microaerophilic non acid fast bacilli primarily of the genus Actinomyces that normally colonize the mouth, colon and vagina. Primary cutaneous actinomycosis is a rare entity and is generally associated with trauma. We report a case of primary cutaneous actinomycosis of the back and left axilla in a 32-year-old female patient with no suggestive history of trauma.The diagnosis was suggested by the characteristic lesions with multiple discharging sinuses draining sero-sanguinous fluid scattered all over the lesions. Gram positive bacilli with plenty of pus cells were demonstrated in the direct examination of the discharging pus. Diagnosis was confirmed by isolation of the organisms by anaerobic culture giving typical molar tooth colonies. Final confirmation was done by histopathological examination.
Back, Discharging sinuses, Molar tooth colonies
Case Report
A 32-year-old woman presented to the Dermatology out patient department (OPD) of a tertiary care hospital in Kolkata with complaint of a large hard lesion over the left side of the back and another in the left axilla which were painful and the one over the back had multiple openings discharging pus. The patient was a housewife, married with two children and of low middle class socio-economic status. She had no other relevant personal history.
The patient revealed that she was apparently well about six months back. Then she noticed a hard swelling over the back which increased in size gradually spreading laterally and upwards on the left side. The lesion over the axilla appeared later. Initially the lesions were non-tender but later some lesions developed tenderness. The lesion over the back developed multiple swellings which subsequently burst to discharge pus. Some of the openings appeared newly while older ones closed down. The patient had no history of trauma, human bite or barefoot walking. She complained of mild internittent fever. There was no history of any systemic illness Sectionor weight loss and no past history any major medical or surgical illness. There was no significant family history.
General examination of the patient revealed that she was conscious, alert and cooperative. There was mild pallor, but no jaundice or cyanosis. Her pulse rate was 80/minute (regular), blood pressure- 110/80 mm Hg, respiratory rate- 20/minute and body temperature was normal. Liver, spleen and lymph nodes were not palpable. Cardiovascular system, respiratory system and central nervous system (CNS) showed no abnormalities.
On inspection, the patient had a large plaque like lesion about 12 cm x 8 cm over the left side of the back. Overlying skin was scarred in places with papules and nodules. Multiple discharging sinuses draining sero-sanguinous fluid were scattered all over the lesion [Table/Fig-1]. On palpation the lesion was fixed to the underlying muscle and the overlying skin was adherent. The margins were well-defined in some places and progressive in others. There were some satellite nodules which were woody hard in consistency and mostly non tender. Local temperature of the lesions was not raised. The lesion over the left axilla and left upper breast showed multiple tender nodules but no discharging sinuses.
Peripheral blood revealed- Haemoglobin 10.1gm/dl. White blood cell (WBC) count 6300/cu mm with a differential count of neutrophil 70%, lymphocyte 20%, monocyte 3%, eosinophil 6% and basophil 1%. Fasting blood sugar, urea, creatinine and uric acid levels were within normal limits. Liver function test showed normal values. Chest X-ray, electrocardiogram and ultrasonography of the abdomen were within normal limits.
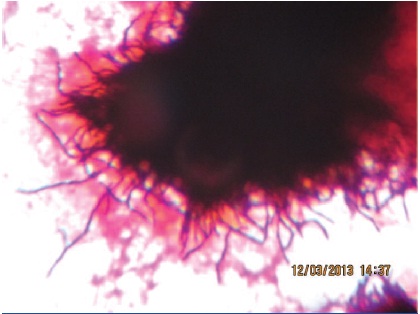
Histopathological examination of lesion biopsy revealed- hyperkeratosis and acanthosis in the epidermis. Mid dermis showed infiltration with multiple microabscesses. Occasional sulphur granules showing typical sun ray appearance were present giving the impression of Actinomycosis.
The pus collected from the discharging sinuses was straw coloured, odourless and serous in consistency. There were no granules in the pus. On direct examination, the pus showed plenty of pus cells and Gram positive bacilli. No Acid fast bacilli were found. KOH mount was prepared but nothing significant was detected. Culture in blood agar showed growth of commensal flora of the skin after overnight aerobic incubation. On anaerobic incubation, typical hard molar tooth appearance colonies were seen after 72 hours [Table/Fig-2]. Gram stainined smear from colony revealed multiple branching gram positive filamentous bacilli suggestive of Actinomyces species [Table/Fig-3].
The patient was admitted and treated with injection Benzyl penicillin eight million units four times daily and tablet Cotrimoxazole twice daily for 20 days. But as she was unwilling to continue with injection, she was put on oral therapy with Cotrimoxazole twice daily and amoxycillin 500mg four times daily and discharged with an advice to report to the Dermatology OPD after four weeks and monthly thereafter. The patient has since been reporting at the OPD regularly for the last two months and is still continuing the same treatment. There has been gross improvement in her condition.The sinuses have healed with fibrosis. Presently there is no induration, discharge or appearance of fresh lesions. Systemic manifestations are also absent and the patient has recovered considerably.
Discussion
Actinomycosis is an indolent, slowly progressive infection caused by anaerobic or microaerophilic bacteria, primarily of the genus Actinomyces, that colonize the mouth, colon, and vagina. It is characterised by contiguous spread, suppurative and granulomatous 4inflammation and formation of multiple abscesses and dischaging sinuses draining sero-sanguinous fluid and sulphur granules. The most common clinical types are cervicofacial, thoracic, abdominal and, in women pelvic. The disease has no geographic boundaries and occurs throughout life, with a peak incidence in the middle decades. Males have a threefold higher incidence than females [1].
Actinomycosis has been called “the most misdiagnosed disease”. It remains a diagnostic challenge. It is most commonly caused by the gram-positive bacterium Actinomyces israelii. Other species that are less common causes of Actinomycosis include A. naeslundii/viscosus complex, A. odontolyticus, A. meyeri, and A. gerencseriae [2].The disease is almost always endogenous in origin. A pivotal step in the pathogenesis is disruption of the mucosal barrier. As the causative agents are non-virulent, they require a break in the integrity of the mucous membranes and the presence of devitalized tissues to invade deeper body structures and cause disease. Oral and cervicofacial disease is frequently associated with dental procedures, trauma, oral surgery, and head and neck radiotherapy or oncologic surgical procedures. Likewise, pulmonary infections often arise in the setting of aspiration, and abdominal infection is usually preceded by conditions that result in loss of mucosal integrity, such as gastrointestinal surgery, diverticulitis, appendicitis, or foreign bodies (e.g.,fish bones). Cutaneous localisation of actinomyces generally occurs by contaguity of underlying foci by direct inoculation or by haematogenous spread during septicaemic stage of infection. Recognition of factors that enable bacterial entry into deep tissues however, may be absent. The lack of such a history should not prevent consideration of this disease when the clinical circumstance is appropriate.
Primary cutaneous actinomycosis is a rare entity and requires a high index of suspicion. Primary disease of the extremities is uncommon because of the exclusive endogenous habitat of the causative organism [3-7]. Most of the cases reported give a clear history of trauma, either human bite or a perforating injury with contamination from outside [3]. Haematogenous spread has also been suggested [8]. In our patient there was no history of trauma and so the exact pathogenesis remains unclear. A similar case reported from Delhi had no history of trauma [9]. Though there were no grains obtained in our case, the diagnosis was suggested from the typical lesions. The diagnosis in our patient was further confirmed by isolation of the organisms by anaerobic culture giving typical molar tooth colonies. Histopathological examination of the lesions helped us to reach a final confirmed diagnosis.
Lesion over the back showing multiple nodules and some discharging sinuses

“Molar tooth” appearance of colonies on Blood Agar (Anaerobic Culture in Candle Jar)

Gram stained smear from colony (100x) showing multiple branching Gram positive filamentous bacilli
Conclusion
Our case stresses the need to have a high degree of suspiscion of actinomycosis in clinically suggestive cases even without a history of trauma. Attempts should be made to diagnose such cases by culture and histopathological examination so that we do not miss the diagnosis of such a case.
Aknowledegement
Our special thanks to Professor Mandira Banerjee, Head of the Department, Department of Microbiology, Nilratan Sircar Medical College, for giving all her support to us for the work. We also extend our sincere thanks to all other faculty members, technical and non-technical staff of the Department of Microbiology, Nilratan Sircar Medical College for all the support given by them to carry out this work.
[1]. TA Russo, Actinomycosis. In: Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J, editors.Harrison’s Principles of Internal Medicine. 2012 18th EditionMcGraw Hill [Google Scholar]
[2]. TA Russo, Agents of Actinomycosis. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Bennett & Dolin: Principles and Practice of Infectious Diseases. 2005 6th EditionPhiladelphiaChurchill Livingstone, An Imprint of Elsevier [Google Scholar]
[3]. SL Reiner, JM Harrelsen, SE Miller, GB Hill, HA Gallis, Primary actinomycosis of an extremity: a case report and review.Rev Infect Dis. 1987 9(3):581-89. [Google Scholar]
[4]. K Sardana, V Mendiratta, RC Sharma, A suspected case of primary cutaneous actinomycosis on the buttock.J Dermatol. 2001 28(5):276-78. [Google Scholar]
[5]. SH Wee, SN Chang, JY Shim, CC Cheek, SL Chun, WH Park, A case of primary cutaneous actinomycosis.J Dermatol. 2000 27(10):651-54. [Google Scholar]
[6]. SC Metgud, Primary cutaneous actinomycosis : a rare soft tissue infection.Indian Journal of Medical Micribiology. 2008 26(2):184-86. [Google Scholar]
[7]. D Patil, B Siddaramappa, BS Manjunathswamy, AM Pandit, S Dastikop, C Fernandes, Primary cutaneous actinomycosis. Int J Dermatol. 2008 47(12):1271-3. [Google Scholar]
[8]. CA Butas, SE Read, Re Coleman, M Abravoltch, Disseminated actinomycosis.Can Med Assoc J. 1970 103(10):1069-71. [Google Scholar]
[9]. D Roy, P Gupta Roy, PK Misra, An interesting case of primary cutaneous actinomycosis.Dermatology Online Journal. 2003 9(5):17 [Google Scholar]