Verruciform xanthoma is an uncommon benign lesion of undetermined aetiology. It is a superficial normo-lipemic xanthoma, probably reflecting a multifactorial reactive and dystrophic process. Its clinical and pathological recognition and correct diagnosis is critical because it can occur in conjunction with other systemic and cutaneous inflammatory diseases; therefore, it necessitates further clinical assessment. We, hereby report a rare case of verruciform xanthoma in 46-year-old male patient with history of leukemia with emphasis on need of vigilant comprehensive analysis of clinicopathological and immunohistohemical finding to arrive at definitive diagnosis and for better understanding of pathogenesis.
Immunohistochemistry, Keratin plugging, Lipids, Verruciform xanthoma
Case Report
A 46-year-old male patient reported with a chief complaint of white patch in the palatal region of mouth since 2-3 yr. He gave history of burning sensation to spicy foods and alcohol. Patient has undergone treatment for Chronic Myeloid Leukemia 10 year back. Intra Oral Examination revealed white non scrappable patch measuring 1cm X 2cm extending from interdental papilla of maxillary left first and second premolar towards the midline and on left side of corner of mouth also [Table/Fig-1] . Provisional diagnosis of verrucuous carcinoma was made. Routine hematological examination was found out to be normal. Differential diagnosis of squamous papilloma, leukoplakia, verrucous carcinoma and squamous cell carcinoma was considered.
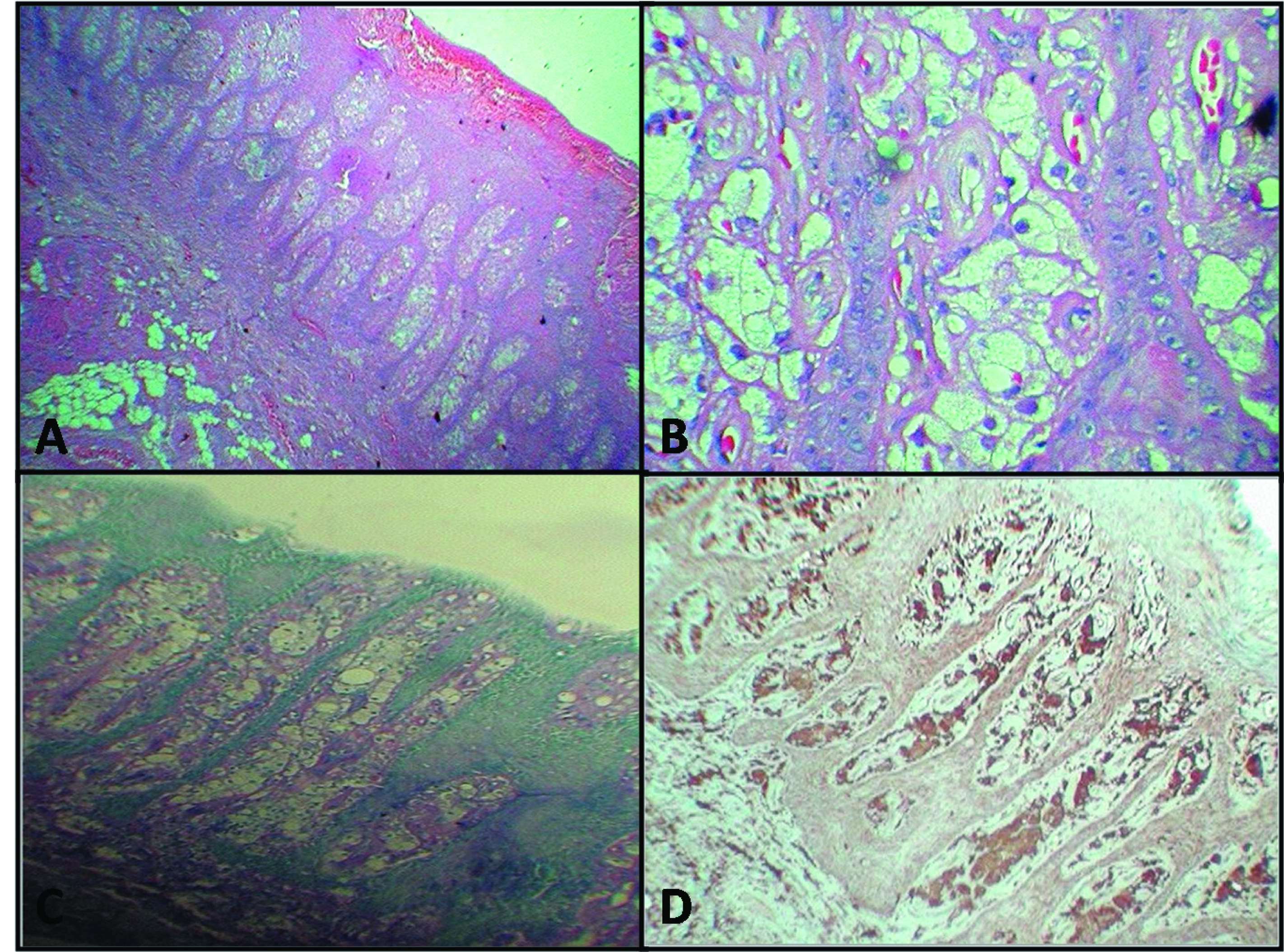
Incisional biopsy was performed under local anesthesia and submitted for histopathological examination. It showed hyperparakeratinized stratified squamous epithelium with elongated rete pegs. Parakeratin plugging was seen in many areas. Underlying connective tissue showed papillae of variable length and thickness extending close to the surface epithelium and accumulation of numerous large macrophages with foamy cytoplasm (Xanthoma cells)[Table/Fig-2a,2b] . The reticular portion of the connective tissue was free of these foamy macrophages. Focal areas of acute and chronic inflammatory cells, numerous budding capillaries along with extravasated RBC’s were seen. All foam cells were PAS positive diastase resistant [Table/Fig-2c] . The immunohistochemical staining for CD68 was positive for the foamy macrophages [Table/Fig-2d] . In the evidence of these features, a confirmatory diagnosis of Sectionverruciform xanthoma was made. The treatment was performed under local anaesthesia. The whole lesion was excised in one piece during excisional biopsy. On follow up, neither malignant transformation nor recurrence of the lesion has been reported.
Photograph showing white patch in relation to interdental area of maxillary left premolars

Photomicrograph showing: A) Papillary projections lined by stratified epithelium and core of connective tissue extending into the epithelium. (H & E, 4x); B) Large swollen cells with granular cytoplasm with eccentrically placed nuclei (foam cells or xanthoma cells) that filled the connective tissue papillae between the epithelial rete ridges. The cells show (H&E,40x); C) PAS positive diastase resistant foam cells; D) Foam cells with strong cytoplasmic CD68 immunostaining. The epithelial cells were negative (IHC stain 10x)
Discussion
Verruciform xanthoma (VX) is a rare benign lesion, primarily of the oral mucosa that can also affect skin and genital mucosa also. It accounts for 0.025-0.05% of all pathology cases [1] .
Based on worldwide survey of 282 cases, it is observed that below the age of 50, male to female ratio is 1.6:1 and this ratio is reversed after the age of 50 in favour of females, where the male to female ratio is 0.8:1[2,3] . Approximately, 75% of all oral VX lesions occur on the masticatory mucosa of the palate, gingiva or the alveolar ridge whereas few cases have also been reported on the floor of mouth, buccal mucosa and tongue [4,5]. Present case also occurred on posterior region of palate in a 46-year-old male patient in accordance to literature.
Clinically oral VX may bear a resemblance to verrucous carcinoma, squamous papilloma, verruca vulgaris, or a mucosal fibroma [2] .
Thus, histopathological confirmation is required. However, verrucous carcinoma can be distinguished from VX, by the presence of invasive epithelial proliferation, cellular atypia, and the lack of foamy histiocytic infiltrate. Less aggressive lesions such as squamous cell papilloma, verruca vulgaris, and condyloma acuminatum does not contain lipid-laden macrophages and they exhibit varying degree of viral cytopathic change, so called koilocytic change, which are known to be absent in VX. In addition to this, the rete ridges in condyloma acuminatum and verrucous carcinoma tend to be bulbous, as opposed to the long and slender ones in VX [3] .
Three histological subtypes (types A, B, and C) have been described based on the texture of the surface epithelium. Lesions of the verrucous type (A) have hyperparakeratosis, verrucous type acanthosis, and elongation of the rete ridges. The papillary form (B) has many finger-like projections composed of stratified squamous epithelium containing connective tissue cores. In the flat type (C), mild acanthosis and subtle thin parakeratosis with variable elongation of rete ridges are commonly observed [4] .
VX aetiology is unknown, but several inciting agents, including cutaneous trauma, could play a role. Ide et al., suggested some possible oral agents as wet microenvironment, periodontal pathogens, mechanical stimuli, tobacco, alcohol, drugs, sensitizing or allergic substances of foodstuffs and dental materials. It may be associated with localized inflammation, Immunologic factors and viral aetiologies have been also suggested [5] . According to Shafer, macrophages are responsible for the initiation of process. As the epithelium degenerates due to local trauma, there is accumulation of epithelial breakdown products which induce inflammatory response and subsequent release of lipid material through the epithelium that finally is scavenged by the macrophages. They also suggested a local irritant as the initiator of the process [1] .
However, Hu et al., suggested that the reciprocal induction between epithelial and mesenchymal cells due to destruction of basement membrane by matrix metalloproteinases (MMP-2 and 9) is responsible for the initiation of the process [6] . Rowden et al., were of the opinion that VX belongs to new category of ‘ non-X histiocytosis’ in which the presence of Langerhans cells suggested in immunological pathogenesis [7] . Santa Cruz and Martin also suggested that a viral cause might be possible. Although, many ultrastructural studies has been conducted, viral particles have been not seen in either the epidermal or epithelial cells [8] .
Nowparast et al., [9] suggested that foam cells may be responsible for verrucous and papillary architecture which effects the nutrition and metabolism of the epithelial cells, leading to the hyperkeratotic change. The lipid material found in the xanthoma cells could be of the same nature as that found within foam cells in the chronic inflammatory reactions such as periapical cysts and dental granuloma, where epithelial degeneration is common. Travis et al., [10] also supported that the epithelial hyperplasia is a secondary event. Macrophages are known to produce a variety of growth factors that might play a role in inducing epithelial hyperplasia.
Many histochemical, immunohistological, and ultrastructural studies have been done so far, but even today pathogenesis is obscure and needs to be clarified [1].
The diagnostic hallmark of VX is the presence of xanthoma cells within the connective tissue papillae [2] . In our case also, large number of xanthoma cells and neutrophilic infiltrate is seen which is in accordance with the finding of Weedon D et al., [11] and the cells present within the connective tissue papilla are PAS positive diastase resistant and CD 68 positive, which is confirmatory for presence of xanthoma cells and in accordance with the finding of Weedon D et al.,[11] .
There is a controversy regarding exact origin of foam cells. Some author’s favour that it is lineage of monocytes/macrophages whereas others believe that lipid found in the xanthoma cells is similar to as seen in other inflammatory reactions [12,13] . Present case, showed strong immunoreactivity for CD68. CD68 is a cell marker confirming the possible role of macrophages in the formation of foam cells [1] . The treatment of choice is complete surgical excision which is very effective with no recurrence. Histopathological examination of the biopsies should be performed to distinguish VX from other verrucous lesions.
Conclusion
VX is a chronic reactive process that must be differentiated from diverse epidermal, hyperplastic lesions, yet histopathologically it still poses a challenge to the understanding of its pathogenesis.
[1]. WG Shafer, Verruciform xanthomaOral Surg Oral Med Oral Pathol 1971 31(6):784-89. [Google Scholar]
[2]. CH Yu, TC Tsai, JT Wang, BY Liu, YP Wang, A Sun, Oral verruciform xanthoma: a clinicopathologic study of 15 cases.J Formos Med Assoc 2007 106:141-47. [Google Scholar]
[3]. HP Philipsen, PA Reichart, T Takata, I Ogawa, Verruciform Xanthoma biological profile of 282 oral lesions based on a literature survey with a nine new cases from japanOral Oncol 2003 39:325-36. [Google Scholar]
[4]. S Bhalerao, P Bhat, R Chhabra, A Tamgadge, Verruciform xanthoma of buccal mucosa: A case report with review of literature.Contemp Clin Dent 2012 3(2):v-59. [Google Scholar]
[5]. F Ide, K Obara, H Yamada, K Mishima, I v, K Kusama, Cellular basis of verruciform xanthoma: Immunohistochemical and ultrastructural characterization.Oral Dis 2008 14:150-7. [Google Scholar]
[6]. JA Hu, Y Li, S Li, Verruciform xanthoma of the oral cavity: clinicopathological study relating to pathogenesis. Report of three cases.APMIS. 2005 113:629-34. [Google Scholar]
[7]. D Rowden, G Lovas, W Shaefer, K Shiekh, Langerhan Cell in the verruciform xanthoma. An immunoperoxidase study of 10 Oral LesionsJ Oral pathol 1986 15:48-53. [Google Scholar]
[8]. DJ Santa Cruz, SA Martin, Verruciform xanthoma of the vulva: Report of two casesAm J Clin Pathol 1979 71:224-8. [Google Scholar]
[9]. B NowParast, FV Howell, GM Rick, Verruciform Xanthoma: A clinicopathologic review and report of 50 cases.Oral Surg Oral Med Oral Pathol 1981 51:619-25. [Google Scholar]
[10]. WD Travis, GE Davis, M Tsokos, R Lebovics, HF Merrick, SP Miller, Multifocal Verruciform Xanthoma of the upper aerodigestive tract in a child with a systemic lipid storage disease.Am J Surg Pathol 1989 13:309-16. [Google Scholar]
[11]. D Weedon, G Strutton, Weedon’s Skin Pathology. Cutaneous infiltrates – nonlymphoid. 2002 2nd EditionNew YorkChurchill Livingstone:2002-964. [Google Scholar]
[12]. Kimura. Verruciform xanthoma of the scrotumArchives of Dermatology 1984 120:1378-79. [Google Scholar]
[13]. KA Mostafa, T Takata, I Ogawa, N Ijuhin, H Nikai, Verruciform xanthoma of the oral mucosa: a clinicopathological study with immunohistochemical findings relating to pathogenesisVirchows Archiv 1993 423:243-48. [Google Scholar]