Mandibular Metastasis of Thyroid Carcinoma: A Case Report
Lavanya C1, Ranganathan K2, Veerabahu M3
1Senior lecturer, Department of Oral and Maxillofacial Pathology, Ragas Dental College and Hospital, Chennai, India.
2Head of the Department, Department of Oral and Maxillofacial Pathology, Ragas Dental College and Hospital, Chennai, India.
3Head of the Department, Department of Oral and Maxillofacial Surgery, Ragas Dental College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lavanya.C, F-2,Kumanan Apts, I Avenue, Ashok Nagar, Chennai -600083, India. E-mail : lavanyac2210@yahoo.com
Metastatic carcinomas to the jaw bones are uncommon and comprise to about 1% of all malignant oral neoplasms. It may be the first indication of an unknown malignancy from a distant primary site which is usually associated with poor prognosis. We report a rare case of thyroid carcinoma metastatic to the mandible in a 76-year-old elderly male patient in which the lesion was asymptomatic. Microscopic examination revealed a tumour structure consisting of cords and islands of infiltrating epithelium. The immunohistochemical marker, thyroid transcription factor -1 was done which showed a positive staining by the follicular cells. The tumour was diagnosed as metastatic follicular thyroid carcinoma. It should be emphasized that histopathological diagnosis along with panel of markers play an important role in diagnosing the site of origin of bone metastasis and these lesions should be included in the differential diagnosis of asymptomatic jaw lesions.
Mandible, Metastasis, Thyroid carcinoma
Case Report
A 76-year-old male patient was referred to the Department of Oral Pathology and Microbiology at Ragas Dental College and Hospital, Chennai, India with a slow growing painless swelling in the left side body of the mandible with unknown duration. The patient was partially edentulous and underwent extraction of infected 36 and 37 due to dental caries six months earlier. The patient on general examination was moderately built, without any relevant medical history and no known habits like smoking , alcohol consumption or pan chewing. Clinical examination revealed a well-defined, firm ,oval swelling measuring 3x3 cm extending horizontally from mid-portion of the left body of the mandible towards angle of the mandible, vertically from inferior border of the mandible to lower middle third of the face. The skin over the swelling appeared normal [Table/Fig-1] . Intra orally,the swelling was solitary, sessile and extended from premolar to molar region. On palpation, it was non-tender, soft to firm in consistency with buccal cortical plate expansion.
Panoramic radiograph revealed a unilocular radiolucency with ill-defined border on the left body of the mandible [Table/Fig-2] . Panoramic section of cone beam computed tomography scan showed a large radiolucent area with irregular borders in relation to edentulous 36, 37 region, not involving left inferior alveolar canal. On further examination, coronal section of the CT revealed an osteolytic expansile lesion with buccal cortical plate erosion, but lingual cortex was intact [Table/Fig-3and4] . Based on the clinical and radiographic findings, a provisional diagnosis of odontogenic tumour was considered.
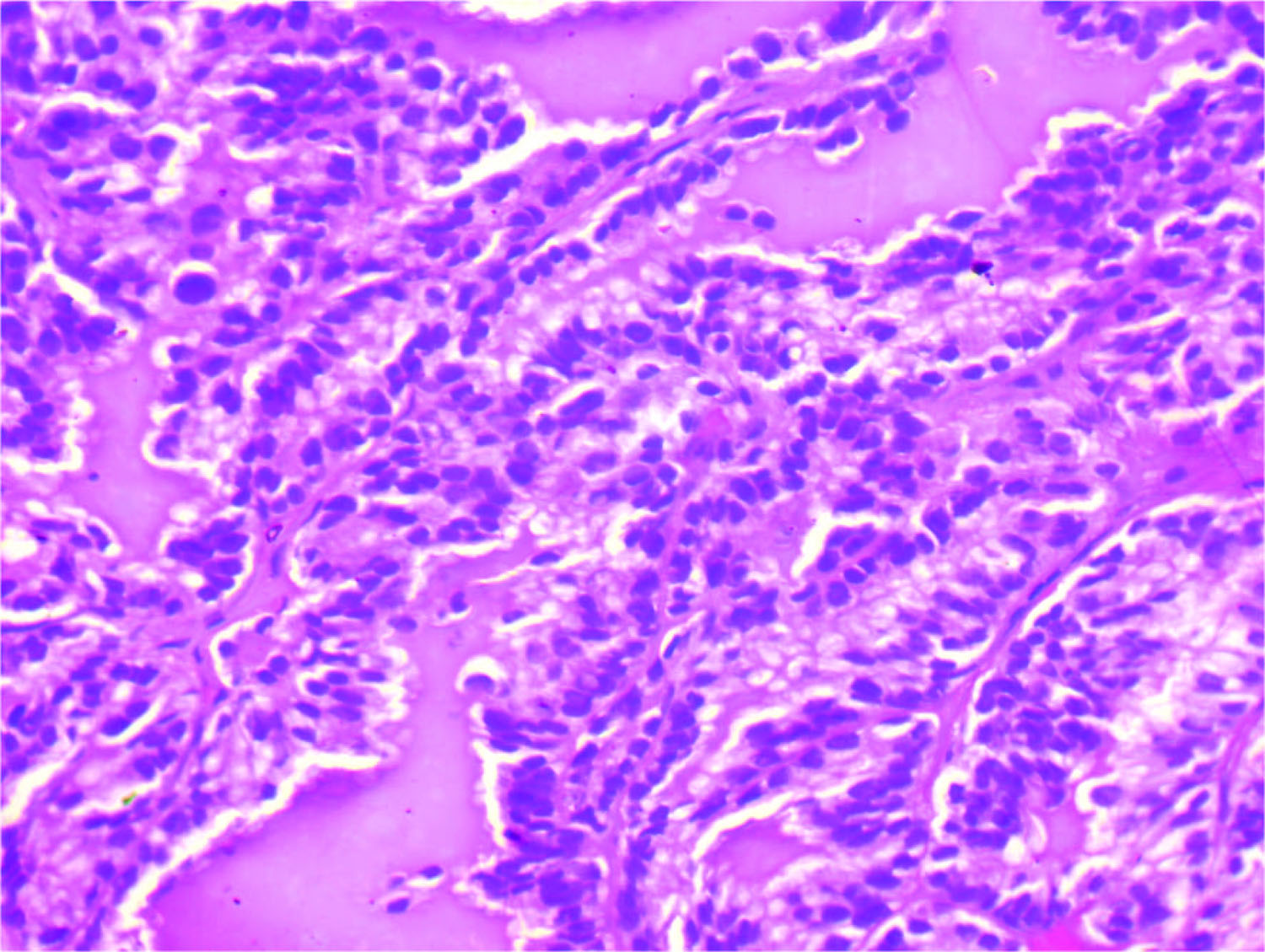
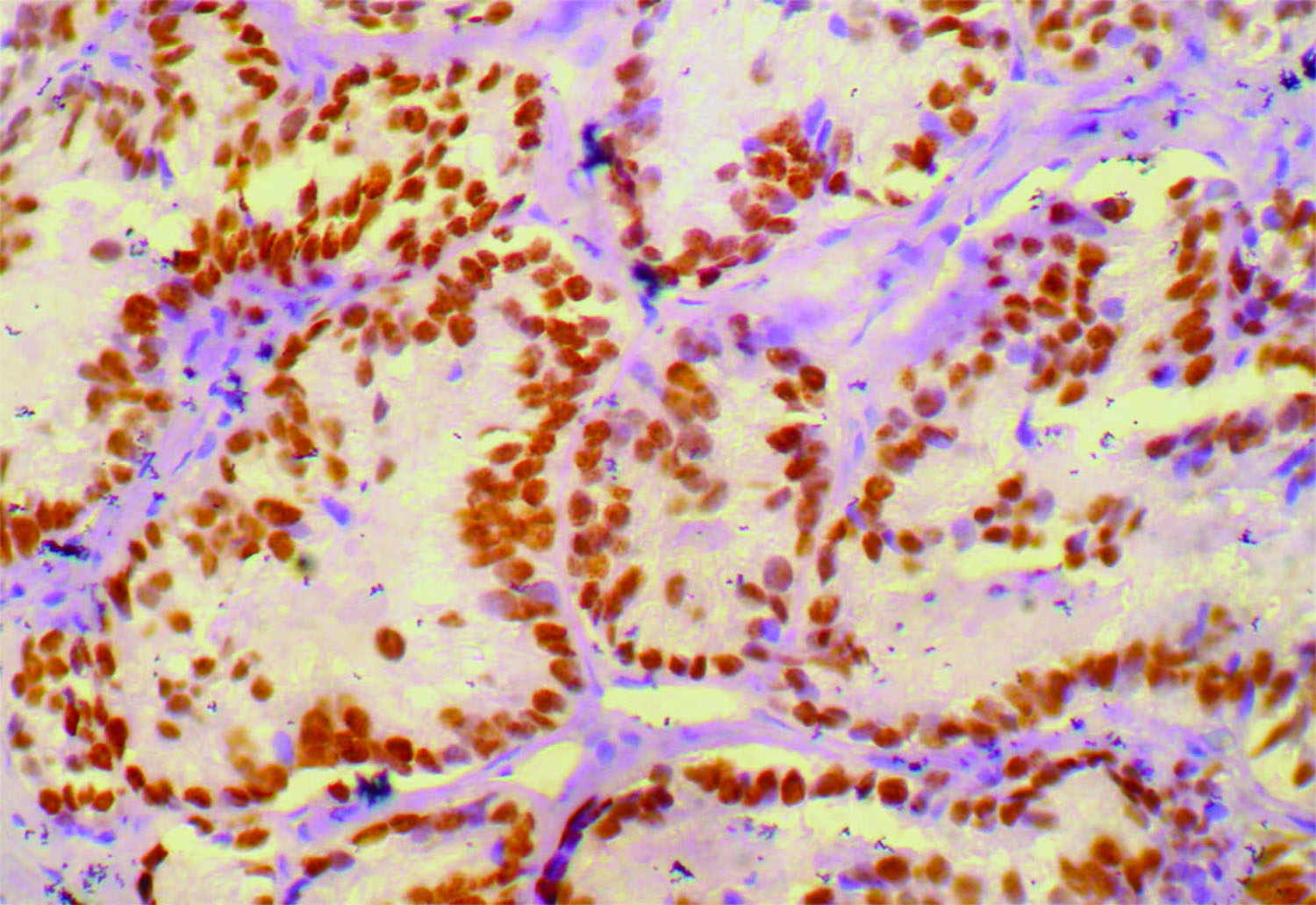
An incisional biopsy was performed. The haematoxylin and eosin stained tissue section showed a tumour consisting of cords and islands of infiltrating glandular epithelium. The peripheral cells in the cords and islands were columnar with eosinophilic cytoplasm and the central cells were vacuolated. The epithelium also exhibited Sectionfocal areas of ductal proliferation with eosinophilic coagulum on the luminal side [Table/Fig-5,6and7]. The eosinophilic secretory material and the well developed duct like structures leads to the provisional diagnosis of adenocarcinoma . Immunohistochemistry was done by immunohistochemical marker ,Thyroid Transcription factor (TTF-1) which showed an isolated positive staining by the cells [Table/Fig-8] and we came to the diagnosis of metastatic thyroid carcinoma, the follicular type. The patient was referred to an oncologist for further management.
Clinical picture of the patient

Panoramic radiograph showing radiolucency in the 36, 37 region
CT scan shows radiolucent area in the region of 36, 37
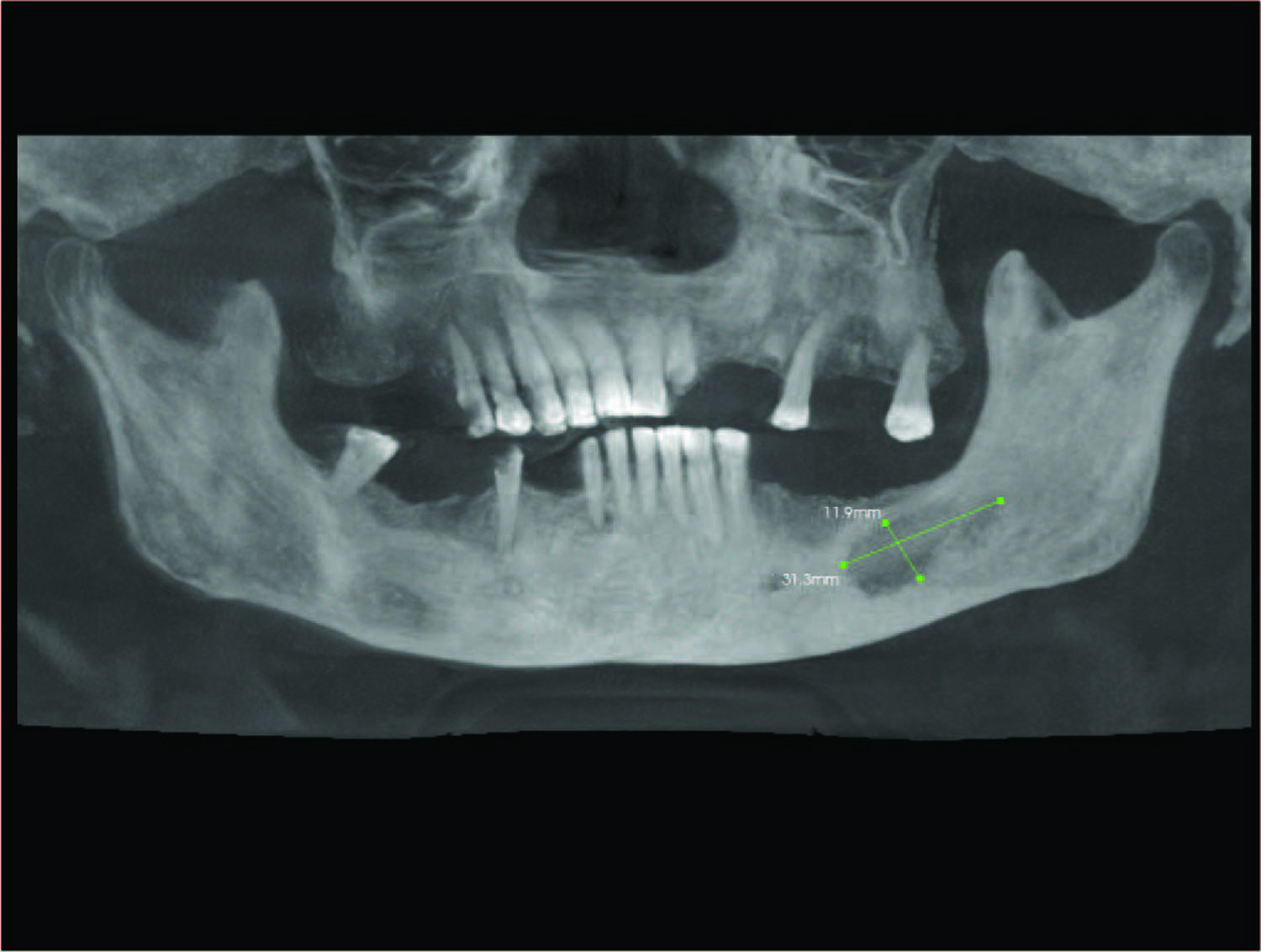
CT scan showing erosion of buccal cortical plate

Haematoxylin and eosin (original magnification 10 x) section showing ductal proliferation of epithelium with eosinophilic coagulum on the luminal side

Haematoxylin and eosin (original magnification 40 x) section showing ductal proliferation of epithelium with eosinophilic coagulum on the luminal side
Immunohistochemical staining of Thyroid transcriptional factor-1 by follicular cells
Discussion
Metastatic carcinomas to the oral region are rare and constitutes to about 1% of all malignant oral neoplasms [1]. Metastasis involving jaw bones are less when compared with other bones such as the vertebrae, ribs, pelvis and the skull owning to decrease in blood vessels and red bone marrow with age[2]. These metastatic tumours are clinically significant, since their appearance may be the first indication of an undiscovered malignancy at a distant primary site, or the first evidence of dissemination of a known tumour from its primary site [3]. Among the well -differentiated thyroid cancer, distant metastasis occurs to about 7%-23% of patients. Thyroid cancer commonly metastasis to lungs and bones [4]. In the oral cavity , the jaw bones are more commonly affected than the soft tissues with the molar-premolar area of the mandible being the frequently involved site [1,5]. In 23-25 % cases, oral metastases is the first sign or indication of an occult malignancy ,as was seen in our case [6].
In an Indian study, Muttagi et al., reported that in the first to second decade of life, the primary site for oral metastatic colonisation were from adrenal, brain and bone, where as in older age group it was from breast and thyroid [5]. According to studies from western literature, sources of metastasis show gender variation. The primary site of origin was lungs ,prostrate, kidney in males while in females it was breast, adrenal and female genital organ. Metastatic lesions from thyroid and adrenals preferred the jaw bones when compared to soft tissues [6]. Patient complaining of numb chin or mental nerve neuropathy should be considered for possibility of metastatic disease in mandible. Postextraction site can also serve as a promoting factor for metastasis [6,7]. Similar case report by Bhadage et al., observed that a two month latency period existed between extraction and the development of metastasis [8]. Most common radiographic appearance of metastatic disease could be a lytic radiolucent lesion with ill-defined margins. Occasionally, osteoblastic lesions with radiopacity were observed[6]. Similarly , Kaveri et al., reported that the radiographic presentation can range from lytic to radio-opaque lesion with ill-defined borders [9]. Most of these clinical findings can be correlated in our study.
Follicular thyroid cancer is a well- differentiated tumour that arise from the follicular cells of thyroid gland ,with incidences ranging from 7% to 28% and is the common histologic origin of bone metastasis [5]. When compared with follicular thyroid carcinoma, papillary thyroid carcinoma is less likely to metastasize to bones [4]. Recent studies on the mechanisms responsible for metastatic tumour growth in bone include an alteration in the physiologic balance between bone formation and resorption. Tumours produce many factors that stimulate osteolysis –parathyroid hormone-related protein (PTHrP), interleukins, IL-11, IL-8, IL-6, and receptor activator of nuclear factor-κ B ligand (RANKL). Bone is a rich source of matrixembedded growth factors such as IGF and TGF-b, these cytokines are released upon osteolysis and act upon the invading tumour cells to promote the induction of osteoclast-promoting factors [5,10]. Histopathologically, a well-differentiated tumour exhibiting follicles is associated with a good prognosis than a poorly differentiated lesion with solid growth and absence of follicles [11].
The optimal treatment for differentiated thyroid cancer includes thyroidectomy and radiotherapy. In cases of asymptomatic bone metastasis, detection can be made by thyroglobulin measurement and radioiodine scans. Reports have shown that clinical diagnosis of bone metastasis in differentiated thyroid carcinoma were 4-13%. Since there is difficulty in diagnosing bone lesions, biopsy is mandatory. Histological diagnosis is important in diagnosing and differentiating primary intraoral malignancies from metastasis of unknown primary tumours. An overall ten year survival rate of patients with distant metastasis from differentiated thyroid carcinoma was 13 -21 %[12].
Conclusion
Due to the rarity of the disease the histopathological diagnosis of jaw bone metastasis is challenging in recognising and determining the site of origin of the lesion. It should be emphasized that histopathological diagnosis along with panel of markers play an important role in diagnosing the site of origin of bone metastasis and these lesions should be included in the differential diagnosis of asymptomatic jaw lesions.
Acknowledgement
We thank our Principal Dr. S. Ramachandran, for encouraging and facilitating the publication of this case report.
[1]. RIF Van der Waal, J Buter, I Van der Waal, Oral metastasis : report of 24 cases.Br J Oral Maxillofac Surg 2003 41:3-6. [Google Scholar]
[2]. N Zachariades, Neoplasms metastatic to mouth, jaws and surrounding tissues.J Cranio Max Fac Surg 1989 17:283-90. [Google Scholar]
[3]. S Anil, PM Lal, DS Gill, VT Beena, Metastasis of thyroid carcinoma to the mandible- Case ReportAust Dent J. 1999 44:54-57. [Google Scholar]
[4]. MY Do, Y Rhee, DJ Kim, CS Kim, KH Nam, CW Ahn, Clinical features of bone metastases resulting from thyroid cancer : A review of 28 patients over a 20 year period.Endocrine journal 2005 52:701-07. [Google Scholar]
[5]. SS Muttagi, P Chaturvedi, A D’Cruz, S Kane, D Chaukar, P Pai, Metastatic tumours to the jaw bones : Retrospective analysis from an Indian tertiary referral center.Indian J Cancer 2011 48:234-39. [Google Scholar]
[6]. A Hirshberg, A Shnaiderman-Shapiro, I Kaplan, B Rannan, Metastatic tumours to the oral cavity –Pathogenesis and analysis of 673 cases.Oral Oncol 2008 44:743-52. [Google Scholar]
[7]. Lim SY, Kim SA, Ahn SG, Kim HK, Kim SG, Hwang HK, Metastatic tumours to the jaws and oral soft tissues: a retrospective analysis of 41 Korean patientsInt J Oral Maxillofac Surg 2006 35:412-15. [Google Scholar]
[8]. CJ Bhadage, S Vaishampayan, H Umarji, Mandibular metastasis in a patient with follicular carcinoma of thyroid.Contemp Clin Dent 2012 3:212-14. [Google Scholar]
[9]. H Kaveri, VA Punnya, TS Amsavardani, Metastatic thyroid carcinoma to the mandible.J Oral Maxillofac Path 2007 11:32-34. [Google Scholar]
[10]. TA Guise, KS Mohammad, G Clines, EG Stebbins, DH Wong, LS Higgins, Basic mechanisms responsible for osteolytic and osteoblastic bone metastases.Clin Cancer Res 2006 12:6213-16. [Google Scholar]
[11]. PM Vishveshwaraiah, A Mukunda, KK Laxminarayana, K Kasim, Metastatic follicular thyroid carcinoma to the body of the mandible mimicking an odontogenic tumour.J Can Res Ther 2013 9:320-23. [Google Scholar]
[12]. AG Pittas, M Adle, M Fazzari, S Tickoo, J Rosai, SM Larson, Bone metastasis from thyroid Carcinoma: Clinical characteristics and prognostic variables in one hundred forty six patientsThyroid. 2000 10:261-68. [Google Scholar]