Lymphangioma Involving the Foetal Lower Limb, A Rare Condition Diagnosed on Prenatal Ultrasound
Sunil Kumar K S1, Suchith Hoblidar2, Ramesh Kumar R3, Rathnamala M Desai4, Nayana A Yelamali5
1Associate Professor, Department of Obstetrics and Gynaecology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India.
2Associate Professor, Department of Obstetrics and Gynaecology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India.
3Associate Professor, Department of Obstetrics and Gynaecology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India.
4Professor, Department of Obstetrics and Gynaecology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India.
5Assistant Professor, Department of Obstetrics and Gynaecology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Kumar K S, Associate Professor, Department of Obstetrics and Gynaecology, SDMCMSH, Sattur, Dharwad, Karnataka-580009, India.
Phone: +919449980334,
E-mail: drsuneelks@yahoo.com
Foetal lymphangiomas are found to frequently occur at the nuchal region. We are reporting a case of a foetal lypmhangioma which involved the abdominal wall and right lower extremity, which was diagnosed by prenatal ultrasonography at 27 weeks of gestation. Prenatal ultrasound, along with Doppler, provided reliable information regarding the extent of the lesion. Magnetic resonance imaging is required only in doubtful cases.
Lymphangioma, Prenatal diagnosis, Ultrasonography
Case Report
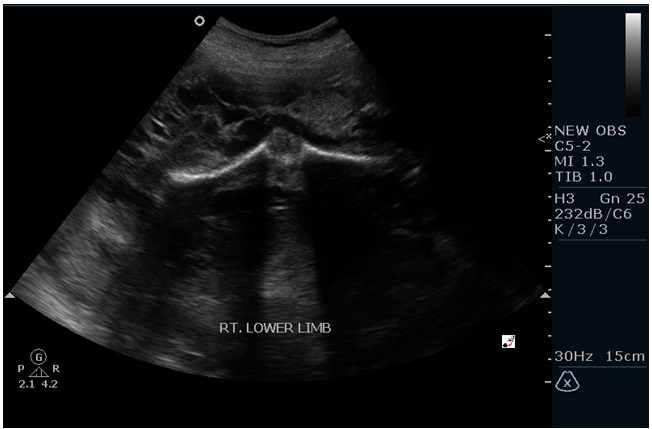
A 22-year-old primigravida came for a routine antenatal check up at 27 weeks of gestation. There was no history of a consanguineous marriage. There was no family history of any hereditary disease or delivery of a malformed foetus in the family. On examination, the fundal height corresponded to that seen at 30 weeks of gestation. Her obstetrics ultrasonography revealed the presence of a single live foetus with large, multicystic, multiseptate, variable sized anechoic areas in an echogenic background, which were found to involve one entire lower limb, which extended upto the ipsilateral pelvic region and were partly seen on the abdomen, on the ipsilateral side [Table/Fig-1,2]. Colour Doppler showed no blood flow within the lesion. The other extremity appeared to be normal. No other structural anomalies were noted. Liquor was excessive. Parameters corresponded to those seen at 27 weeks of gestation. Patient went in to preterm labour at 30 weeks of gestation and delivered a baby with ambiguous genitalia. Baby showed massive oedema with congestion of right side of abdominal wall, back and whole of right lower limb, with involvement upto the toes. No other gross external malformations were noted. On autopsy, multiple sections taken from skin, which were studied, showed a cavernous lymphangioma which involved the right side of abdomen, back and right lower limb. Abdominal organs and the bones of the affected limb were normal. The foetal karyotype showed 46 XX chromosomes.
Ultrasound picture showing cross section of the foetal abdomen with lymhangioma of the abdominal wall

Ultrasound picture showing the entire length of the right lower limb of the foetus affected with lymhangioma
Discussion
Lymphangiomas are benign tumours of the lymphatic vessels, which consist of multiple dilated cysts of varying sizes, which are lined by endothelial cells. They arise from a developmental defect which occurs in the lymphatic pathways. Lymhangiomas occur in almost any area of the body where lymphatics are present. Nearly 75% of the lymphangiomas are located in the head and neck region, which are called as cystic hygromas, which are frequently associated with chromosomal abnormalities. Other areas which are affected are axilla (20%), retroperitoneum and abdominal viscera (2%), limbs and bones (2%) and cervicomediastinum (1%) [1].
Lymphangiomas are classified histologically into three types; simple lymphangiomas which consist of lymphatic capillaries, cavernous lymphangiomas which have larger lymphatic vessels with a fibrous adventitia (index case) and cystic lymphangiomas /cystic hygromas which comprise of multiple cysts. Mixed lesions are likely to coexist in different areas of the same lymphangioma. The cysts usually contain serous or chylous fluid and if they are complicated, they may have bloody or purulent contents [2]. To the best of our knowledge, only few cases of foetal lymphangiomas have been reported so far, with extensions to extremities, which had been diagnosed prenataly by ultrasonography. In our case, ultrasound accurately identified the lesion and defined the extent of the lymphangioma. Doppler studies would help in differentiating them from haemangiomas, because of the absence of blood flow. Extension to extremities can be confirmed by Magnetic resonance imaging (MRI), as was reported by Sung Eun et al., [3]. MRI has added advantage of making an accurate diagnosis of the extent and character of the lesions and also of ruling out abdominal neoplasia with metastatic spread to the limbs. Recently, a three dimensional (3D) ultrasound diagnosis of a massive fatal lymphangioma which occurred at the lower extremity was reported, which showed several advantages of 3-D ultrasound [4]. Pregnancies were terminated in most of the cases which were reported, in view of the poor prognosis of the disease. In some cases, lymphangiomas which were confined to abdominal cavity or wall were treated postnatally by either surgical resection or sclerotherapy [5]. The overall prognosis of foetal lymphangiomas which are diagnosed in the antenatal period is poor, with a mortality rate of 50-100%. Lymphangiomas affecting the head and neck (cystic hygroma) region are frequently associated with karyotypic abnormalities (50-80%), and their prenatal diagnoses are important for their further evaluations and management [6]. The association of chromosomal abnormalities with lymphangiomas affecting the other areas has not been established, but making the karyotype of the foetus is recommended, to counsel patients regarding the prognosis [5].
Although spontaneous regression of foetal lymphangiomas can occur, with normal chromosomes, extensive lymphangiomas require a team approach in the post natal period. Sclerotherapy has been tried for surgically unresectable lymphangiomas by using intralesional Bleomycin, OK 432 or a percutaneous injection of ethibloc, with successful outcomes [3,7]. Recurrences are known to occur in one-third of cases, regardless of the site of lesion and type of the adjunctive therapy which is given.
Conclusion
Foetal lymphangiomas are benign tumours of the lymphatic vessels, which occur frequently in the neck region as cystic hygromas. Lymphangiomas affecting the extremities are rare. Ultrasound with Doppler studies, is a reliable means of diagnosing lymphangiomas. MRI helps in confirming the diagnosis and in knowing the accurate extent of lesion in doubtful cases. Foetal karyotyping should be done for lymphangiomas which are seen in the nuchal region (cystic hygromas), as they are known to have frequent associations with aneuploidy, but it is uncertain as to whether lymphangiomas affecting other areas carry a significant risk of aneuploidy.
[1]. MA Kosir, RE Sonnino, MW Gaurderer, Pediatric abdominal lymphangiomas: a plea for early recognition.J Pediatr Surg 1991 2:1309-13. [Google Scholar]
[2]. P Kaminopetros, E Jauniaux, P Kane, Weston KH Nicolaides, DJ Campbell, Prenatal diagnosis of an extensive fetal lymphangioma using ultrasonography, magnetic imaging and cytologyBr J Radiol 1997 70:750-3. [Google Scholar]
[3]. ER Sung, Prenatal sonographic and MR imaging findings of extensive fetal lymphangioma: A case reportKorean J Radiol 2003 4:260-3. [Google Scholar]
[4]. Schild R L, Orhan Y, Meyberg H, Three-dimensional ultrasound of a massive fetal lymphangioma involving the lower extremityUltrasound Obstet Gynecol 2003 22:547-51. [Google Scholar]
[5]. P Deshpande, P Twining, D O’Neill, Prenatal diagnosis of fetal lymphangioma using ultrasonographyUltrasound Obstet Gynecol 2001 17:445-8. [Google Scholar]
[6]. M HO, CC Lee, TY Lin, Prenatal diagnosis of abdominal lymphangiomaUltrasound Obstet Gynecol 2002 20:203-8. [Google Scholar]
[7]. J Dubois, L Garel, Abela L Laberge, S Yazbeck, Lymphangiomas in children: Percutaneous sclerotherapy with an alcoholic solution of ZeinRadiology. 1997 204:651-4. [Google Scholar]