Classification & Prevalence of Dental Surface Defects in Areas of Gingival Recession- A Clinical Study
Prashant Bhusari1, Nitin Agrawal2, Shivam Upadhyay3, Shiras Verma4, Amiyavardhan Jain5, Shraddha Jaroli6
1 Professor, Department of Periodontics, Modern Dental College & Research Centre, Indore, India.
2 Post Graduate Student, Department of Periodontics, Modern Dental College & Research Centre, Indore, India.
3 Post Graduate Student, Department of Periodontics, Modern Dental College & Research Centre, Indore, India.
4 Senior Lecturer, Department of Periodontics, Institute of Dental Education and Advance Studies. Gwalior (M.P.), India.
5 Post Graduate Student, Department of Periodontics, Modern Dental College & Research Centre, Indore, India.
6 Post Graduate Student, Department of Conservative & Endodontics, Modern Dental College & Research Centre, Indore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nitin Agrawal, Modern Dental College & Research Centre, Gandhinagar, Indore-453112, MP, India.
Phone: +919770907205,
E-mail: drnitin143agrawal@gmail.com
Background: Apical migration of the gingival margin beyond the cement-enamel junction (CEJ) is called as gingival recession. Various classifications of gingival recession have been proposed to evaluate different degrees of damage to periodontal tissues, but do not consider the condition of the exposed root surface: presence of an identifiable CEJ and presence of root abrasion. Sometimes these lesions may be associated with enamel abrasion. Therefore, the aim of this paper is to propose the new classification of dental surface defects in gingival recession area.
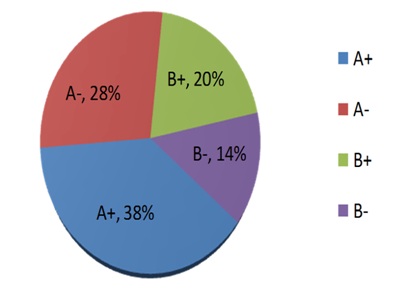
Methods: Two factors were evaluated to set up a classification system: presence (A) or absence (B) of CEJ and presence (+) or absence (-) of dental surface discrepancy caused by abrasion (step). Four classes (A+, A-, B+, and B-) were identified on the basis of these variables. The classification was used on 1,000 gingival recessions to examine the distribution of the four classes.
Results: Out of 1,000 exposed root surfaces, 380 showed an identifiable CEJ associated with step (Class A+, 38%); 280 an identifiable CEJ without any associated step (Class A-, 28%); 200 an unidentifiable CEJ with a step (Class B+, 20%); and 140 an unidentifiable CEJ without any associated step (Class B-, 14%).
Conclusion: The proposed classification describes the dental surface defects that are of paramount importance in diagnosing gingival recession areas which might help in selecting the definite treatment approach.
Cemento-enamel junction, Cervical abrasions, Coronally advanced flap, Diagnosis, Periodontal probe
Introduction
Over the last few years dentistry has evolved in such a way that clinicians are not only required to treat disease and improve function but also to cope with the ever increasing aesthetic demands of our patients. Among the aesthetic procedures, root coverage by periodontal plastic surgery has attracted the most interest. Indications for exposed root coverage are aesthetic and/or cosmetic demands, as well as the management of root hypersensitivity, shallow root caries lesions, and cervical abrasions.
To categorise gingival recession, Miller proposed four classes of marginal gingival recessions based on the degree of involvement of the periodontal tissues (Mucogingival junction and underlying alveolar bone). This clinically useful classification evaluates different degrees of damage to periodontal tissues, but does not consider the condition of the exposed root surface: presence of an identifiable cemento-enamel junction (CEJ) and presence of root abrasion. Sometimes these lesions may be associated with enamel abrasion.
The CEJ serves as the reference point for the diagnosis and treatment of such defects. The anatomic and aesthetic success of a procedure is based on a gingival margin located slightly more coronally to CEJ after surgery [1] and in a good integration of the grafted gingival tissue with the adjacent teeth [2]. However, the CEJ is not identifiable in some cases because of dental abrasion caused by tooth brushing trauma or cervical caries [3,4]. In this situation, clinicians encounter difficulties in accurately measuring the depth and the width of recessions during the diagnostic phase. Other problems may arise during the surgical procedure because the lack of an identifiable CEJ does not allow for the precise location of the gingival margin when suturing. Where does the clinician place the margin of the flap or graft? In fact, after surgery the coronal position of the gingival margin with respect to the CEJ is a fundamental requirement for obtaining complete root coverage using coronally advanced flap [4,5].
In addition, the accurate evaluation of the clinical outcome of the root coverage procedure is difficult at the end of the treatment if the CEJ is lacking. In this situation, it is not possible to establish whether or not complete root coverage has been achieved. In many articles dealing with root coverage procedures, gingival recessions with no identifiable CEJ are excluded from the study as selection criteria [5,6]. Therefore, an accurate evaluation of the dental hard tissues associated with Miller’s periodontal classification could be useful for a complete diagnosis of gingival recession areas. Pini-Prato GP et al., [7] had described the classification of dental surface defects which were of paramount importance in diagnosing gingival recession areas.
The aim of this article is therefore to evaluate the prevalence of dental surface defects in gingival recession areas by examining two factors: presence or absence of CEJ, and presence or absence of dental surface discrepancy (step).
Materials and Methods
To observe the distribution of the four classes of the present classification, 100 patients (64 males and 36 females) presenting at least one gingival recession were examined between August 2012 and January 2013 in the Department of Periodontology, Modern Dental College & Research Centre Indore, India. A sample of 1,000 consecutive maxillary and Mandibular gingival recessions was included in the study. Informed written consent was obtained from all subjects who participated in the study.
The evaluation was performed on both frontal and lateral views using an x4 magnification lens, a periodontal probe (PCP UNC 15), and a dental explorer. Two variables were considered: CEJ and cervical discrepancies. Considering the presence of the CEJ on the buccal surface, two classes were identified: Class A, identifiable CEJ on the entire buccal surface; and Class B, unidentifiable CEJ totally or partially. Considering the presence of cervical discrepancies (step), measured with a periodontal probe perpendicular to the long axis of the tooth in the deepest point of the abrasion, two classes were identified: Class (+), presence of cervical step (>0.5 mm) involving the root or the crown and the root; and Class (-), absence of cervical step. Therefore, a working classification identifies four different conditions [Table/Fig-1,2,3,4and5].
Identifiable CEJ without any associated step (Class A-)

Identifiable CEJ associated with a root surface defect (Class A+)

Unidentifiable CEJ without any associated step (Class B-)

Unidentifiable CEJ with a step (Class B+)

Classification system of four different classes of root surface discrepancies
Results
The distribution of the four classes was observed within a population of 1,000 teeth in 100 patients, between 20 and 75 years of age. A total of 554 recessions were located in the maxillary arch and 446 in the lower jaw. A descriptive analysis is given in [Table/Fig-6]. Out of 1,000 exposed root surfaces associated with gingival recession, 380 showed an identifiable CEJ associated with a root surface defect (Class A+, 38%); 280 an identifiable CEJ without any associated step (Class A-, 28%); 200 an unidentifiable CEJ with a step (Class B+, 20%); and 140 (Class B-, 14%) an unidentifiable CEJ without any associated step [Table/Fig-7].
Distribution of the four classes with in a population of 1,000 gingival recessions
| Maxillary teeth | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
|---|
| Class A+ | 08 | 10 | 14 | 31 | 25 | 18 | 05 | 08 | 10 | 13 | 20 | 21 | 20 | 02 |
| Class A- | 09 | 11 | 10 | 12 | 13 | 07 | 02 | 10 | 13 | 14 | 19 | 18 | 10 | 05 |
| Class B+ | 02 | 03 | 05 | 12 | 15 | 18 | 03 | 02 | 07 | 08 | 20 | 11 | 19 | 01 |
| Class B- | 01 | 04 | 05 | 05 | 09 | 08 | 04 | 05 | 05 | 08 | 05 | 06 | 04 | 01 |
| Mandibular teeth | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 41 | 42 | 43 | 44 | 45 | 46 | 47 |
|---|
| Class A+ | 03 | 05 | 05 | 15 | 15 | 25 | 03 | 02 | 02 | 10 | 30 | 25 | 30 | 05 |
| Class A- | 04 | 05 | 08 | 15 | 10 | 11 | 03 | 08 | 01 | 10 | 15 | 15 | 13 | 09 |
| Class B+ | 08 | 01 | 03 | 15 | 10 | 05 | - | 01 | 02 | 05 | 10 | 09 | 05 | - |
| Class B- | 01 | 01 | 03 | 04 | - | 07 | 06 | 06 | 03 | 05 | 14 | 10 | 05 | 04 |
Distribution of dental surface defects
Discussion
The goals of periodontal plastic surgery are to re-establish aesthetic by obtaining complete root coverage, function of dento-gingival complex and to treat root sensitivity.
During daily practice routine, recording an identifiable CEJ or the presence of a tooth discrepancy is of a paramount importance for measuring recession depth and evaluating the outcome after treatment (i.e., partial or complete root coverage). Therefore, a complete diagnosis of a defect requires not only the evaluation of the periodontal tissue, but also the assessment of the hard dental tissue conditions.
In this study surface discrepancy (step) was measured with the help of ×4 magnifying lens and periodontal probe (PCP UNC 15) perpendicular to the long axis of the tooth in the deepest point of the abrasion. The choice of a step >0.5 mm is justified by a clinical observation that flap thickness >0.8 mm is associated with complete root coverage as the thick flap may fill the cervical discrepancy at the end of its coronal position [4].
Following the validation of the system, a sample of 1,000 teeth with gingival recessions was examined to assess the distribution of the four classes of this classification. It should be noted that 28% of gingival recessions showed an identifiable CEJ without surface discrepancy (Class A -), thus allowing for a precise diagnosis and for precise outcome assessment of the root coverage procedure after treatment. There was 14% of the recessions without identifiable CEJ and any associated step (Class B -) thus making the recession more difficult for diagnosis and not allowing for precise outcome assessment of the root coverage procedure after treatment. In 38% of gingival recessions CEJ was identifiable with surface discrepancy (Class A +) but 20% of cases were worst as they made the diagnosis and assessment of prognosis after treatment extremely difficult due to un-identifiable CEJ associated with surface discrepancy(step). These different conditions should be taken into consideration and might require different treatment approaches.
According to our knowledge, there is only one study by Pini-Prato et al., [7] who proposed the classification of dental surface defects in gingival recession areas. They found highest prevalence of an identifiable CEJ without any associated step (Class A-, 46%) in their study. Our results are not in accordance with their results as we found highest prevalence of an identifiable CEJ associated with a root surface defect (Class A+, 38%). The difference in the results might be due to racial & genetic factors (thickness of enamel and cementum). Although there was no age group and sex difference in participants, other confounding factors that influence the occurrence of various dental surface defects such as habits, brushing techniques, type of brush used, frequency of brushing need to be investigated further.
The literature, however, contains little information on periodontal treatment of gingival recessions associated with cervical dental lesions. The abrasions can involve the root, with deep steps at the CEJ, or both the root cementum and the enamel. In this latter situation there often marked steps at the CEJ level. This is often associated with dental hypersensitivity which, along with cosmetic problems, is an individual for mucogingival surgery for root coverage. In these cases, in order to adapt the coronally advanced flap to the tooth surface or to the underlying connective tissue graft (when using the bilaminar approach), and to cover the CEJ, practitioners tend to grind and eliminate the abrasion. This, however, further diminishes the dental tissue, and if root coverage is incomplete leads to the onset/increase of dental hypersensitivity. The choice of the technique is based on the assessment of the abrasion depth (CEJ step) [7].
For steps with a depth of <1mm, the technique was to apply a connective tissue graft over the abrasion, extending laterally and apically over the recipient site, associated with a pedicle flap positioned as coronally as possible. Recent studies have shown that the further the flap is coronally advanced, the greater the root coverage [8].
For step with a depth of ≥1mm, the procedure consisted of two connective tissue grafts covered by a coronally advanced flap. The first (primary) graft served to fill the abrasion, while the second (secondary graft) placed over the primary, was extended into the adjacent receiving site. This strategy makes it possible to adapt the secondary graft perfectly to the tooth surface, avoiding dead tracts under the secondary graft, and above all does away with the need to remove dental tissue to eliminate the existing abrasion [3]. Both techniques proved effective in the treatment of gingival recessions associated with dental abrasions. If defects are treated by CAF only it may complicate the proper adaptation of the flap on the tooth, leading to soft tissue collapse and poor stabilization of the graft over the exposed root. In this case, even if complete root coverage occurs, the final esthetic result may be poor because the profile of the gingival margin tends to be flat, parallel to the abrasion edge [3].
Finally, the loss of an identifiable CEJ makes the interview with the patient regarding the choice of treatment and its prognosis difficult. The patient might expect that the entire dental lesion (root and crown abrasion) will be covered completely by gingival tissue after the procedure. Since the original gingival margin covered the CEJ, the margin level after the procedure cannot be located coronally on the lost enamel but apically at the level of the previous CEJ; the periodontist has to explain to the patient the expected location of the gingival margin after treatment [9].
Restoration of a missing CEJ before the root coverage procedure has been suggested. Various dental materials and surgical approaches have been used to manage gingival recessions associated with tooth abrasion in the area of the CEJ [10,11]. Resin ionomer materials have many properties that allow them to be used successfully in the sub gingival region [12]. Dragoo [13] demonstrated histological evidence that both epithelium and connective tissue can adhere to the resin ionomer when placed in a sub gingival environment. A new class of fluoride releasing resin materials with pre-reacted glass (PRG), called Giomer, has been introduced for cervical restorations with claims of good color matching, biocompatibility and fluoride release and fluoride release and fluoride recharge potential [14]. The combined restorative and periodontal approach allowed for careful finishing of the restoration margin after flap elevation using a magnification system. This may have facilitated proper soft tissue healing over the apical aspect to the restoration margin [15,16]. These findings corroborate the observation that minimal inflammation is observed following root coverage and CEJ reconstruction when a proper finishing of the dental material is accomplished [17,18].
Conclusion
The described classification of dental surface defects in conjunction with the classification of periodontal tissue is useful for reaching a more precise diagnosis in areas of gingival recession and is useful for selecting the appropriate treatment approach without having to eliminate additional dental hard tissue. Complete root coverage might not be obtained even in Miller’s Recession defects associated with root and crown abrasion. Therefore, an accurate evaluation of the dental hard tissue associated with Miller’s periodontal classification could be useful for complete diagnosis of gingival recession areas.
[1]. Zucchelli G, Testori T, De Santis M, Clinical and anatomical factors limiting treatment outcomes of gingival recession: A new method to predetermine the line of root coverageJ Periodontal 2006 77(4):714-21. [Google Scholar]
[2]. Cairo F, Rotundo R, Miller PD, Pini-Prato GP, Root coverage esthetic score score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical casesJ Periodontol. 2009 80:705-10. [Google Scholar]
[3]. Pini-Prato G, Baldi C, Rotundo R, Franceschi D, Muzzi L, The treatment of gingival recession associated with deep corono-radicular abrasions (CEJ step)- A case seriesPerio- Periodontal Practices Today 2004 1:57-66. [Google Scholar]
[4]. Pini-Prato G, Baldi C, Pagliaro U, Coronally advanced flap procedure for root coverage. Treatment of root surface: Root planning versus polishingJ Periodontal. 1999 70:1077-84. [Google Scholar]
[5]. Pini-Prato GP, Baldi C, Nieri M, Coronally advanced flap: The post-surgical position of the gingival margin is an important factor for achieving complete root coverageJ Periodontol 2005 76:713-22. [Google Scholar]
[6]. Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M, Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: A comparative controlled randomized clinical trialJ Periodontol 2009 80(7):1083-94. [Google Scholar]
[7]. Pini-Prato GP, Franceschi D, Cairp F, Classification of Dental Surface Defects in Areas of Gingival RecessionJ Periodontol. 2010 81:885-90. [Google Scholar]
[8]. Baldi C, Pini-Prato GP, Pagliaro U, Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage? A 19-case seriesJ Periodontol. 1999 70:1077-84. [Google Scholar]
[9]. Cairo F, Pini-Prato GP, A technique to identify and Reconstruct the Cemento-enamel Junction level Using Combined Periodontal and Restorative Treatment of Gingival Recession. A Prospective Clinical StudyInt J Periodontics Restorative Dent 2010 30:573-81. [Google Scholar]
[10]. Terry DA, McGuire MK, McLaren E, Fulton R, Swift EJ Jr, Perioesthetic approach to the diagnosis and treatment of carious and noncarious cervical lesions: Part IIJ Esthet Restor Dent. 2003 15:284-96. [Google Scholar]
[11]. Lucchesi JA, Santos VR, Amaral CM, Peruzzo DC, Duarte PM, Coronally positioned flap for treatment of restored root surfaces: A 6-month clinical evaluationJ Periodontol. 2007 78:615-23. [Google Scholar]
[12]. Alkan A, Keskiner I, Yuzbasioglu E, Connective tissue grafting on resin ionomer in localized gingival recessionJ Periodontol. 2006 77(8):1446-51. [Google Scholar]
[13]. Dragoo MR, Resin-ionomer and hybrid-ionomer cements: part II, human clinical and histologic wound healing responses in specific periodontal lesionsInt J Periodontics. Restorative Dent. 2007 17(1):75-87. [Google Scholar]
[14]. Matis BA, Cochran MJ, Carlson TJ, Guba C, Eckert GJ, A three- year clinical evaluation of two dentin bonding agentsJ Am Dent Assoc. 2004 135(4):451-57. [Google Scholar]
[15]. Santamaria MP, Suaid FF, Nociti FH Jr, Casati MZ, Sallum AW, Sallum EA, Periodontal surgery and glass ionomer restoration in the treatment of gingival recession associated with a non-carious cervical lesion: Report of three casesJ Periodontol. 2007 78:1146-53. [Google Scholar]
[16]. Santamaria MP, Suaid FF, Casati MZ, Nociti FH, Sallum AW, Sallum EA, Coronally positioned flap plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with noncarious cervical lesions: A randomized controlled clinical trialJ Periodontol 2008 79:621-28. [Google Scholar]
[17]. Santamaria MP, da Silva Feitosa D, Nociti FH Jr, Casati MZ, Sallum AW, Sallum EA, Cervical restoration and the amount of soft tissue coverage achieved by coronally advanced flap: A 2-year follow-up randomized-controlled clinical trialJ Clin Periodontol 2009 36:434-41. [Google Scholar]
[18]. Santamaria MP, Ambrosano GM, Casati MZ, Nociti Júnior FH, Sallum AW, Sallum EA, Connective tissue graft plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with non-carious cervical lesion: A randomized controlled clinical trialJ Clin Periodontol 2009 36(9):791-98. [Google Scholar]