Risk Factors Assessment of the Difficult Intubation using Intubation Difficulty Scale (IDS)
Vaibhav K. Nasa1, Shaila S. Kamath2
1Postgraduate, Department of Anaesthesiology, Kasturba Medical College, Mangalore, Manipal University, Manipal, India.
2Associate Professor, Department of Anaesthesiology, Kasturba Medical College, Mangalore, Manipal University, Manipal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shaila S. Kamath, “Krithika” 5-7-710/2, Near Sathyasai Nursing Home, Dongerkery, Mangalore-575003, Karnataka, India.
Phone: 9844090231,
E-mail: shailakamath@ymail.com
Background: The major responsibility of anaesthesiologist is to maintain adequate gas exchange in his patients in all circumstances and this require that patency of upper airway is constantly maintained. Problems with upper airway management are among the most frequent causes of anaesthetic mishaps. Using intubation difficulty scale (IDS) we made an attempt to objectively assess the predictors of difficult intubation. We assessed classical bedside tests such as modified Mallampati test, Thyromental distance test and also neck extension test.
Methods: We prospectively observed 400 patients undergoing general anaesthesia with endotracheal intubation, for each patient intubation difficulty score was recorded during intubation. Risk factors assessment of difficult intubation done using IDS. Risk factor assessed includes modified mallampati class III and IV, thyromental distance ≤ 6cm and neck extension < 5cm. Patients were categorised as Easy intubation (IDS, 0 to 2), slightly difficult intubation (IDS, 3 to 4) and difficult intubation (IDS 5). Preoperative airway assessment was done by thyromental distance measurement, neck extension measurement and modified mallampati test. Data was analysed using Receiver operating characteristic curve (ROC) and area under curve (AUC) for each test computed. p<0.05 was considered significant.
Results: The incidence of difficult intubation was 8% and there were no failure to intubate the trachea. The AUC were as follows: modified Mallampati test 0.473 (p<0.005), Thyromental distance test 0.753 (p<0.005) and neck extension test 0.768 (p<0.005).
Conclusion: The results indicate that neck extension test is strongest predictor of difficult intubation (IDS≥5) in comparison to Thyromental test and modified mallampati test.
Airway, Difficult intubation, Mallampati
Introduction
The major responsibility of anaesthesiologist is to maintain adequate gas exchange in his patients in all circumstances and this require that patency of upper airway is constantly maintained. Problems with upper airway management are among the most frequent causes of anaesthetic mishaps. In the past numerous studies have been done to predict the difficult intubation. In one meta analysis [1] of 35 studies it was found that each preoperative airway assessment test that included modified mallampati test, thyromental distance measurement, sternomental distance, yielded poor to moderate sensitivity (20-62%), and moderate to fair specificity (82- 97%). Interestingly, in 80% of these studies diagnostic criteria for difficult intubation used was Cormach and Lehane grade III or IV. Other studies [2,3] too indicated that poor laryngeal view is not synonymous with difficult intubation. Objective of our study was to find out the incidence of difficult intubation and to compare the three available methods of predicting intubation difficulty scale (IDS) [4] i.e. modified Mallampati classification, thyromental distance test and neck extension test.
Materials and Methods
After obtaining institutional ethics committee approval, patients were given information about the procedure and written informed consent was taken. Four hundred patients above the age of 12 years and above who were fit for general endotracheal anaesthesia irrespective of their ASA physical status were included in the study.
Patients below the age of 12 years, patients with obvious airway malformations, patient with inter incisor distance < 3cm, patient allergic to drugs used in study were excluded from the study. Each patient underwent a preoperative general physical examination and a detailed systemic examination. Plastic measuring tape was used for measuring thyromental distance and neck extension.
Modified Mallampati test was carried out based on the method described by Mallampati et al., [5] In class I- the soft palate, fauces, uvula and pillars seen, in class II- soft palate, fauces and uvula seen, in class III-soft palate and base of uvula seen and in class IV- soft palate not visible [6] Patil’s test was done for the measurement of thyromental distance. It was defined as the straight distance from the inside of mentum to the thyroid prominence while the patient’s neck is fully extended. Patient’s were categorised into two groups based on thyromental distance < 6 cm or > 6 cm [7]. Range of head and neck extension was measured as described by Chow et al., [8]. It is nothing but modified measurement of sternomental distance which advocates measuring the straight distance from sternal notch to the inside of mentum with patient’s head both in neutral and maximally extended position. Patients were categorized into two groups based on neck extension < 5 cm or > 5 cm. Standardised anaesthesia protocol was followed. Premedication comprised of oral diazepam 0.2 mg/kg (max.15 mg) administered night before and two hour prior to induction of anaesthesia. After preoxygenation anaesthesia was induced with iv propofol 2 mg/kg, and iv fentanyl 2 μg/kg. Once mask ventilation was ensured, iv vecuronium 0.1 mg/kg was administered to facilitate endotracheal intubation, laryngoscopy was performed with patient’s head resting in the sniffing position on a pillow measuring 10cm in height, using Macintosh blade, size 3. The anaesthesiologist performing the laryngoscopy had working experience of at least two years in operating room. Laryngoscopic grading of best view possible without optimal external laryngeal manipulation was made according to Cormack and Lehane’s classification. IDS was recorded for each patient according to Adnet et al., [4]. Backup plan for the management of difficult airway, along with the difficult airway cart was readily available in all the cases. Data was analysed using Receiver operating characteristic curve (ROC) and area under curve (AUC) for each test was computed. p<0.05 was considered significant.
Results
Incidence of difficult intubation in our study was 8% (32 out of 400 patients). The study done on 400 patients included 210 male (52.5%) and 190 female (47.5%) patients. Study covers the wide age group from 12 yrs and above. Nearly 63% of study population was in 21-50 yrs age group.
Prediction of difficult intubation by modified mallampati test and actual intubation difficulty score (IDS) were compared. Among 368 patients (92%) who were mallampati grade1 and grade 2, 306 patients (83%) had IDS score of 0-2, 40 patients (11%) had IDS score of 3-4 and 22 patients (6%) had IDS score >5. Among 32 patients (8%) with mallampati grade 3 and grade 4, 10 patients (31.25%) had IDS score of 0-2, 12 patients (37.5%) had IDS score of 3-4 and only 10 patients (31.25%) had IDS score >5 [Table/Fig-1] .
The sensitivity of the modified Mallampati test was 31.25% and specificity was 96%. The test has a positive predictive value of 31% and an overall accuracy of 79% [Table/Fig-2] .
Comparison of thyromental distance test with IDS we found that out of 356 patients (89%) who had thyromental distance >6, 312 patients (88%) had IDS score of 0-2, 37 patients (10%) had IDS score of 3-4 and only 7 patients (2%) had IDS score >5. Similarly, out of 44 patients (11%) who had thyromental distance <6, 4 patients (9%) had IDS score of 0-2, 15 patients (34.5%) had IDS score of 3-4 and 25 patients (56.5%) had IDS score >5 [Table/Fig-3] . The sensitivity of thyromental distance was 78% and specificity of 98%. The test has a positive predictive value of 56% and overall accuracy of 84% [Table/Fig-2] .
Comparison of neck extension test with actual intubation difficulty score (IDS) revealed that out of 383 patients (95.75%) with neck extension >5 cm, 315 patients (82%) had IDS score of 0-2, 49 patients (13%) had IDS of 3-4 and 19 patients (5%) had IDS score of >5. Among 17 patients (4.25%) with neck extension <5cm, 1 patient (6%) had IDS score of 0-2, 3 patient (17.6%) had IDS score of 3-4 and 13 patients (76.4%) had IDS score of >5 [Table/Fig-4] . The sensitivity of neck extension test was 40% and specificity of 99%. The test has positive predictive value of 76% and overall accuracy of 82% [Table/Fig-2] .
So, we observe that among the three tests used thyromental distance test has the highest sensitivity (78%) and highest overall accuracy of 84%. The neck extension test has the highest specificity (99%) and highest positive predictive value of 76%. But its overall accuracy is slightly less than thyromental test (82% vs. 84%). Modified Mallampati test is least sensitive with a sensitivity of 31% and weakest predictive of difficult intubation (PPV 31%) among these three tests.
Comparison of modified mallampati grading vs. IDS Score
| MP Grade | IDS Score | Total |
| 0-2 | 3-4 | ≥5 |
| 1 and 2 | 306 (83%) | 40 (11%) | 22 (6%) | 368 |
| 3 and 4 | 10 (31.25%) | 12 (37.5%) | 10 (31.25%) | 32 |
| Total | 316 | 52 | 32 | 400 |
Comparison of three airway indices used
| | Modified Mallampati test | Thyromental test | Neck extension test |
| Sensitivity | 31% | 78% | 40% |
| Specificity | 96% | 98% | 99% |
| Positive predictive value | 31% | 56% | 76% |
| Accuracy | 79% | 84% | 82% |
Comparison of TMD vs. IDS Score
| TMD (cm) | IDS Score | Total |
| 0-2 | 3-4 | ≥5 |
| ≤6 | 04 (9%) | 15 (34.5%) | 25 (56.5%) | 44 |
| >6 | 312 (88%) | 37 (10%) | 07 (2%) | 356 |
| Total | 316 | 52 | 32 | 400 |
Comparison of neck extension test vs IDS score
| Neck Extension (cm) | IDS Score | Total |
| 0-2 | 3-4 | ≥5 |
| ≥5 | 315 (82%) | 49 (13%) | 19 (5%) | 383 |
| <5 | 1 (6%) | 03 (17.6%) | 13 (76.4%) | 17 |
| Total | 316 | 52 | 32 | 400 |
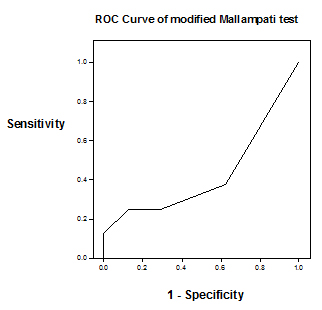
Area under receiver operating characteristic (ROC) curve for modified Mallampati test is 0.473
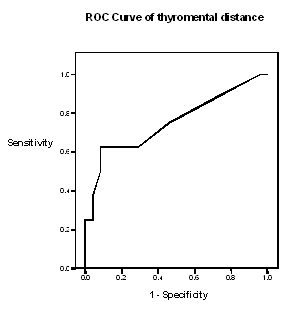
Area under receiver operating characteristic (ROC) curve for thyromental distance test is 0.753
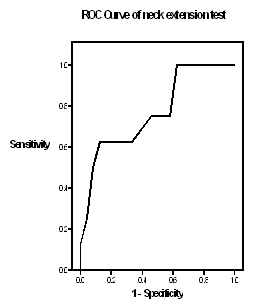
Area under receiver operating characteristic (ROC) curve for neck extension test is 0.768
Discussion
In our study, the rate of difficult intubation (IDS>5) was 8% and there were no failure to intubate the trachea. One of the important highlight of our study is the detection of incidence of minor intubation difficulties (13%) during routine surgeries.
Modified mallampati test which is reported to have sensitivity and specificity 65%- 81% and 66%- 82% respectively with positive predictive value between 8% -9% [9] fails to reach such high sensitivity in our study (31%). The reasons for it may be poor interobserver reliability [10] and / or different criteria set for difficult intubation in our study. But our results are in good agreement with the findings of Cattano et al., [11]. They concluded that mallampati by itself is insufficient for predicting difficult intubation. The higher positive predictive value (31%) for mallampati test in our study could be because of high prevalence of difficult intubation (8%). But it is significantly less in comparison to positive predictive value observed for thyromental test (56%) and neck extension test (76%). Our data demonstrated moderate sensitivity (78%) and good specificity (98%) and positive predictive value (56%) for thyromental test which is in contrary to the findings of Tse et al., [12]. Reasons could be different cut off values and definition of difficult intubation used in both studies. But our findings support the results of Gonzalez et al., [13]. The reasons could be the similar definition of difficult intubation (IDS≥5) and cut off level of 6cm in both studies. The bedside test used to evaluate neck extension was new and our results demonstrate that it is the strongest predictor of difficult tracheal intubation (IDS≥5) with a positive predictive value of 76%. This was in contrary to the findings of Tse et al.,[12], where they concluded that cervical mobility was of little value in predicting difficult airway. The discrepancies in two studies could be because of different methods of assessing neck extension and different criteria of difficult intubation used. But our results further confirmed the findings of Hu et al., [14].
Moreover, ROC Curv analysis revealed that area under ROC curve (AUC) for modified mallampati test was 0.473 [Table/Fig-5] , which is significantly less than AUC for thyromental test was 0.753 [Table/Fig-6] , and neck extension test 0.768 [Table/Fig-7] .
Conclusion
We conclude that neck extension < 5 cms is the strongest predictor of difficult intubation with a positive predictive of 76% and area under ROC curve of 0.768. Also, thyromental distance of < 6cms has better positive predictive value than modified Mallampati test (56 % Vs 31%) in predicting difficult tracheal intubation. This is supported by area under ROC curve (0.753 Vs 0.473).
Finally it may be emphasized that this study is an attempt to assess the risk factors for difficult tracheal intubation in a more objective and reliable way to make this whole exercise worthwhile.
Acknowledgement
We would like to acknowledge the support and help of Kasturba Medical College, Mangalore, Manipal University, Manipal, Karnataka, India in performing this study.
[1]. T Shiga, Z Wajma, T Inoue, A Sakamoto, Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance.Anesthesiology. 2005 103:429-37. [Google Scholar]
[2]. P Juvin, E Lavaut, H Dupont, Difficult tracheal intubation is more common in obese than in lean patientsAnesth Analg 2003 97:595-600. [Google Scholar]
[3]. AN O’Leary, M Sandison, D Steele, M Fitzpatrick, KW Roberts, Cormack Grade is a poor index of difficulty experienced during endotracheal intubation.Anesthesiology. 2006 105(A522.) [Google Scholar]
[4]. F Adnet, SW Borron, SX Racine, JL Chemessy, JL Fournier, P Plaisance, The Intubation Difficulty Scale [IDS]: Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation.Anesthesiology. 1997 87:1290-97. [Google Scholar]
[5]. SR Mallampati, SP Gatt, LD Gugino, SP Desai, A clinical study to predict difficult intubation: A prospective study.Can Anaesth Soc J 1985 32:429-34. [Google Scholar]
[6]. GLT Samsoon, JRB Young, Difficult tracheal intubation: A retrospective studyAnaesthesia. 1987 42:487-90. [Google Scholar]
[7]. VU Patil, LC Stehling, HL Zaunder, Predicting the difficulty of intubation utilizing an intubation guide.Anesthesiology. 1983 10(32) [Google Scholar]
[8]. FL Chow, PG Duncan, WE Code, Bedside assessment of neck extensionCan J Anesth 1993 40(A4) [Google Scholar]
[9]. SM Yentis, Predicting difficult intubation – worthwhile exercise or pointless ritualAnaesthesia. 2002 57:105-09. [Google Scholar]
[10]. K Karkouti, DK Rose, LE Ferris, DF Wigglesworth, Meisami-Ford H Lee, Inter observer reliability of the tests used for predicting difficult intubation.Can J Anaesth. 1996 43:554-59. [Google Scholar]
[11]. D Cattano, E Panicucci, A Paolicchi, F Forfori, F Giunta, C Hagberg, Risk factors assessment of the difficult airway: An Italian survey of 1956 patientsAnesth Analg. 2004 99:1774-79. [Google Scholar]
[12]. JC Tse, EB Rimm, A Hussain, Predicting difficult endotracheal intubation in surgical patients scheduled for general anaesthesia: A prospective blind study.Anesthesia and Analgesia 1995 81:254-58. [Google Scholar]
[13]. H Gonzalez, V Minville, K Delanoue, M Mazerolles, D Concina, O Fourcade, The importance of increased neck circumference to intubation difficulties in obese patients.Anesth Analg 2008 106:1132-36. [Google Scholar]
[14]. LQ Hu, RM Boyer, RJ Marcus, P Robles, RJ McCarthy, Importance of ASA task force airway management risk factors in predicting difficult intubationAnesthesiology. 2008 109(A1242.) [Google Scholar]