Primary Necrotising Fasciitis of the Breast: Case Report and Brief Review of Literature
Prabhat Yaji1, Balachandra Bhat2, Harish E3
1Postgraduate Student, Department of General Surgery, Vijayanagar Institute of Medical Sciences, Bellary, Karnataka, India.
2Assistant Professor, Department of Pathology, PES Institute of Medical Sciences and Research, Kuppam, Chittoor District, AP, India.
3Postgraduate Student, Department of General Surgery, Ramaiah, Bellary, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prabhat Yaji, 24/1, 2nd cross, ISEC Main Road, Nagarbhavi, Bangalore-560072, India.
Phone: 9844980053,
E-mail: prabhatyaji@gmail.com
Necrotizing fasciitis is a rapidly spreading progressive infection of the fascia with necrosis of the subcutaneous tissues. Primary necrotising fasciitis of the breast is extremely rare and hence we report the case of a 55-year-old woman presenting to our hospital with primary necrotising fasciitis of the breast in a state of systemic septic shock. She was admitted in surgical intensive care unit and treated with resuscitation, intravenous antibiotics and aggressive debridement. We discuss the details of the case, our treatment approach, the outcome and also briefly review the literature.
Breast gangrene, Necrotising fasciitis, Polymicrobial infection
Case Report
A 55-year-old postmenopausal woman brought to emergency department of our hospital with history of progressive pain and swelling in the left breast since last one week. She also had high grade fever since the onset of pain and swelling. There was no history of any trauma. She is a known diabetic since last 4 yrs and she was diagnosed to be hypertensive 6 months back. She was regularly taking her anti-diabetic and anti-hypertensive medications. She visited a clinic at her local place and was treated on outpatient basis before being referred here as her condition deteriorated.
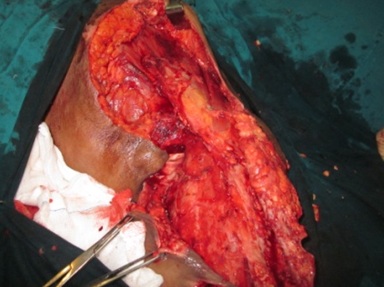
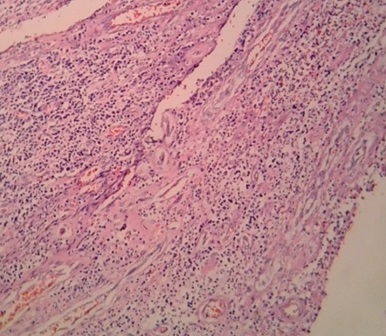
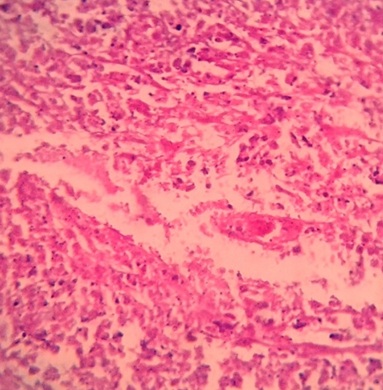
On examination the patient was febrile, drowsy and dehydrated. Pulse- 140/min, BP- 80/46 mm Hg, Respiratory rate- 32/min. Local examination showed foul smelling extensively sloughed out outer part of the breast including nipple areola complex and the infection was also extending into the left arm [Table/Fig-1]. Systemic examination of cardiovascular and respiratory system were normal. Her clinical picture indicated that she was in septic shock secondary to the necrotising fasciitis of the left breast. Investigations revealed Haemoglobin- 9mg/dl, total leucocyte count- 28,000/cu.mm, Urea – 69mg/dl and creatinine – 2.1mg/dl. Chest X-ray was normal. Her serum electrolytes were deranged and liver enzymes elevated. After primary resuscitation with intravenous fluids, broad spectrum antibiotics (piperacillin and tazobactum with metronidazole) and other supportive measures, her BP was 100/60 mm Hg and her urine output was about 300ml in 6hrs indicating adequate correction of dehydration. She was taken up for emergency surgery and adequate debridement comprising almost left mastectomy was done [Table/Fig-2] removing all the necrotic tissues of the breast including the deep fascia of the breast and the deep fascia of proximal part of left upper arm. On the 2nd day of admission the patient continued to be drowsy and her Pulse- 124/min and BP was 100/64 mm Hg. She was maintaining her blood pressure without any inotropic support. Her haematological investigations did not show any marked improvement. Urea, creatinine, electrolytes remained deranged. She continued to receive antibiotics and supportive measures in ICU. The wound culture was reported as polymicrobial growth. A second culture swab taken 48hrs after admission was reported as E.Coli and Pseudomonas which were resistant to many of the commonly used antibiotics. Blood culture showed no organisms. The patient succumbed to the severe sepsis on the third day after admission. Histopathology was reported as exuberant inflammatory granulation tissue [Table/Fig-3] with suppurative necrosis of connective tissue fascia [Table/Fig-4] confirming the diagnosis of necrotising fasciitis.
Discussion
Necrotising fasciitis was first defined by Wilson in 1952 as necrosis of the fascia and subcutaneous tissue with sparing of the muscle [1]. Necrotizing fasciitis is a rapidly spreading infection characterised by widespread necrosis of the subcutaneous tissue and fascia with associated systemic toxicity and extending along fascial planes[1,2]. Patients susceptible to this infection include those with advanced age, chronic renal failure, peripheral vascular disease, and diabetes mellitus [3].
Although, it can affect any part, the sites commonly affected are extremities, scrotum (Fournier’s gangrene) and perianal region [3].
Primary necrotising fasciitis of the breast is a rare entity. Shah et al., [4, reported the first case of necrotising fasciitis of breast in the year 2001. Since then only few cases have been reported in world literature. To the best of our knowledge three cases have been reported from India. We describe the salient features of these cases [Table/Fig-5].
As evident from the above published reports , Necrotising fasciitis of the breast affects lactating women and postmenopausal women. Necrotising fasciitis of the breast can also be misdiagnosed as Inflammatory Carcinoma, Cellulitis or Breast abscess [2-7].
Diagnosis is based on clinical examination showing signs of inflammation. However, because of thicker tissue between deep fascia and breast skin, cutaneous signs may not be apparent until the disease is well advanced [7,8]. So a high index of suspicion is necessary for timely diagnosis and prompt treatment of this disease. Diagnostic adjuncts like ultrasound and MRI are helpful in early recognition of the disease.
The treatment is mainly aggressive surgical debridement and broad spectrum antibiotics [8] apart from resuscitative measures from sepsis and shock. If detected early, breast salvage is almost always possible, whereas in extensive disease mastectomy may be necessary. The aim of the surgery must be to remove all infected tissue at the first debridement. Thorough, debridement should be done and deep fascia must be excised as much as feasible. A second look surgery may be planned after 24-48hrs depending on patient’s clinical situation [7,9].
Necrotising fasciitis of left breast extending to left arm

Histopathology (H&E, 10X) showing exuberant inflammatory granulation tissue
Histopathology (H&E, 40X) showing suppurative necrosis of connective tissue fascia
Salient features of the cases
| S. no | Author | Year | Salient features of the case | Treatment and Disease outcome. |
| 1 | Rajakannu M et al., [2] | 2006 | Necrotising fasciitis mimicking inflammatory carcinoma of the breast in a post menopausal women | Mastectomy was done. Patient recovered. |
| 2 | Venkatramani V et al., [5] | 2009 | Necrotising fasciitis of breast in a HIV positive middle aged women. | Mastectomy was done. Patient recovered. She was started on her anti-retroviral therapy subsequently. |
| 3 | Vishwanath G et al., [6] | 2011 | Necrotising fasciitis in a lactating women presenting in septic shock | Mastectomy was done. Patient recovered. Skin grafting of the wound done subsequently. |
| 4 | Present case | 2014 | Necrotising fasciitis of breast in a post menopausal, diabetic women presenting in septic shock | Wide debridement was done. Patient died on 2nd post operative day. |
Conclusion
1. Although necrotising fasciitis of the breast is very rare, the outcome of this condition could be rapidly fatal.
2. Early diagnosis and radical debridement can potentially cure this otherwise fatal disease.
3. A high index of suspicion by practicing surgeons and clinicians could help diagnose the disease early and in initiating the treatment.
[1]. B Wilson, Necrotising fasciitis.Am Surg. 1952 18:416-31. [Google Scholar]
[2]. M Rajakannu, V Kate, N Ananthakrishnan, Necrotizing infection of the breast mimicking carcinoma.Breast J. 2006 12(3):266-67. [Google Scholar]
[3]. S Hasham, P Matteucci, PR Stanley, NB Hart, Necrotising fasciitis.BMJ. 2005 330:830-33. [Google Scholar]
[4]. J Shah, AK Sharma, JM O’Donoghue, B Mearns, A Johri, V Thomas, Necrotising fasciitis of the breast.Br J Plast Surg. 2001 54:47-8. [Google Scholar]
[5]. V Venkatramani, S Pillai, V Venkatramani, S Marathe, SA Rege, JV Hardikar, Breast gangrene in an HIV-positive patient.Ann R Coll Surg Engl. 2009 91(5):W13-4.doi: 10.1308/147870809X401056 [Google Scholar]
[6]. G Vishwanath, SI Basarkod, Katageri Geetanjali M, Mirji Promod, Mallapur Ashok S, Necrotizing fasciitis of the breast with shock and postpartum psychosis.Journal of Clinical and Diagnostic Research. 2011 5:1117-19. [Google Scholar]
[7]. Chin-Ho Wong, Tan Bien-Kien, Plastic and Reconstructive Surgery 2008 122(5):e151-2. [Google Scholar]
[8]. S Nizami, K Mohiuddin, Mohsin-e-Azam H Zafar, MA Memon, Necrotizing fasciitis of the breast.Breast J. 2006 12(2):168-69. [Google Scholar]
[9]. A Subramanian, G Thomas, A Lawn, P Jackson, GT Layer, Necrotising soft tissue infection following mastectomy.JSCR 2010 :1-4. [Google Scholar]