Epidural Anesthesia for Caesarean Section in a Pregnant Patient with Pituitary Macroadenoma
Remadevi R1, D. Dinesh Babu2, K Sureshkumar3, Shubhada A. Patil4
1Assistant Professor, Department of Anaesthesiology, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India.
2Assistant Professor, Department of Anaesthesiology, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India.
3Associate Professor, Department of Anaesthesiology, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India.
4Associate Professor, Department of Anaesthesiology, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Remadevi R, Type-V-A-13, JIPMER Campus, Dhanvantri Nagar, Pondicherry-605006, India.
Phone: 919894243375,
E-mail: remadevi70@gmail.com
Anaesthesia for patient with pituitary adenoma posted for non-neurosurgical surgeries is a challenge to the anaesthesiologist with the risk of sudden change in intracranial dynamics during administration of spinal anaesthesia or during stress response of general anaesthesia. There is a chance of increase in tumour size during antenatal period. A careful assessment of pituitary function and a screening of visual field and fundus examination are essential to rule out any mass effect. We are presenting the anaesthetic management of patient with pituitary macroadenoma posted for elective caesarean section done under epidural anaesthesia due to its rarity.
Obstetric anaesthesia, Pituitary tumor, Regional anaesthesia
Case Report
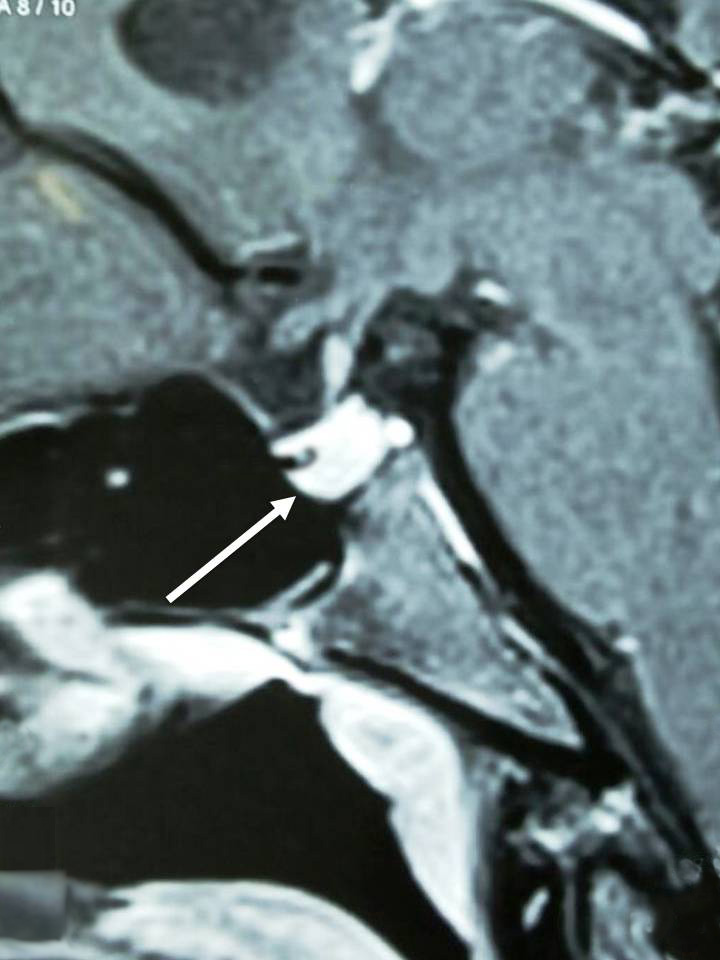
A 29-year-old primigravida with oligohydraminious was admitted at 37th week of gestation for elective Lower Segment Caesarean Section (LSCS). While she was being evaluated for infertility, she was diagnosed to have hypothyroidism, hyperprolactinemia secondary to pituitary macroadenoma. She was on Carbogolin 0.5mg twice a week, started six months before conceiving and continued till 7th month of pregnancy. There were no clinical signs suggestive of raised intracranial tension fundus was normal on ophthalmoscopic examination. Airway, system examination was normal. Routine haematological, biochemical and hormonal investigations were normal. CT-Scan [Table/Fig-1] and MRI [Table/Fig-2] taken one month before conception showed enlarged anterior pituitary with well-defined adenoma (11x12mm) confined to Sellaturcica (occupying right compartment) with mild deviation of infundibular stalk to the left. The lesion was abutting the medial wall of the cavernous internal carotid artery on the right side, with no features suggestive of invasion.
Patient was informed regarding the anaesthetic options and perioperative risk involved in regional and general anaesthesia. She preferred to remain awake during delivery. Aspiration prophylaxis was given 30 min before surgery. Patient was monitored using electrocardiogram, pulse‑oximeter and non-invasive blood pressure. Under aseptic precaution an 18 G epidural catheter was placed at L3-L4 inter space using 16G Tuohy needle. Epidural space confirmed with loss of resistance technique and test dose of 3 ml of 1.5 % lignocaine with adrenaline5μg/ml was given. Nine ml of 2% lignocaine was given in incremental doses after negative aspiration for blood and CSF. A wedge was placed under right side of pelvis to minimize aorto-caval compression.
A sensory level of T4 was achieved at six minutes. A 3.2 kg baby was delivered with Apgar score of eight at birth. The patient was hemodynamically stable. Postoperative analgesia was continued via epidural catheter with infusion of Fentanyl and Bupivacaine. Postoperative period was uneventful.
CT Scan Coronal image showing pituitary macroadenoma

MRI sagittal image showing pituitary macroadenoma
Discussion
Knowledge of the normal anatomy and physiology of pituitary gland is necessary to understand the pathophysiological effects relevant to anaesthesia and for appropriate preoperative preparation, intra and postoperative management of complications [1].
Pituitary tumours may present in different conditions such as, hormonal hyper secretory syndrome like hyperprolactinomas, acromegaly and Cushing disease or with mass effect causing visual disturbance and signs of raised intracranial tension. Sometimes they present with nonspecific symptoms like infertility, headache, epilepsy, pituitary hypo secretion or may be detected during imaging for some other condition [2]. During pregnancy, the pituitary gland undergoes global hyperplasia and volume may increase by 45% [3]. Tumour cells in patients with prolactinomas and that with growth hormone secreting tumour may exhibit symptomatic enlargement during pregnancy, either due to the growth‑promoting effect of oestrogens or due to high levels of circulating progesterone that occur with gestation. Based on their size prolactinomas are classified into macroadenoma (>1 cm) or microadenoma (< 1 cm) [4]. Medical management of prolactinomas is curative in 95% cases, in which prolactin concentration is restored to normal with dopamine agonist, bromocriptine. Carbergoline is an alternative to bromocriptine.
A careful assessment of pituitary function and a screening of visual field and fundus examination are essential to rule out any mass effect.
Mass effect of a tumour on adjacent structures is more likely to occur with non-functioning macroadenomas. By compression of pituitary gland in sellaturcica by haemorrhage into pituitary (pituitary apoplexy) or very rarely by postpartum pituitary infarction (Sheehan’s syndrome). Compression of optic chiasm results in bitemporal hemianopia. In pituitary apoplexy, third cranial nerve palsy can occur. Large tumours can cause obstruction to cerebrospinal fluid flow leading to increase in intracranial pressure [1] which may be acute and fatal in the peripatum period. We avoided general anaesthesia in this patient because of the possible risk of an acute increase in intracranial pressure associated with laryngoscopy and tracheal intubation. The patient preferred regional anaesthesia as well. Also an awake patient would alert early in the event of an intracranial complication. There is only one report of a subarachnoid block being used in a pregnant patient with glioblastoma for an emergency section due to foetal distress [5]. We avoided spinal anaesthesia because of possible decrease in intracranial pressure due Cerebrospinal Fluid (CSF) leak in postoperative period, if multiple attempts were made.
Akashi N et al.,[6] also described a similar case where, caesarean section was successfully performed with epidural anaesthesia, the pituitary tumour was removed trans-sphenoidally under general anaesthesia. Therefore, we decided to go ahead with epidural anaesthesia. There are reports of safe use of epidural block for labour analgesia and caesarean section in patients with intracranial tumours[7,8]. However, Hilt et al., [9] demonstrated that CSF pressure rises significantly even with 10 ml of bupivacaine administration in the epidural space in patients with reduced intracranial compliance. We had taken care to administer the epidural drug slowly to minimise this effect and there was no adverse event in the intra and postpartum period. There is a possible risk of accidental dural puncture during placement of epidural catheter. Performance of epidural by an experienced anaesthesiologist and use of ultrasound, if available, to measure the depth of needle placement may minimise this risk to a large extent.
Conclusion
The epidural anaesthesia may be used safely for caesarean section in patients with pituitary macroadenoma. However, we suggest that the epidural placement should be performed by an experienced anaesthesiologist preferably with ultrasonographic guidance.
[1]. M Smith, NP Hirsch, Pituitary disease and anesthesiaBJA. 2000 85:3-14. [Google Scholar]
[2]. A Levy, Sl Lightman, Diagnosis and management of pituitary tumoursBr Med J 1994 308:1087-91. [Google Scholar]
[3]. JF Gonzalez, G Elizondo, D Saldivar, Pituitary gland growth during normal pregnancy: An in vivo study using magnetic resonance imagingAm J Med 1988 85:217-20. [Google Scholar]
[4]. JV Kredentser, CF Hosking, JZ Scott, Hyperprolactinoma - a significant factor in female infertilityAm J Obstet Gynecol 1981 139:264-67. [Google Scholar]
[5]. PG Ata nassoff, BM Weiss, U Lauper, Spinal anaesthesia for caesarean section in a patient with brain neoplasmCan J Anesth 1994 41:163-64. [Google Scholar]
[6]. N Akashi, M Yoshida, A Yonei, Anesthetic management of a pregnant woman scheduled for cesarean sectionunder epidural anesthesia and simultaneous surgical removal of pituitary tumour under general anaesthesiaMasui. 2010 59(6):753-56. [Google Scholar]
[7]. T Goroszeniuk, RS Howard, JT Wright, The management of labour using continuous lumbar epidural analgesia in a patient with a malignant cerebral tumour.Anaesthesia. 1986 41:1128-29. [Google Scholar]
[8]. S.R Finfer, Management of labour and delivery in patients with intracranial neoplasms.Br J Anaesth 1991 67:784-87. [Google Scholar]
[9]. H Hilt, HJ Gramm, J Link, Changes in intracranial pressure associated with extradural anaesthesiaBr J Anaesth 1986 58:676-80. [Google Scholar]