Background: Orbitozygomatic fracture that most commonly accompanies craniofacial injury is a challenge for medical science to reduce complications and to attain aesthetically satisfying results.
Objective: To summarize our experiences with the optimum management of orbito-zygomatic fractures.
Materials and Methods: This retrospective study was aimed at investigating indications and surgical approaches for orbitozygomatic fractures with clinical follow-up, particularly with regard to postoperative complications. Since 2010, 100 cases with faciomaxillary injury were assessed for Orbitozygomatic fractures with the help of physical examination, non-invasive investigations including computed tomography of the orbit. Patients were retrospectively analysed for data, such as mechanism of injury, classification of fracture, and complications.
Results: Amongst 100 consecutive patients with orbito-zygomatic fractures an overwhelming majority were males (n=83). In the age distribution a great majority (45%) were in 30-45 years age group, followed by 15-30 years (22%) and 45-60 years (18%). So in the productive age group i.e. 15-60 years age group were affected mostly (85%) in our series. Among different injury mechanism, Road traffic accident affected most (69%) that landed up in orbito-zygomatic fractures followed by altercations (22%). We preferred Open reduction and internal fixation (ORIF) for 68% of the patients with orbito- zygomatic fractures, followed by closed reduction (12%).
Conclusion: Ophthalmology consultation is recommended for all patients presenting with orbitozygomatic fractures, and is essential for patients with orbital blowout fractures, based on the high incidence of clinical ocular findings and injuries in this subgroup of patients.
Introduction
Facial injuries are commonly associated with brain trauma. Their early diagnosis and management is important as delay in treatment may lead to permanent facial disfigurement. Facial injuries could vary from isolated soft tissue injuries to complex pan facial fractures. Fractures of orbital and zygomatic areas (orbitozygomatic) because of its close association with brain and globe form a triad of facial, brain and ophthalmic damage. Biomechanics of facial skeleton explains that the fractured zygomatic segments have six possible directions of motion: translation across x, y and z-axis; rotation about x, y and z-axis. The inferior orbital rim is a common location for displaced and comminuted fractures with an associated high velocity injury. Jelks described a 14-40 percent incidence of major intraocular injury in patients with zygomatic fractures involving the orbital floor. Management depends on a thorough preoperative physical examination, with special attention to the ophthalmologic assessment [1].
The patients presenting with orbitozygomatic fractures were studied with emphasis on causative factors, treatment and complications encountered subsequently.
Coronal and axial computed tomography is indispensable for classifying fracture and orbital association. For the optimum outcomes sufficient exposure and mobilisation of fracture segments are needed for successful anatomical positioning, accurate fracture reduction and effective fixation to prevent complications like enophthalmos and diplopia [2,3]. To share experiences with the optimum management of orbito-zygomatic fractures the authors summarised their experience in this study.
Materials and Methods
This was a retrospective audit done from 2010 onwards at Dayanand Medical College & Hospital, Ludhiana, Punjab, India. Patients who presented with history of trauma were assessed for facio-maxillary injury, brain injury and any associated ocular injury. Patients who had associated traumatic brain injury were assessed by the neurosurgeon and were operated for the same wherever indicated. The facio maxillary injury was dealt subsequent to (either simultaneously or later) neurosurgery procedure. The ophthalmological consult was taken and managed accordingly. Patients with isolated fracture of the zygomatic arch were treated with closed reduction. All other patients were treated with open reduction and internal fixation with mini plates. The fracture sites were exposed by lateral brow, subciliary, intraoral buccal incision for exposure of zygomatico frontal, inferior orbital rim and zygomatico maxillary buttress respectively. The plates used were made of titanium.
The Inclusion criteria were
History of trauma
Presentation in emergency department
Clinical evidence of facio maxillary injury
Exclusion criteria were
Refusal for surgery
Associated co-morbid conditions warranting delay in surgery
Results
Amongst 100 consecutive patients with orbito-zygomatic fractures an overwhelming majority were males (n=83).
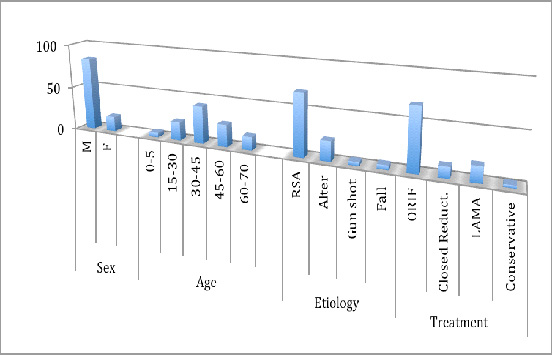
In the age distribution a great majority (45%) were in 30-45 years age group, followed by 15-30 years (22%) and 45-60 years (18%). So, the productive age group i.e. 15-60 years age group was affected the most (85%) in our series[Table/Fig-1] .
Among different injury mechanisms, the most common was road traffic accident (69%) that landed up in orbito-zygomatic fractures followed by altercations (22%), gun shot (4%) and fall (5%) [Table/Fig-1] .
Of the total 100 patients, 61% had associated traumatic brain injury. Of these patients, contusion was seen in 40% patients, sub dural hematoma in 25% patients, extradural hematoma was seen in 22% patients, pneumocephalus was in 15% patients and diffuse axonal injury in 10% patients. Twenty percent of the total 61 patients underwent surgery for brain injury.
For facio maxillary injuries, we preferred ORIF for good number of cases (68%), followed by closed reduction (12%). Remaining patients were managed conservatively [Table/Fig-1] .
Surgery was conducted with an average delay of 2.5 days after the incident. Sub ciliary incision was the most common surgical approach to the orbital floor. For orbital floor reconstruction titanium mesh (42.60 %) was most commonly used. There were 18% of patients who showed postoperative orbital complications: 7.0% suffered from persisting motility impairment, 14.0% from enophthalmos, 6.0% from persistent diplopia, 5.0% from ectropion, and 2.0% from orbital infection. Globe rupture was seen in 9.0% patients resulting in permanent blindness, 1.0% had plate exposure.
Showing distribution of sex, age, etiology and treatment
3 DCT reconstruction showing Bi lateral orbito zygomatic fracture

Discussion
Orbitozygomatic injuries are among the most common fractures encountered by the plastic surgeon. Appropriate management depends on an accurate diagnosis, focusing on the physical examination and data from computed tomography scans [4] .
The most common cause of facial fractures, in our study, was road traffic accidents. Males were more commonly involved than females. These findings were consistent with findings from other countries [5-9] .
Management of orbital and mid-facial fractures requires a thorough ophthalmic evaluation and precise imaging. Diagnostic advances and new surgical /imaging techniques have dramatically improved both the functional and aesthetic outcome of reconstructions. He D et al., in their study on 64 patients with orbitozygomatic fractures found navigation-guided surgery, and 3-dimensional (3D) modelguided surgery to be very effective tool in treating patients with enophthalmos [Table/Fig-2] [10] .
A principle goal of therapy is to anatomically reduce fracture segments and to restore a normal orbital volume as soon as possible. Luo JC et al., [11] has emphasised on need for early diagnosis and treatment for periorbital injuries. According to them fracture reposition and orbital wall reconstruction should be performed at an early period.
In a study at Limerick Regional Hospital, Ireland, among 148 patients (130 males, 18 females) all fractures were unilateral and ocular findings were present in 29 (20%) patients [12] .
In this study, zygomatic fractures were managed with closed reduction in 12% cases. The literature indicates that 10%–50% of all zygomatico maxillary complex fractures require no surgical intervention[13] . Mohammadinezhad C resorted to minimal invasive treatment for isolated zygoma fractures in the form of hook reduction and fixation with single miniplates. He demonstrated good aesthetic results in his case series of 17 patients [14] . Bezuhly M et al., have shown in their study that Gillies elevation combined with percutaneous Kirschner wire fixation provides facial contour restoration that is not significantly different from that of open reduction and internal fixation, with less soft-tissue morbidity. The technique is safe, easy to learn, and easy to perform, and should be considered in cases of isolated simple zygoma fractures [15] .
In most countries, traffic accidents are the leading cause of orbital fractures [16] .
Facial/ Orbital fractures are usually associated with ocular and intracranial injuries. Orbital fractures are usually part of more complex midfacial trauma. In our study, 18% patients had associated ocular involvement. Of these enophthalmos (14%) was the most common complication. Clauser et al., [17] defined enophthalmos as a backward, and usually downward, displacement of the globe into the bony orbit. In their study, 80 patients (52 cases of orbitozygomatic fractures and 28 late post-traumatic enophthalmos) were treated between January 1998 and January 2005. Fracture reduction in primary enophthalmos was performed. In enophthalmos as sequel, the treatment consisted of orbital reconstruction in combination with bone grafts harvested from calvaria, iliac crest, and/or orbital osteotomies.
According to Kovács AF, Ghahremani M, a patient with a zygomatic fracture and diplopia should be classified as having an orbitozygomatic fracture. In case of comminuted fractures, exploration of the orbital floor remains mandatory [18] .
Ong WC [19] reported Cervicofacial, retropharyngeal and mediastinal emphysema (a rare complication) after orbital fractures.
Traumatic brain injury concomitant with facial fractures is another common occurrence. In our series, 61% of the patients had associated brain injury of 114 mid-face fractures treated by Brandt KE et al., [20] over a one year period, 43 (38%) had a concomitant traumatic brain injury. The majorities, 36 (84%), were from motor vehicle accidents (MVAS). Frontal sinus and orbito ethmoid fractures were at the highest risk for injury, although orbitozygomatic fractures caused by MVAs also had a surprisingly high incidence of traumatic brain injury.
Strengths of our study
Firstly, the take home message from the outcome of our study is that, even in the resource poor settings in absence of state-of-art infrastructure in the tertiary care teaching institutes in Northern India, we shall be bold enough to keep us updated to work out on applications of novel surgical approaches of the international standard.
Secondly, in the light of the sincere data abstraction and analysis of our hands-on experiences on this improvised approach we will be definitely able to deliver qualitatively improved and better patient care to our future series of cases presented to us for Orbitozygomatic fractures with brain injury.
Limitations of the study
A major drawback of the presented approach is a relatively small sample size. Also, patients with associated other organ injuries, like chest and abdomen, have not been taken into consideration.
Future directions of the study
Future advances in the treatment of facial trauma most likely will involve more extensive use of endoscopy for minimally invasive repair of traumatic injuries. The advanced techniques involve using computer-imaging software that can compare the more nonfractured side and create a computer model for reconstruction planning. Image-guidance surgery systems may also play a role in optimising fracture reduction. Further, a larger clinical series with long-term follow-up will be needed to determine reproducibility and cost-effectiveness. In addition to bone repositioning, a future application may include simulation of craniofacial osteotomies.
Conclusion
Facio maxillary injuries are very common in trauma patients. Thorough multi disciplinary evaluation is a must to rule out concomitant injuries. The long-term prognosis after repair of zygomaticomaxillary complex (ZMC) fractures is very good.
Acknowledgement
Department of Ophthalmology, DMC & Hospital, Ludhiana, India.
[1]. GW Jelks, G La Trentra, Orbital fractures. In: Foster CA, Sherman JE, eds. Surgery of Facial Bone Fractures 1987 17th EditionNew York, NY:Churchill Livingston:67-91. [Google Scholar]
[2]. C Westendorff, D Gülicher, F Dammann, S Reinert, J Hoffmann, Computerassisted surgical treatment of orbitozygomatic fracturesJ Craniofac Surg 2006 17(5):837-42. [Google Scholar]
[3]. Y Kaufman, D Stal, P Cole, JR Hollier L, Orbitozygomatic fracture management.Plast Reconstr Surg 2008 121(4):1370-74. [Google Scholar]
[4]. LH Hollier, J Thornton, P Pazmino, S Stal, The management of orbitozygomatic fractures.Plast Reconstr Surg 2003 111(7):2386-92. [Google Scholar]
[5]. SK Punjabi, Habib-ur-Rehman AZ S Ahmed, Causes and management of zygomatic bone fractures at Abbasi Shaheed Hospital Karachi (analysis of 82 patients)J Pak Med Assoc 2011 61(1):36-9. [Google Scholar]
[6]. AM Batista, O Ferreira Fde, LS Marques, ML Ramos-Jorge, MC Ferreira, Risk factors associated with facial fractures.Braz Oral Res 2012 26(2):119-25. [Google Scholar]
[7]. S Olate, Jr Lima SM, R Sawazaki, RW Moreira, M de Moraes, Variables related to surgical and nonsurgical treatment of zygomatic complex fractureJ Craniofac Surg. 2011 22(4):1200-02. [Google Scholar]
[8]. S Gandhi, LK Ranganathan, M Solanki, GC Mathew, I Singh, S Bither, Pattern of maxillofacial fractures at a tertiary hospital in northern India: a 4-year retrospective study of 718 patientsDent Traumatol 2011 127(4):257-62. [Google Scholar]
[9]. PF Trivellato, MF Arnez, CE Sverzut, AE Trivellato, A retrospective study of zygomatico-orbital complex and/or zygomatic arch fractures over a 71-month period.Dent Traumatol 2011 27(2):135-42. [Google Scholar]
[10]. D He, Z Li, W Shi, Y Sun, H Zhu, M Lin, Orbitozygomatic fractures with enophthalmos: analysis of 64 cases treated lateJ Oral Maxillofac Surg 2012 70(3):562-76. [Google Scholar]
[11]. JC Luo, L Gui, ZY Zhang, L Teng, JM Zhu, TZ Hao, Early reconstruction of the periorbital injuriesZhonghua Zheng Xing Wai Ke Za Zhi 2008 24(5):362-64. [Google Scholar]
[12]. C Barry, M Coyle, Z Idrees, MH Dwyer, G Kearns, Ocular findings in patients with orbitozygomatic complex fractures: a retrospective studyJ Oral Maxillofac Surg 2008 66(5):888-92. [Google Scholar]
[13]. JM Joseph, IP Glavas, Orbital fractures: a reviewClin Ophthalmol 2011 5:95-100. [Google Scholar]
[14]. C Mohammadinezhad, Evaluation of a single miniplate use in treatment of zygomatic bone fracture.J Craniofac Surg. 2009 20(5):1398-402. [Google Scholar]
[15]. M Bezuhly, J Lalonde, M Alqahtani, G Sparkes, DH Lalonde, Gillies elevation and percutaneous Kirschner wire fixation in the treatment of simple zygoma fractures: long-term quantitative outcomesPlast Reconstr Surg 2008 121(3):948-55. [Google Scholar]
[16]. AA Cruz, GC Eichenberger, Epidemiology and management of orbital fracturesCurr Opin Ophthalmol 2004 15(5):416-21. [Google Scholar]
[17]. L Clauser, M Galiè, F Pagliaro, R Tieghi, Posttraumatic enophthalmos: etiology, principles of reconstruction, and correctionJ Craniofac Surg 2008 19(2):95-100. [Google Scholar]
[18]. AF Kovács, M Ghahremani, Minimization of zygomatic complex fracture treatment.Int J Oral Maxillofac Surg 2001 30(5):380-83. [Google Scholar]
[19]. WC Ong, TC Lim, J Lim, G Sundar, Cervicofacial, retropharyngeal and mediastinal emphysema: a complication of orbital fractureAsian J Surg 2005 28(4):305-08. [Google Scholar]
[20]. KE Brandt, GL Burruss, WL Hickerson, CE White, JB DeLozier, The management of mid-face fractures with intracranial injuryJ Trauma 1991 313rd Edition(1):15-9. [Google Scholar]