3D Laparoscopy - Help or Hype; Initial Experience of A Tertiary Health Centre
Diwakar Sahu1, Mittu John Mathew2, Prasanna Kumar Reddy3
1Registrar, Department of Surgical Gastroenterology and Minimal Access Surgery, Apollo Hospitals, Greams Road, Chennai, Tamil Nadu, India.
2Registrar, Department of Surgical Gastroenterology and Minimal Access Surgery, Apollo Hospitals, Greams Road, Chennai, Tamil Nadu, India.
3Senior consultant & Head of Department, Surgical Gastroenterology and Minimal Access Surgery, Apollo Hospitals, Greams Road, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prasanna Kumar Reddy,Department of Surgical gastroenterology, Apollo hospital, 21 Greams road, Chennai, Tamil nadu– 600006, India.
Phone: 09677184896
E-mail: drpkreddyapollo@gmail.com
Introduction: To evaluate the advantages of 3D laparoscopy and compare its significance with conventional 2D laparoscopy during various operative procedures.
Methods: During present study, two groups were formed. Group A included patients who were operated using 3D laparoscopic imaging and Group B consisted of operated patients by 2D laparoscopy. Operative performance of both the groups was compared in terms of operative time and quality of imaging.
Results: Operative time interval for various procedures was significantly less in Group A as compared to Group B. Also, imaging quality was far superior with use of 3D imaging system especially in terms of depth perception.
Conclusion: Advantages of 3D laparoscopy are well appreciated during operative procedures as previously documented by other studies in training models.
3D imaging, 3D laparoscopy, Laparoscopic surgery
Introduction
Laparoscopy has revolutionized our approach to a number of surgical problems and caused a re-evaluation of clinical strategies. Now it has become the standard treatment for majority of ailments including symptomatic gall stone disease, appendicitis, GERD and morbid obesity. Over past few decades, tremendous growth in minimally invasive techniques and technology has occurred. All this developments aim at minimising peroperative morbidities, providing rapid postoperative recovery and enhancing patient’s safety profile. One of the major limitations of conventional laparoscopy is lack of depth perception and tactile feedback. Introduction of robotic technology, which employs 3D imaging, has removed many of these technical obstacles. In 1993, Becker et al., reported that a 3D display might improve laparoscopic skills [1]. Since then many researchers have demonstrated benefit of 3D imaging [2]. Despite the significant advantages claimed, 3D systems have not been widely accepted. Poor image quality due to technological limitations of early 3D equipments and the high price of these systems could be the possible reasons. Also, most of the studies which showed superiority of 3D system have been conducted using endotrainer and experimental surgical model [3,4].
So, our present study intends to analyse the effect of 3D technology on operative performance during various elective laparoscopic surgeries and to assess its advantages and disadvantages over 2D laparoscopy.
Materials and Methods
A prospective cohort study was conducted where 3D laparoscopic setup (Viking 3D HD Vision System) was used to perform elective cases in our institute which is a tertiary health care centre. Total 53 patients were operated and all surgeries were performed by the same surgeon over a period of two months. The operating surgeon is a senior most laparoscopic surgeon with vast experience in laparoscopic surgery. During two months period, 13 cases were operated using 3D HD laparoscopy system (Group A) and 40 cases with the help of 2D laparoscopy setup (Group B). In both operative groups, 30º telescope was used. Patients were selected by random sampling and subjected to either operative group with informed consent. Elective cases of gall stone disease were included in the study and cases of carcinoma of gall bladder were excluded. Similarly, elective cases of reducible inguinal and incisional hernia were included and cases of irreducible, obstructed and strangulated hernia were excluded. Only benign case of ovarian cyst was included and cases of ovarian carcinoma were excluded. Patients who were subjected to distal gastrectomy and G-J were cases of corrosive injury of stomach, leading to gastric outlet obstruction. Also, for adhesiolysis, cases of subacute bowel obstruction were included and gangrenous or perforated bowel obstruction cases were excluded. Operative performance was evaluated and recorded in terms of intra-operative ease and difficulty, complications and operative time (interval from giving first incision to closure of last port site). Subsequently, the resultant data was compared with records of patients with similar clinical profile in whom same operation were performed using 2D laparoscopy (Group B). Scientific calculation was done using SPSS release 18.0 (Chicago, II, USA) windows software. Also, experience of operating surgeon in terms of superiority and inferiority of either technique was recorded using Likert scale.
Type and number of operated cases in both groups
| S. No | Type of procedure | No. of cases |
|---|
| 3D (n-13) | 2D (n-40) |
|---|
| 1. | Laparoscopic cholecystectomy | 8 | 29 |
| 2. | Laparoscopic inguinal hernioplasty (TAPP) | 1 | 4 |
| 3. | Laparoscopic incisional hernioplasty | 1 | 2 |
| 4. | Laparoscopic ovarian cystectomy | 1 | 1 |
| 5. | Laparoscopic distal gastrectomy with gastro-jejunostomy | 1 | 1 |
| 6. | Laparoscopic adhesiolysis | 1 | 3 |
Comparison of basic background characteristics of both the operative groups.
| S No. | Pre-operative charateristics | L.C | T.A.P.P | L.I.H | L.O.C | L.GJ | L.A |
| Study group | 3D | 2D | 3D | 2D | 3D | 2D | 3D | 2D | 3D | 2D | 3D | 2D |
| 1. | Sex (Female:Male) | 6:2 | 22:7 | 0:1 | 0:4 | 1:0 | 1:1 | 1:0 | 1:0 | 1:0 | 1:0 | 1:0 | 2:1 |
| 2. | Mean age (in years) | 49.7 | 44.2 | 51 | 58.5 | 49 | 52 | 38 | 27 | 40 | 36 | 45 | 56.7 |
| 3. | Mean BMI (in kg\m2) | 31.2 | 29.4 | 28 | 30.6 | 34.9 | 35.3 | 27.7 | 24.2 | 29.4 | 26.7 | 27.3 | 26.5 |
| 4. | Co-morbidities (diabetes malletus-DM & hypertension-HTN) | DM-3 HTN-4 | DM-12 HTN-16 | nil | HTN-1 | HTN-1 | DM-1 | nil | nil | DM-1 | nil | nil | HTN-1 |
Comparative operative time interval between two operative groups.
| S. No | Type of procedure | Operative time interval (in minutes) |
|---|
| 3-D laparoscopy | 2-D laparoscopy |
|---|
| 1. | Laparoscopic cholecystectomy | 40 | 54 |
| 2. | Laparoscopic inguinal hernioplasty (TAPP) | 75 | 87 |
| 3. | Laparoscopic incisional hernioplasty | 70 | 85 |
| 4. | Laparoscopic ovarian cystectomy | 25 | 42 |
| 5. | Laparoscopic distal gastrectomy with gastro-jejunostomy | 150 | 190 |
| 6. | Laparoscopic adhesiolysis | 20 | 27 |
Comparative evaluation of operative parameters.
| S. No | Operative parameters | 3D laparoscopy | 2D laparoscopy |
| 1. | Image quality | Superior | Inferior |
| 2. | Depth perception | Superior | Inferior |
| 3. | Lack of operative strain | Inferior | Superior |
| 4. | Intra corporeal knotting | Superior | Inferior |
| 5. | Hand eye coordination | Superior | Inferior |
| 6. | Advantage of 30º scope (lateral view) | Superior | Inferior |

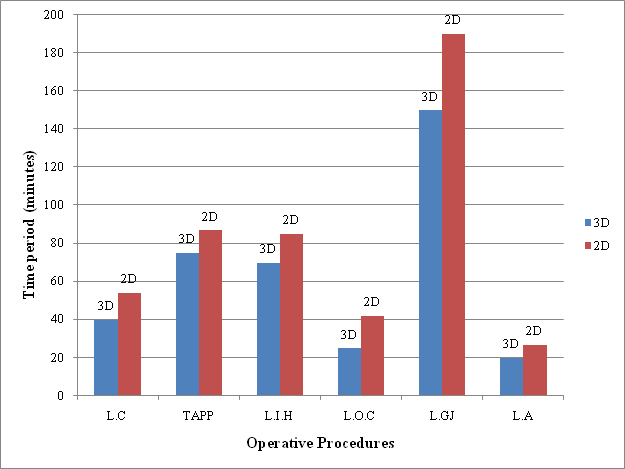
Comparative operative time period of Group A and B
Results
During our study total 53 patients were operated. In Group A, maximum operated cases were of cholelithiasis (eight). Other cases were that of inguinal hernia, incisional hernia, ovarian cyst, gastric outlet obstruction due to corrosive injury and post operative adhesion [Table/Fig-1]. Basic background characteristics of cases of both the operative Group A and B are shown and compared in [Table/Fig-2].
The average operative time in Group A was 40 minutes with longest time interval of 90 minutes and shortest being 20 minutes. On review of the data of 40 patients of 2D laparoscopic cholecystectomy, mean operative duration was 54 minutes and p-value after comparison of two groups was 0.04 (<0.05). Similarly, operative time interval for other procedures of two groups was compared [Table/Fig-3]. As single surgeon carried out all the procedures, a comparative evaluation was made in terms of operative imaging parameters like image quality, depth of perception, operative strain including headache, dizziness and eye strain; hand eye coordination and ease of intra corporeal suturing. All these parameters were rated as superior, inferior or equivocal [Table/Fig-4]. There were no intra operative complications like significant bleeding, bile duct injury, access injury or any visceral injury in both the groups. Postoperative period was devoid of any morbidity or mortality and all patients recovered well as per expectation.
Discussion
The prime disadvantage of 2D imaging system is lack of depth perception. The significant improvement in 2D image display quality has aided in overcoming this limitation. Moreover, skilled 2laparoscopic surgeons surmount this by extracting ‘pictorial’ depth cues from conventional images [4,5].
With the use of advance 3D laparoscopic system, the limitations of 2D laparoscopy can be overcome. Imaging in 3D system is obtained by either a dual-lens system or a single-lens system [6]. In dual-lens system, which was employed in our study, two separate lenses are present within a single laparoscope along with two cameras. Each camera captures their respective images, which are then displayed and synchronized on either a head-mounted display (active system) or a video monitor (passive system) [Table/Fig-5]. In the present study, a variety of cases were selected to assess the performance of 3D technology. In cholecystectomy procedures, anatomy of Calot’s triangle and identification of cystic duct and artery was very well appreciated as compared to 2D imaging. This can aid in minimising the margin of error during laparoscopic cholecystectomy. The only drawback was difficulty in posterior dissection of Calot’s triangle which was due to inability to rotate the light cable head of dual lens 3D telescope. Similarly, during laparoscopic TAPP because of clear anatomy, dissection of cord structures was comparatively easy and prompt. In order to view the under surface of abdominal wall during laparoscopic incisional hernioplasty and adhesiolysis, telescope was detached from camera, rotated upside down and refixed.
On comparison of mean operative time of the two groups, it was quiet evident that surgeries executed using 3D imaging took less time [Table/Fig-6]. Our finding was supported by a study carried out by O.J Wagner et al., in which they demonstrated that performance speed can be increased by 60-70% with use of 3D imaging system [7]. Mean time for laparoscopic cholecystectomy of Group A and B were 40 and 54 minutes respectively. P-value was 0.04 (< 0.05) which was significant. In a previous study done by Rakesh et al, it was mentioned that learning curve for 3D laparoscopy procedures involves five cases [8]. But this does not holds true in our study as time taken to perform the first surgery (laparoscopic cholecystectomy) in Group A was 20 minutes. In our opinion, if a surgeon is well trained in conventional laparoscopy, then he or she will accustom to advance technology more readily. Also, there are several studies stating that trained as well as novice surgeons perform well with 3D training model in comparison to 2D training model [9,10]. In advance laparoscopic surgery like distal gastrectomy with gastrojejunostomy, operative time was significantly reduced (150 mins vs 190 mins).
On comparison of image quality between two groups, except for operative strain and inability to rotate light cable, other constraints were enhanced in 3D HD system. Depth perception and hand eye coordination were excellent with 3D imaging system leading to accurate and swift dissection as well as better intra-corporeal knotting.
The role of robotic technology in laparoscopic surgery has been debated since its invention. The technical supremacy of these systems is mainly because of increased degrees of freedom of equipments, elimination of tremor and 3D imaging. But high cost of equipment, steep learning curve and lack of ability to feel the tissue are certain limiting factors for this new emerging technology
Modern 3D HD system offers many advantages of robotic surgery at low cost and with use of conventional laparoscopic equipments.
Conclusion
Athough the superiority 3D laparoscopic system over 2D systems is yet unsettled, the potential benefits of 3D imaging are well documented. These benefits might translate into enhanced operative times and greater surgeon comfort, making laparoscopy quicker and less prone to error. Our study may be decisive in stating that advantages of 3D laparoscopy are well appreciated in training models as well as during operative procedures.
Acknowledgement
I would like to thanks Dr. M.J Mathew for compilation of data and Mr. Pawan kumar for his valuable support.
[1]. H Becker, A Melzer, MO Schurr, 3-D video techniques in endoscopic surgery.Endosc Surg Allied Technol. 1993 1:40-46. [Google Scholar]
[2]. HR Patel, MJ Ribal, M Arya, Is it worth revisiting laparoscopic threedimensional visualization? A validated assessment.Urology. 2007 70(1):47-9. [Google Scholar]
[3]. HT Tevaearai, XM Mueller, LK Von Segesser, 3 -D vision improves performance in a pelvic trainer. Endoscopy. 2000 32:464-68. [Google Scholar]
[4]. JC Byrn, S Schluender, CM Divino, Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System.Am J Sur 2007 519:22 [Google Scholar]
[5]. J Hofmeister, TG Frank, A Cuschieri, Perceptual aspects of two dimensional and stereoscopic display techniques in endoscopic surgery: review and current problems.Semin Laparosc Surg. 2001 8(1):12-24. [Google Scholar]
[6]. UD Mueller-Richter, A Limberger, P Weber, Possibilities and limitations of current stereo-endoscopy.Surg Endosc. 2004 18:942-47. [Google Scholar]
[7]. Wagner O J, M Hagen, A Kurmann, Three-dimensional vision enhances task performance independently of the surgical method.Surg Endosc. 2012 26:2961–-68. [Google Scholar]
[8]. Sinha Rakesh, Sundaram Meenakshi, raje Shweta, 3D Laparoscopy-Technique and Initial experience with 451 cases.Gynecol Surg. 2013 :123-28. [Google Scholar]
[9]. V Falk, D Mintz, J Grunenfelder, Influence of three-dimensional vision on surgical telemanipulator performance.Surg Endosc. 2001 :1282-88. [Google Scholar]
[10]. N Taffinder, SC Smith, J Huber, The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons.Surg Endosc. 1999 :1087-92. [Google Scholar]