Giant Follicular Cyst of Ovary in an Adolescent Girl
Disha Rajput1, Jaya Gedam2, Minal Bhalerao3, Ponambalaganpathi A Nadar4
1Associate Professor, Department of Obstetrics and Gynaecology, ESI PGIMSR MGM Hospital, Parel, Mumbai, India.
2Associate Professor, Department of Obstetrics and Gynaecology, ESI PGIMSR MGM Hospital, Parel, Mumbai, India.
3Senior Registrar, Department of Obstetrics and Gynaecology, ESI PGIMSR MGM Hospital, Parel, Mumbai, India.
4House Officer, Department of Obstetrics and Gynaecology, ESI PGIMSR MGM Hospital, Parel, Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Disha Rajput, Department of Obstetrics and Gynaecology, ESI PGIMSR MGM Hospital, Parel, Mumbai-400012, India.
Phone: 9819720141 (Mangalore),
E-mail: disharajput@yahoo.co.in
Cystic abdominal lesions are extremely common in adolescent girls and are now diagnosed more frequently due to the availability of better imaging modalities. Presentations as huge cysts have become rare as most of them are diagnosed and treated early. Adolescent girls presenting with huge benign abdominal cysts is not uncommon, most of them due to serious cystadenomas of the ovary, but large follicular cysts are rare. We present a 13-year-old girl who presented with a large abdominal mass which was subsequently diagnosed as juvenile follicular cyst of the ovary.
Dysfunctional ovulation, Follicular Cyst
Case Report
A 13-year-old girl was referred to us in view of a large abdominal mass. Ultrasonography of the abdomen had been reported as ovarian tumour. She had presented with a history of abdominal pain and distension since last 15 days. The patient had attained menarche at the age of 12 years but had amenorrhoea for the last three months. An elder brother had died of lung cancer at the age of 15 years.
On examination, her weight and height were 38 kg and 140cm (BMI 19.4). Vital parameters were stable. There was no pallor, icterus, oedema or lymph node enlargement. The abdomen was grossly distended. We palpated a large cystic non-tender mass arising from the pelvis and extending up to the epigastrium.
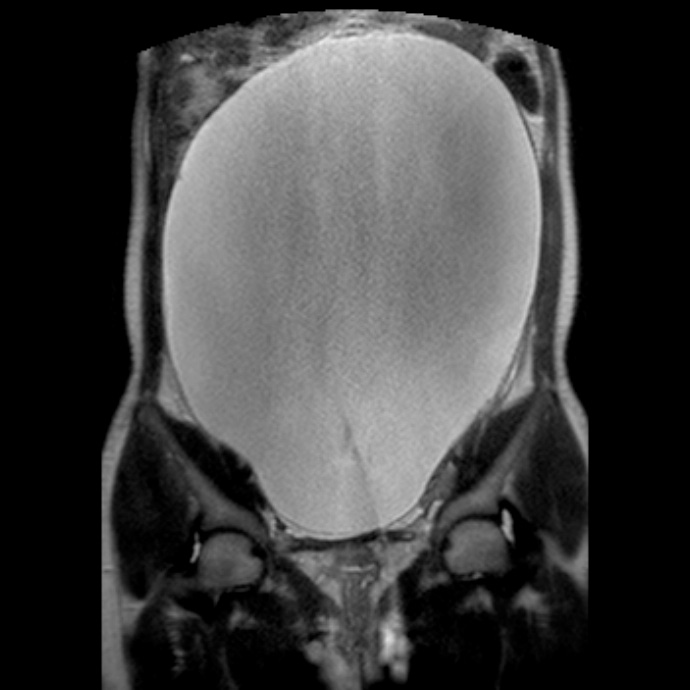
Hemoglobin was 10g/dL, the total and differential white blood cell count was within normal limits. Carcino-embryonic antigen – 125 (CA-125) was 55 IU/ml (normal < 35 IU/ml). Magnetic resonance imaging of abdomen and pelvis [Table/Fig-1] revealed a thin-walled cystic lesion of size 30 x 22.7 x 14.1cm. A few thin hypo-intense septations were seen on T2 weighted images. No solid components were seen. The mass could not be differentiated from the left ovary. The right ovary was normal. Moderate hydronephrosis and upper hydroureter were noted on the right side.
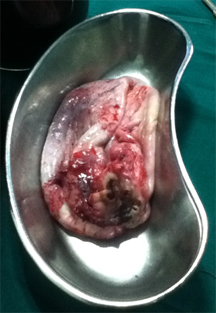
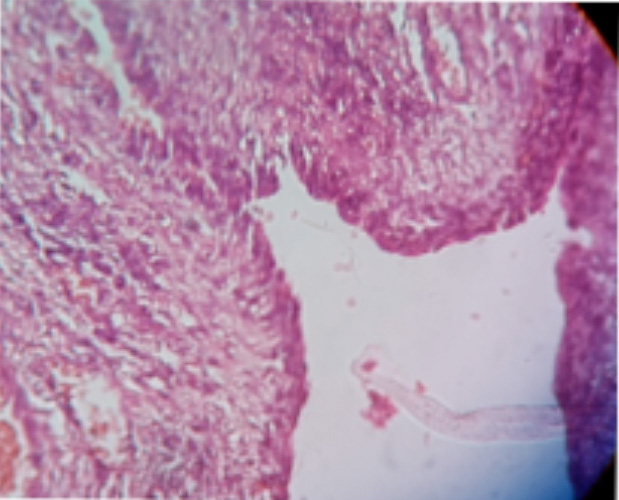
We considered a diagnosis of serous cystadenomas in view of the size and marginal elevation of CA-125. We took 2-3 inches suprapubic incision and aspirated 6-7 liters of straw-coloured fluid from the cyst [Table/Fig-2]. Cytology of the fluid showed a few benign epithelial cells and no malignant cells. No normal ovarian tissue could be identified and we removed the cyst. Histo-pathological examination of the cyst wall [Table/Fig-3] was reported as juvenile solitary follicular cyst with no evidence of malignancy. The patient got her periods on the third day after surgery. The intraoperative and postoperative course was otherwise uneventful and we discharged the patient on the ninth postoperative day. At follow up a month later, the child was doing well.
Discussion
Ovarian cysts are very common in the adolescent. Of these follicular cysts are the most common and occur due to dysfunctional ovulation with persistence of the remaining follicle. These cysts areusually 2 to 3 cm in diameter and resolve during the second half of the menstrual cycle. Most girls with follicular cysts present with abdominal pain and will often report irregular menses as well [1]. If ovulation does not occur, these follicular cysts can continue to grow under hormonal stimulation, occasionally to sizes as large as 8 cm [2]. However, cysts as large as seen in our patient are rare.
Our initial diagnosis was serous cystadenoma of ovary. Only on subsequent histopathology of the lesion was a diagnosis of benign follicular cyst of the ovary established. The diagnostic approach should be directed to differentiating benign conditions like follicular cysts from neoplastic lesions [3].
The aim of treatment are resolution of symptoms and preservation of ovarian tissue for future fertility. Follicular cysts in adolescents often regress without further treatment [4]. Hormonal suppression, such as with oral contraceptive pills, does not change the outcome and is not recommended [1].
Surgery is indicated in persistent or symptomatic cysts. The surgical options include aspiration of the cyst, fenestration or cystectomy. The reported recurrence of ovarian cysts in postmenarchal women after ultrasound- guided or laparoscopic aspiration ranges from 33% to 84%.Laparoscopic exploration with unroofing or excision of the cyst is considered the procedure of choice for a persistent or symptomatic functional ovarian cyst in the adolescent patient [1].
Magnetic resonance imaging of abdomen and pelvis (coronal section) T2 weighted image showing a large ovarian cyst occupying the whole abdomen
Gross specimen of the giant ovarian cyst removed by surgery
Histopathology slide showing preserved theca cell lining as in case of follicular cyst
Conclusion
Early diagnosis of ovarian tumours in adolescents is important. Since most of these tumours are benign, surgical treatment should be conservative to minimise the risk of subsequent infertility.
Acknoledgement
We would like to thank Dr Preeti Shanbaug Professor Paediatrics for guiding us, Dr Nilima Kshirsagar, Dean for permitting us to publish this manuscript.
[1]. ML Brandt, MA Helmrath, Ovarian cysts in infants and children.Semin Pediatr Surg. 2005 14:78-85. [Google Scholar]
[2]. P Kumar, N Malhotra, 2008 p7th EditionNew DelhiJaypee Brothers Medical Publishers (P) Ltd;:524-560. [Google Scholar]
[3]. P Tessiatore, R Guanà, A Mussa, L Lonati, M Sberveglieri, L Ferrero, When to operate on ovarian cysts in children?.J Pediatr Endocrinol Metab. 2012 25:427-33. [Google Scholar]
[4]. DL Cass, E Hawkins, ML Brandt, Surgery for ovarian masses in infants, children, and adolescents: 102 consecutive patients treated in a 15-year period.J Pediatr Surg. 2001 36:693-99. [Google Scholar]