Indigenization of dental industry in India has ironically been a low priority area for an economy that has a huge trade deficit as well as highest numbers of poor and needy people in the world. With curbing of import restrictions by government in last decade of the 20th century, perennial businessmen flooded local markets with healthcare equipment of dubious quality imported from the Far East. Quality assurance and nationalist sentiments of self-reliance were replaced by corrupt trade practices while lack of research & development (R&D) continued to push the import bill higher with each passing day. Ongoing global recession added to the woes of ailing economy where social welfare programs, including primary healthcare, were at receiving ends of skewed budgetary allocations since government did not have sufficient funds to spare. A glaring outcome of that is the low per-capita expenditure on public health in the country, in spite of recommendations to the contrary.
For millions of Indians who suffer from dental ailments, consulting a dental surgeon remains an elusive dream, especially in rural areas. High capital required to establish dental operatories in rural outposts, i.e. Primary Health Centers (PHCs), is an obvious impediment. Dental vans owned by teaching institutions and philanthropic organizations have limited operational capability in rural terrain due to lack of motorable roads. Portable dental units are an alternative, but not the imported ones since they are costly and their spares are scarce. Indigenization of technology, therefore, is the only way forward.
Portable dental services eliminate the transportation barrier by bringing the service to the client. The portable dental chair provides a greater assistance to disabled clients living in those out of reach places. They make it possible for the elderly to receive the care they deserve. The mobile and portable dental services also enable care for the elderly in their homes or care facilities [1–3].
The basic portable dental unit includes an operator light source, an examination kit, a portable head rest, and a first aid kit for dental purposes. These portable dental units used have a rotary instrument and an operator light fixture that is packed in two cases. More complex portable units include a vacuum canister, ultrasonic scaler, radiographic equipment along with compressors for air-water syringes and high and low speed handpieces. This equipment is stored and transported in durable boxes and cases [4,5]. The basic rationale for these chairs is to allow provision of simple filling and basic preventative treatments such as fluoride therapy and fissure sealants, but they remain largely unevaluated.
Thus, the aim of the current study is to compare the financial gains that can be made in primary oral healthcare delivery by cost-efficiency analysis of indigenously fabricated portable dental units, transported to camp sites in small vehicles.
Materials and Methods
The present study is based on a portable dental unit designed and fabricated indigenously by author (AG) in the year 2005, which is being utilized ever since for delivery of primary oral healthcare in remote and rural areas of Jaipur (northern India.) [Table/Fig-1,2] depict portable dental unit in working (ready-to-use) and folded (take-away) positions. Its features are described in [Table/Fig-3].
Portable dental unit in working (ready to use) position

Portable dental unit in folded (take - away) position

Showing features of portable dental unit
| Features |
|---|
| Length | Main seat: 18 inches. Back rest: 253 inches (moveable 0° to 90°). Leg rest: 22 inches (moveable 0° to 90°). Total length: 63 inches (5 feet 3 inches) |
| Width | 18 inches (1½ feet) |
| Height | 24 inches (2 feet) |
| Weight | 30 kilograms |
| Attachments | Halogen light, manual compressor, ultrasonic scaler (piezo-electric), micromotor machine with hand-piece and burs |
| Cost | Indian Rupees (Rs.) 8000 ($ 145) for portable Dental chair. Rs. 15,000 ($ 272) for attachments. Total Cost of portable Dental unit: Rs. 24,000 ($ 417) |
| 59 (35.76%) | 117 (70.91%) |
The range of services provided using portable dental unit include screening, oral prophylaxis, simple tooth extractions, restoration of decayed teeth using Atraumatic Restorative Treatment (ART)/temporary fillings, access opening of deeply carious teeth, and impression making for removable partial dentures (RPD)/complete dentures (CD.) A team of resident dental surgeons posted in the department of Public Health Dentistry of Rajasthan Dental College (RDC), Jaipur, delivered primary oral healthcare using the portable dental units in rural field practice area of the institute. Data related to services provided since inception (2005) till date (2012) were retrieved from the institutional records and arranged according to each financial year (i.e. April 1 to March 31) for analysis.
Cost-efficiency ratio was calculated on the basis of (a) input, i.e. expenses, and (2) output, i.e. number of patients treated. The expenses included in the present study were further divided into two: (1) direct cost, i.e. capital cost of fabricating portable dental unit, (2) indirect cost, i.e. transportation of portable units to the camp site, dental materials/medicines used while performing various procedures on the unit, publicity and allowances (DA) paid to personnel operating the unit. In other words, direct costs were the costs of all activities involved in the actual provision of services, i.e. they are costs of production. Indirect costs were the costs of activities involved in supporting the provision of care, i.e. they are costs of program.
Operational efficiency (i.e. the ratio between the input to run a dental care program and the output gained from the program) of portable dental unit was also compared with that of a dental van, which served as a positive control. Two such vans (with two fixed dental chairs each) operated by other dental colleges located in Modinagar and Bhopal were selected for comparison since they were serving similar field practice areas (northern India) and providing the same types of primary oral healthcare services. Observations related to cost and feasibility of utilizing dental vans were provided by the primary author (PG) from these locations and compared with that of the portable dental unit.
Results
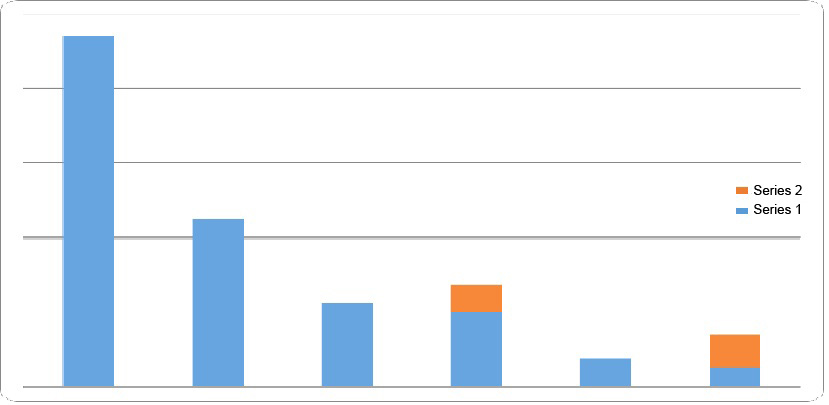
A total of 223 camps were organized using the indigenously fabricated portable dental unit in remote and rural areas of Jaipur from April 2005 - March 2012. A total of 52,900 patients were provided primary oral healthcare services at these camps, which included 23,615 (44.6%) screenings, 11,226 (21.2%) oral prophylaxis, 5613 (10.6%) tooth extractions, 4989 (9.4%) temporary fillings, 1814 (3.4%) fillings using ART, 1843 (3.5%) access openings for deep caries, 2184 (4.1%) impression makings for RPDs and 1265 (2.4%) impressions makings for CDs. [Table/Fig-4,5] depict the distribution of services provided during the study period.
Services provided using indigenously fabricated portable dental units
| Year* | No. of Camps conducted | No. of Patients treated | Direct Cost** | Indirect Cost |
|---|
| 2005-06 | 32 | 9133 | Rs. 96,000 ($ 1745) | Rs. 256,000 ($ 4655) |
| 2006-07 | 32 | 8515 | - | Rs. 256,000 ($ 4655) |
| 2007-08 | 33 | 8694 | - | Rs. 264,000 ($ 4800) |
| 2008-09 | 32 | 8019 | - | Rs. 256,000 ($ 4655) |
| 2009-10 | 33 | 8446 | - | Rs. 264,000 ($ 4800) |
| 2010-11 | 32 | 7385 | - | Rs. 256,000 ($ 4655) |
| 2011-12 | 29 | 2708 | - | Rs. 232,000 ($ 4218) |
| TOTAL | 223 | 52900 | Rs. 1,880,000 ($ 34,181) |
*Year denotes Financial Year (April to March)
**Four (4) portable Dental units used for treatment in all the camps
Frequency of different primary oral healthcare services provided during 2005-12
An initial, one-time direct cost was incurred on fabricating four portable dental chairs that amounted to Rs. 96,000 ($ 1745). The indirect cost of service provision was variable during each financial year and totaled Rs. 1,784,000 ($ 32,436) for the entire study period (seven years). Cost-efficiency was calculated by the formula: total cost (direct + indirect) of service provision ÷ total numbers of patients who used the services in the same period. This works out to Rs 35.53 per person ($ 0.65 per person) spent on provision of primary oral healthcare using indigenously fabricated portable dental unit.
[Table/Fig-6] summarizes the observations made by authors in relation to operational efficiency of the portable dental unit vis-à-vis dental van. Cost-minimization of primary oral healthcare service delivery in rural areas appears to be achievable using portable dental units due to their lower fabrication and maintenance cost. Feasibility of domiciliary visits for elderly, handicapped and other special groups is an additional advantage. However they have inherent limitations in terms of additional shelter and time required setting up the operatory. Also range of equipment and level of infection control achievable is a constraint.
Operational efficiency of portable dental unit vis-à-vis dental van in service provision
| Variable | Portable Dental Unit | Dental Van |
|---|
| Capital cost (average) | Rs. 24,000 ($ 417) | Rs. 1,20,000 ($ 2181) |
| Maintenance | Negligible | Required |
| Depreciation | Less | More |
| Operatory | Additional space or shelter is required to create an operatory | Readymade operatory |
| Time required to setup the unit | More | Minimal |
| Domiciliary visit | Feasible | Difficult |
| Range of equipment | Basic | More sophisticated |
| Level of infection control | Limited | Higher |
Discussion
Portable dental equipment has been defined as any non-facility in which dental equipment, utilized in the practice of dentistry, is transported to and utilized on a temporary basis at an out of office location including, but not limited to (a) another dentists’ offices, (b) patients homes, (c) schools, (d) nursing homes, or (e) other institutions. The concept of portable dental equipment dates back to 1617 when John Woodall, Surgeon General to East India Company produced details of the contents of surgical chests which included instruments for scaling, gum treatment and extractions [6]. Innovation in Dental field equipment made rapid strides during the two World Wars [7] and subsequently its use spread to the civilian sector. One of the earliest documented uses of portable dental equipment in general population is from Malaysia where ‘flying squads’ were reported to provide oral healthcare services to rural population during 1952 to 1963 [8]. Today a variety of portable dental equipment is available that includes foldable dental chairs, hand held intra-oral radiographic machines, suitcase or trolley units having attachments for ultrasonic scalers and airotor/micro-motor hand pieces, high and low speed suction, built-in compressor systems, lathes and portable dark rooms.
However, costs of such equipments remain high, which undermines their utilization in the groups that they are intended to target. At times, initial cost of purchasing portable dental equipment can even exceed the cost of equipping a private practice operatory. Overcoming cost barrier was the primary motivation for authors to indigenously develop and evaluate efficiency of portable dental unit in the present study. Efficiency has been defined as the extent to which a program has converted or is expected to convert its resources/inputs (such as funds, expertise, time, etc.) economically into results in order to achieve the maximum possible outputs, outcomes, and impacts with the minimum possible inputs. Cost-efficiency is the extent to which a program has achieved or is expected to achieve its results at a lower cost compared with alternatives. Shortcomings in cost-efficiency occur when the program is not the least-cost alternative or approach to achieving the same or similar outputs and outcomes. In this study assessment of efficiency was made by relating the results of operating the portable dental unit to its costs. Ideally this should attempt to put a monetary value on the benefits arising from the activities of the program, compare these with the costs of the program, and calculate the internal rate of return that equalizes the present value of the benefits and costs. But a monetary quantification of the program’s outputs and outcomes is problematic and would have been based on potentially controversial assumptions. Hence the assessment of efficiency focused on a simple ratio, i.e. the number of patients provided dental care per thousand rupees/dollars invested.
The cost-efficiency analysis showed that primary oral healthcare delivery using indigenously fabricated portable dental units was achievable at extremely economical rates ($ <1 per person.) This successful attempt at indigenizing technology to reduce cost was inspired by and similar to innovative attempts undertaken elsewhere. For example in Thailand where Mahidol university dental foundation collaborated with Thai dental products company to locally produce portable dental chairs with units. These turned out to be not only far less expensive ($ 2000) but also much lighter than their foreign counterparts [9]. Another successful dental care program using portable dental equipment for children residing in remote areas has been reported from El Salvador [10]. In this program the camp site was divided into four sections: one for dental examination, second to administer topical fluorides, third to distribute free toothbrushes as well as coloring books on dental prevention, and fourth section was dental surgery. Approximately 100-150 children were served every day at the camp and 20 communities were covered in a period of two weeks. Cost of providing dental care to the children was $ <3 per child and 11,000 children were covered in a period of six years by conducting two visits each year with a gap of six months duration. Similarly university of southern California’s mobile clinic program began in 1965 when John Ronnau, a member of the school’s oral surgery faculty, his family and a few dental students visited a remote site in Mexico to provide emergency dental care and oral health education. In 1968, when the students identified an underserved population closer to home, the program’s focus shifted to serving the dental needs of migrant workers in central and southern California. They devised the “octopus,” a method for running a few air-turbine hand pieces with a paint compressor, which allowed eight students to work at once. They also mounted an old X-ray unit on the back of a truck to improve their diagnosis [11]. In another, ‘right to you’ provided dental hygiene services on locations at a work camp in Alberta once a month for two years period. A room was constructed according to specifications to hold the mobile equipment [12]. A collaborative, comprehensive preventive oral health program between university of Missouri – Kansas City school of dentistry, the Olathe school district collectively worked to provide school-based services to disadvantaged children using portable dental equipment operated by dental hygiene students [13]. Oral prophylaxis, radiographs, sealants, fluoride varnish, oral health education and nutritional counseling to 339 children was provided under this program named ‘miles of smiles clinic.’ Upon re-evaluating at the end of school year, 11% of children had successfully begun the transition process of seeking restorative care from a local dentist.
Comparison of portable dental units with dental vans was made on the assumption that both attempt to deliver similar services. While a range of potential adverse events were acknowledged in both situations, the potential clinical significance of these events is minimal justifying cost-minimization using the indigenously fabricated portable dental unit. Although indigenously fabricated portable dental units cost just a fraction of operating dental vans, it may not always be the only factor governing choice of strategy in primary healthcare delivery. Hence qualitative observations were also recorded in this study, which found that prime advantage of portable dentistry includes eliminating the transportation barrier by bringing services to patients’ doorsteps, especially the elderly and institutionalized. Since treatment is done in a room that is familiar to them, patient feels more comfortable and the motivational barrier is also removed. Main disadvantage of portable dentistry is the time, space and equipment constraints that affect productivity. Also most of the complex surgical and follow-up procedures like Orthodontics and prosthesis fabrication cannot be carried out unless there are fixed clinics. Hence this study does not underestimate utility of dental vans but underscores a viable alternative in situations where capital cost is a limitation.
These observations are in agreement with other studies showing merits and demerits of dental vans over fixed clinics. For example a community trial held in India found that using portable dental units to provide on-site treatment in outreach areas was a feasible option in patient care [14]. This study also highlighted merits of dental vans in primary oral healthcare provision vis-à-vis fixed clinics. In another study in Michigan the overall cost in a five year school based comprehensive programme was estimated [15]. Procedures included ingestion of fluoridated water, oral hygiene education programs, dental examinations, prophylaxis, acidulated phosphate fluoride gel (1.23%) applied in trays, pit and fissure sealants (BISGMA) on occlusal surfaces of all eligible posterior teeth and provision of all restorative care. The vans were purchased and fully equipped for a total cost of $75,000. The five-year-cost of operating the two mobile vans was $13,727. This represents a facility cost of $18 per year per student involved in the project. By including personnel and other costs, the total cost per student was $146.58 per year. A similar study was conducted which compared the costs of providing children’s dental services in three practice settings: private practices, public mobile clinics, and public fixed clinics [16]. Some 15,000 children were provided comprehensive dental care over a three-year period. Costs were divided into direct and indirect categories. The results indicate that costs per visit and per child were lowest in mobile clinics and highest in private practices. A study by Doherty and Vivian focused on direct and indirect costs in their economic analysis [17]. They evaluated the Chattanooga Project, a publicly funded children’s dental care program, over a three-year period from 1971-1973. The program provided dental services in three different settings, private or public permanent clinics, and public mobile clinics. Overall, the average direct and indirect costs were lowest in the mobile clinics, and highest in private practice permanent clinics. Average total costs were $50.73 per patient (PP) and $20.57 per patient visit (PPV) in the mobile clinics compared to $64.16 PP and $30.47 PPV in private practice permanent clinics. Direct costs were $38.08 PP and $15.44 PPV in the mobile clinics compared to $48.21 PP and $22.89 PPV in private permanent clinics and $43.52 PP and $16.90 PPV in public permanent clinics. This study was extended to a full five-year period and findings corroborated the results from the first three years. In terms of direct costs, cost PP was $35.49 and cost PPV was $14.74 at the mobile clinics, compared to $46.56 and $23.59 in the permanent clinics. The indirect costs were also lowest in the mobile clinics, though less significantly, and the differences were attributable to transportation costs. The cost of transport for the mobile clinics was $1.38 per child compared to $3.27 per child for the permanent clinics. Another study in Thailand focused on comparing the unit costs of dental services for school children produced in two settings, hospital-based permanent dental clinics and community-based mobile dental clinics [18]. The unit costs of sealants and extractions in the mobile clinics were approximately 41 bahts less than the same services produced at the permanent dental clinic and the cost of amalgam filling was 10 bahts less in the mobile clinics but cost of scaling was about eight bahts higher in the mobile clinic compared to the permanent clinic.
Within the limitations of the present study it can be recommended that public health programs should combine elements from portable equipment along with dental vans to create a hybrid system. Clinical service delivery with portable equipment has been shown to be most productive in a facility where set-up and breakdown occurs only once [19]. This can comprise of a trailer full of portable dental equipment which is hauled by a truck and parked at a fixed site to stimulate a dental operatory. Training resident dental surgeons and other categories of health workers in use of portable equipment will also pave way for further innovation in future.
Provision of healthcare to millions of people is a huge challenge for policy makers and health administrators, especially in developing countries that also are some of the most populous. Expensive imported technology can no longer be treated as a luxury of the privileged few. As aptly said in the Alma-Ata declaration [20], primary health care should be provided at a cost that the community and country can afford to maintain at every stage of their development in the spirit of self-determination!
*Year denotes Financial Year (April to March)
**Four (4) portable Dental units used for treatment in all the camps