Early identification of Autism Spectrum Disorders (ASDs) is vital as it facilitates the process of referral to specialist services and lead to early individualised intervention for children with these disorders [1]. Primary health care (PHC) providers such as General Practitioners (GPs) provide a gateway to specialist services [2]. In Australia, GPs are the primary paediatric providers and an average of 4.7 per 100 of their encounters are for providing immunization to children [3]. This places them at a unique position to screen children for early identification of ASDs. However, this could be a challenge due to structural barriers such as resources and reimbursement for extra time for consultation, diversity of clientele, diagnostic uncertainties for these disorders and a lack of consensus on the best screening strategy [4–8]. Professional organizations like the American Academy of Paediatrics (AAP) and Royal Australian College of General Practitioners (RACGP) emphasize the need to identify early signs of autism by primary care providers [9–11]. The two commonly suggested strategies include either the use of standardized developmental screening tools for well childcare visits or a red flag approach for five early signs of ASDs [10, 12]. The other challenges for GPs are the unclear reasons for the increasing prevalence of these disorders and the recent changes in the diagnostic categories of pervasive developmental disorders (PDDs) in Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)-V [5,13–17].
This rapidly changing and uncertain landscape of ASDs creates a dilemma for PHC providers. Qualitative research from Australia and North America points to hesitancy of GPs to refer early as a factor contributing to a delay in diagnosis of children with autistic disorders [18–20]. There is paucity of published literature on the importance of these disorders to GPs in Australia. Specifically the gaps in the literature include:
1. How often do GPs see children with autistic disorders and consider the diagnosis within their practices? (i.e., the relevance of autistic disorder to GPs)
2. What perceptions do GPs have about their ability (confidence and competence) to manage these disorders? What are their perceptions about the services, their beliefs in prescribing psychotropic medications and how aware are they of community resources in their region?
3. What knowledge (i.e. factual awareness of early signs, diagnostic features and management) of the condition do GPs have and what are their educational needs?
In order to explore the above research questions we conducted a survey of GPs in the state of New South Wales (NSW) in Australia. We felt challenged as to which terminology (PDDs, ASDs, Autism or Autistic disorder) to use in the survey. We preferred to use the term “Autistic Disorder” as it is known that GPs are more likely to consider the classical diagnostic concepts of autism, which correspond to the Autistic Disorder category of DSM-IV-TR [21].
Methods
The study was approved by the Northern Sydney Central Coast Area Health Service (NSCCAHS) Ethics Committee (Protocol Number, HREC-1102-076 M).
Sample Selection
There are several demographic variations for GPs in NSW based on the region and type of practice (e.g. solo versus larger practices, availability of practice nurses) and country of primary medical qualifications [22]. As a general rule of thumb, obtaining a representative sample from heterogeneous populations requires a minimum of 100 subjects for major groups (e.g. region of practice, gender) and 20 to 50 subjects for minor subgroups (e.g. such as GPs with specific areas of interest) [23]. Anticipating a response rate of 25-30 % from previous surveys done with GPs in NSW, 1185 questionnaires were posted. A simple random sample selection method from the health provider’s directory of the Northern Sydney District Health Network was used. This directory maintains the database of GPs across the state and was last updated in the year 2009-2010. Thus, the final sample frame consisted of 734 GPs from the urban/metropolitan regions, 237 from the regional areas and 214 from the rural/remote areas of NSW.
Design and Pre-Testing of the Questionnaire
The most commonly used instrument for evaluating knowledge of health professionals regarding ASDs was developed in 1987 [24]. It contained 22 Likert scale questions on beliefs regarding ASDs and 18 descriptors of behavior, intellect and symptomatology associated with these disorders. It was felt by the authors that this scale may not be sufficient for evaluating knowledge of primary care physicians due to rapid changes in the understanding of ASDs in the last two decades. Further factors unique to GPs such as the time constraints, diverse nature of practices cutting across disciplines of medicine and care provision across life span need to be considered. This suggested that questionnaires which capture not only the knowledge but also the relevance of these disorders to GPs may be more suitable. Factors such as the time constraints may be the reason why recent studies with GPs have used knowledge questionnaires using true/ false questions [25, 26]. For the purpose of understanding the broad research questions of the current study a brief questionnaire was developed (available on request from the author). The aim was to capture both qualitative and quantitative information with an emphasis on quantitative data.
Section A collected demographic information on age, years of practice, number of clinical sessions worked, country of primary medical qualification, region of practice and any areas of special interests.
Section B was designed to measure the “relevance”, “perceptions” of GPs as well as understand perceived educational needs and referral choices for children with autistic disorders. The items of the perceptions and relevance scale were scored on a linear scale to achieve a composite score (score range 1-10 and 2-12 for perceptions and relevance scales respectively). An example of how this was done is that question 1 of the relevance scale was scored from 0-4 and questions two and three from 1-4. This provided an opportunity to explore the potential relationship between knowledge, perceptions and relevance scores.
Section C contained 14 true/false type knowledge questions identified from the recent literature on ASDs. The questions were chosen to include domains of knowledge likely to be relevant to GPs. Refinement of the wordings of questions was done based on discussions during the pre-test phase. An “unsure/don’t know” response option was not given in the questionnaire to avoid skewing of the results towards negative [27]. A score of 11 out of 14 questions was taken as a cut-off criterion for knowledge scale. This was based on the T-scores where 75% was equivalent to 11 out of 14 questions. Similar cut-off has been used in an earlier study in Singapore [25]. We also confirmed the high cut-off point of 11 for the knowledge score using the k-means cluster analysis (k = 2) with the nearest centroid-sorting method [28, 29]. This derived two statistical group’s one forming the high cluster (i.e. those with the highest centroid value) and the other forming low cluster (i.e. those with the lowest centroid value).
Test-Retest Reliability and Clinical Usefulness
Pre-testing of the questionnaire was done on a purposive sample of 15 GPs. These GPs were requested to return the questionnaire twice within a period of two weeks. Out of them, 10 returned the questionnaire twice and seven achieved above cut-off score at both time points. Intra-class correlation coefficient for the paired GPs at two points was 0.59, which is fair [30]. Further no significant differences were evident in the mean total scores using paired t- test [Mean difference (MD) -0.1, Standard error of MD 0.45, p-value =0.8].
An “Ease Of Use (EOU)” questionnaire with Likert type responses was used to evaluate simplicity and usefulness of the questionnaire to GPs [31]. All GPs participating in the pretest phase found the questionnaire simple and easy to use so no major changes were made to the questionnaire.
Data Collection and Analysis
An information sheet, a personalised request letter, an anonymous questionnaire (coded to avoid duplication of GPs who had already participated in pretest phase) and a self-addressed reply paid envelope was posted in June 2011. An educational resource on ASDs was offered as an incentive for participation [32]. Reminders were sent within four weeks of the first posting. Administrative general practice divisions of NSW were contacted to further encourage participation.
Four hundred seven (34.3%) of surveys were returned out of which, 191 (16.1%) were completed while 216 (18.2%) unfilled questionnaires were returned mostly due to outdated addresses. This was not surprising as there is known inequality of provider continuity with GPs in Australia [33]. It was not possible to determine how non-respondents differed from respondents, because the lists comprising the sample frame did not contain descriptive data.
After data collection, internal consistency of the subscales of the questionnaire was checked using Cronbach alpha while the conceptual constructs of relevance, perceptions and knowledge scale were tested using Exploratory Factor Analysis (EFA).
Internal Consistency
The Cronbach alpha for knowledge and Relevance scale was 0.47 and 0.57 respectively. There was poor internal consistency among items of perceptions scale reflecting the highly subjective nature of this scale. Although the Cronbach alpha scores obtained were sub-optimal [30], similar Cronbach scores have been obtained in many other studies using true/false questions [34, 35].
Factor Analysis
Principal axis factoring with an oblique rotation method (Promax) was used [36]. The sample size was appropriate to run an EFA (Kaiser-Meyer-Olkin measure >0.5). Items which loaded into extracted factors with coefficients of more than 0.3 were generally considered except where clinical relevance was evident for variables loading with coefficients between 0.1-0.3. Factor analysis was done using IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY. In order to overcome the potential problems of factor analysis of binary responses of knowledge scale such as non-normal distribution of responses, an optimal implementation of parallel analysis was done using computer program “FACTOR” [37]. This program uses a polychoric correlation matrix suitable for binary variables and overcomes the problem of over-extraction of dimensions in EFA. The results were further verified using SPSS syntax for Parallel analysis [38].
Quantitative Analysis
We explored the association of baseline variables with knowledge score by treating it both as categorical variable (>11 vs. ≤11 correct responses) and continuous variable. For baseline variables continuous data was used whenever available except number of children with autism under care and new diagnosis of autism under care as data for these variables was only collected categorically. Baseline data of perceptions scale was coded for analysis as elaborated earlier.
Chi-square tests were used to explore the associations between knowledge scores as a binary variable and baseline categorical variables. Non-parametric methods were used to compare continuous dependent variable (knowledge scores as continuous variable) and baseline categorical variables. Univariate linear regression was used to examine the relationship between knowledge scores as continuous variable and baseline continuous variables. Pearson correlation coefficients were used to explore strength of relationship between significant baseline variables with knowledge score and between perceptions and relevance scores with knowledge score.
To analyse potential predictors for knowledge scores, variables (age, years in practice, new diagnosis of autism every year, self-perceived competence for ASD, awareness of community resources and perception of services) with p-value <0.25 in univariate analyses were included in a multivariate linear regression model. Due to the left skewed distribution of knowledge score, a power of two transformations was performed and distribution for transformed knowledge score was checked with normality plot of residuals.
Analyses were performed using SAS version 9.2 (SAS Institute. SAS: statistical software. 9.1 ed. Cary, North Carolina. SAS Institute, 2003).
Qualitative Analysis
Perspectives of GPs regarding their self-perceived educational needs, use of medications in children with autistic disorders and other comments made by them were explored using thematic analysis of the qualitative data. Coding of the qualitative data was done by reading sentences for recurring words and then by identifying patterns for themes [39]. Interpretations of qualitative findings were made to integrate results obtained from the quantitative data.
Results
A total of 191 (16.1%) completed questionnaires were analysed. Five GPs did not attempt any questions of the knowledge scale, while two attempted less than five questions (excluded from univariate and multivariate analysis). The proportions of GPs achieving correct answers to questions are shown in [Table/Fig-1]. Majority of GPs achieved satisfactory responses to these questions except failing to recognize the age of onset cut-off criteria in DSM-IV-TR. The baseline demographic characteristics of the participating GPs as compared to GPs in NSW and Australia are highlighted in [Table/Fig-2]. The sample obtained in the study was representative with regards to age and region of practice of GPs in NSW. However, more female GPs (not significant, p=0.06) and graduates from Australian medical schools (77%) responded [Table/Fig-2]. Twenty-five (13%) participants with primary medical qualification from a non-English speaking region responded [Indian subcontinent (13), Singapore (4), Hong Kong (1), South America (3), Middle eastern region (3), Eastern Europe (1)]. Similarly, more GPs with an interest in mental and/or child health responded (38% of respondents).
Proportion of GPs with correct responses to questions
| Question | N (%)a |
|---|
| Diagnosis can be made solely on parental report of child’s development/behaviour at home | 162(87.1) |
| DSM IV criterion includes abnormal functioning/delay in three areas with onset after 3 yearsb | 36(19.3) |
| Evidence based treatment is an early individualized education based program | 112(60.2) |
| MMR vaccine should be deferred in suspected Autistic disorders | 171(91.9) |
| Visual cues should be discouraged to improve verbal communication | 135(72.5) |
| Change in prevalence of Autistic disorder in school aged children compared to pre-schoolers | 140(75.3) |
| Prevalence of ASDs in preschoolers in Australia | 125(67.9) |
| Toddlers with autism often have suspected deafness and speech delay | 165 (89.6) |
| The diagnosis can be made in a language impaired child | 157 (84.4) |
| Boys should be explored for a possibility of Fragile X syndrome | 126 (68.4) |
| M-CHAT is a useful screening tool | 166 (92.4) |
| IQ status of children with ASDs | |
| Role of medications in children with ASDs | 176 (95.6) |
| Risk of ASDs in siblings is increased 20 to 40 fold | 137 (74.5) |
a186 GPs completed the knowledge scale, Missing response to questions on knowledge scale were taken as wrong bThe wording of DSM IV criteria was changed to “onset after 3 years” instead of “onset prior to age 3 years
Characteristics of respondents as compared to characteristics of GPs in NSW and Australia
| Characteristic | Survey respondents N (%)a | NSWb 2010-2011 N(%), p-value | Australiab 2010-2011 N(%), p-value |
|---|
| Number | 191 | 8654 | 27639 |
| Gender | 95(49.7) | 5134(59.3), 0.07 | 16357(59.9), 0.06 |
| Male | 96(50.3) | 3520(40.7) | 11282(40.1) |
| Female | | | |
| Age proportion | 48 (25.7) | 2543 (29.3), 0.7 | 9144(33), 0.4 |
| 30-46 | 62 (33.1) | 2520 (29.1), 0.6 | 8375(30.3), 0.7 |
| 47-55 | 77 (41.2) | 3591 (41.6), 0.97 | 10120(36.7), 0.5 |
| >55 | | | |
| Place of graduation Australia Overseas | 145 (77.1) 43 (22.9) | 5507(63.6), 0.001c* 3147(36.4), 0.09 | 17686(63.9), 0.001 c* 9953 (36.1), 0.1 |
| Place of practice Metropolitan Inner Regional Rural(Outer regional)/Remote | 125(65.8) 39(20.5) 26(13.7) | 6351(73.3), 0.07 1820(21.1), 0.9 483 (5.6), 0.2 | 18645(67.5), 0.7 5461 (19.7), 0.9 3533 (12.8), 0.9 |
a Some characteristics (variables) have less than 191 responses b GP Practice workforce statistics accessed from the Australian Government, Department of health and ageing website and includes GP registrars in training. The total number includes those GPs providing at least one claim for Medicare health service (public funded health insurance scheme for Australian citizens and residents),p- values are calculated in comparison to survey respondents c Statistically significant using Chi-square test for comparison of proportions
Univariate Analysis
Overall, 62% GPs achieved above cut-off score (≥11 correct answers) in the knowledge scale. More GPs with primary medical qualification from Australia achieved above cut-off score (64.4% vs. 48.8%, Chi-square test, p =0.04) [Table/Fig-3]. Other demographic characteristics were not different between GPs achieving above cut-off versus those achieving below cut-off.
Association between GPs characteristics with proportion achieving above cut-off scores
| Characteristica | <11 n=69 | ≥11 n=115 | Statistical test |
|---|
| Age yrs |
| Median | 56.5 | 52.0 | Kruskal Wallis, p-value=0.01* |
| Gender, n (%) |
| Female Male | 30 (33.7) | 59 (66.3) | χ2 test, p-value=0.28 |
| 40(42.1) | 55 (57.1) | |
| Years in practice |
| Median | 29.5 | 25.0 | Kruskal Wallis, p-value=0.01* |
| Country of primary qualification |
| Australia Others | 51 (35.6) | 92(64.4) | χ2 test, p-value=0.04* |
| 21 (51.2) | 20(48.8) | |
| Primary region of practice |
| Rural/remote Urban/metropolitan Regional | 9(34.6) | 17 (63.4) | χ2 test, p-value=0.66 |
| 49 (40.8) | 71(59.2) | |
| 15 (38.4) | 23 (62.6) | |
| Number clinical sessions |
| Median | 8.0 | 7.25 | Kruskal Wallis, p-value=0.93 |
| Specific field of Interest |
| None Mental health/Pediatrics Others | 23(34.8) | 43 (65.2) | χ2 test, p-value=0.30 |
| 21 (41.1) | 30 (58.9) | |
| 30(44.7) | 37 (55.3) | |
a Knowledge score available for 184 participants
There was a significant inverse relationship between age and years of practice with knowledge score using linear regression analysis [Table/Fig-4].This relationship was significant using Pearson coefficients as well (Pearson correlation coefficients -0.24, p-value<0.0001 and -0.25, p-value=0.001, respectively). There was a difference in knowledge score between GPs perceiving themselves to be competent in screening for autistic disorders (p=0.1, not significant) and those reporting awareness of community resources (p=0.005) [Table/Fig-5].
Relationship between characteristics of GPs and knowledge scores
| Characteristic | Na | Univariate analysis |
|---|
| Coefficient | 95% CI | p-value |
|---|
| Age | 191 | -1.04 | -1.60- -0.50 | <0.001* |
| Gender |
| Female | 95 | 5.44 | -5.07-15.95 | 0.31 |
| Male | 96 | 1 | | |
| Years in practice | | -1.16 | -1.72- - 0.60 | <0.001* |
| Country of primary qualification | | | | |
| Australia | 145 | 7.47 | -5.54-20.47 | 0.26 |
| Others | 43 | 1 | | |
| Primary region of practice |
| Rural/remote | 26 | 9.89 | -8.55-28.34 | 0.29 |
| Urban/metropolitan | 125 | 1.95 | -11.47-15.37 | 0.78 |
| Regional | 39 | 1 | | |
| Number clinical sessions | | 4.79 | -5.0-14.57 | 0.34 |
| Specific field of Interest |
| None | 70 | 3.97 | -8.62-16.56 | 0.54 |
| Mental health/Paediatrics | 52 | 0.54 | -12.39-13.47 | 0.94 |
| Others | 69 | 1 | | |
a Participants for whom knowledge score (available from 184) or information on characteristic was not available were considered missing data *significant
Relationship between relevance and perceptions items with knowledge score
| Relevance Items | Na | Univariate analysis |
|---|
| Coefficient | 95% CI | p-value |
|---|
| Autism under care |
| 1-2 | 76 | -8.43 | -22.80-5.94 | 0.25 |
| >2 - <5 | 67 | -2.86 | -17.27-11.55 | 0.70 |
| ≥5 | 34 | 1 | | |
| New Autism Diagnosis per year |
| <5 | 160 | -16.13 | -31.27- -0.99 | 0.04* |
| ≥5 | 22 | 1 | | |
| Number of children per week | | -0.02 | -0.32-0.28 | 0.89 |
| Perceptions items |
| Self-perceived as confident/competent |
| Developmental disorders in general |
| Confident and competent | 23 | 1 | | |
| Competent but not very confident | 75 | 4.49 | –11.95-20.92 | 0.59 |
| Not confident or competent | 79 | -6.84 | -23.28-9.59 | 0.41 |
| Screening for autistic disorders |
| Yes | 52 | 9.54 | -1.89-20.96 | 0.10 |
| No/somewhat | 123 | 1 | | |
| Awareness of community resources |
| Yes | 103 | 14.89 | 4.47 – 25.31 | 0.005* |
| No | 77 | 1 | | |
| Perception of services |
| Good/adequate | 60 | 9.10 | -8.04-26.24 | 0.30 |
| Inadequate | 106 | 17.80 | 1.89-33.71 | 0.03* |
| Unsure/left blank | 25 | 1 | | |
| Prescribe medications |
| With support of Specialist | 136 | 2.26 | –1.84-16.35 | 0.75 |
| On own initiative | 21 | -1.66 | -18.22-14.90 | 0.84 |
| Unsure/left blank | 34 | 1 | | |
a Participants for whom knowledge score(available from 184) or information on characteristic was not available were considered missing data
A weak but significant relationship existed between overall perception and relevance scores with knowledge scores [Pearson correlation coefficients 0.24 (p=0.001) and 0.15 (p=0.04) respectively].
Multivariate Regression Model
A multivariable regression analysis (variables with p<0.25 on univariate analysis were entered into this model) showed awareness of community resources as a significant factor affecting knowledge score (11.97, 95% CI 1.07-22.88, p=0.03).
Pattern of Medication use
Twenty one GPs (10.9%) reported using psychotropic medications on their own initiative. Out of these 11 reported prescribing risperidone and olanzapine along with other psychotropic medications (three also used mood stabilizers, two reported using clonidine, four used antidepressants and seven used stimulants). Ten reported prescribing Selective Serotonin Reuptake Inhibitors (SSRIs) antidepressants only.
Factor Analysis
A combined EFA of all the relevance, perceptions and knowledge items (true/false question) confirmed these to be separate constructs and a total of 10 factors were extracted accounting for 60% of the variance. Subsequently EFA was run for these three constructs separately.
For the knowledge scale six factors loaded 10 questions to account for 59% of the variance (eigen value >1.0). These factors were identified as the relevant sub-domains of knowledge for GPs and included “clinical suspicion”, “screening and referral”, “diagnostic criteria” “investigations”, “counselling” and “surveillance”. Factor covariance matrix showed strong correlation between the six factors (0.57-2.12). Parallel analysis using Factor program extracted four factors out of which three were group factors. Thus a final bi-factor solution emerged and included one factor which represented general questions on prevalence, risk factors, screening, investigation, counselling and referral and we called this dimension as “General Knowledge” regarding ASDs, while the other factor loaded questions on medications, change in the prevalence of ASDs in school going children compared to toddlers and IQ status of children with ASDs. This factor was called “Surveillance” [Table/Fig-6].
EFA and parallel analysis to understand the construct of knowledge scale as relevant to GPs
| Knowledge Scale | |
|---|
| Factor | Clinical constructa | Questions loadedb | Coefficientc | % variance explained |
|---|
| 1 | General Knowledge regarding autistic disorders (Prevalence, risk factors, Screening, Investigation, counselling and referral) | A diagnosis of Autistic Disorder can be made in a language impaired child. | 0.65 | 35.4 |
| Toddlers with Autistic Disorders often have suspected deafness and delayed speech development. | 0.48 |
| Modified Checklist for Autism in Toddlers (M-CHAT) is a useful screening tool | 0.44 |
| Boys with Autistic Disorder should be explored for a possibility of Fragile X syndrome | 0.83 |
| MMR vaccine should not be deferred in toddlers suspected to have Autistic Disorders | 0.45 |
| The evidence based treatment is an early individualized educational based program. | 0.37 |
| Prevalence of ASDs in preschoolers | 0.25 |
| Risk of ASDs in siblings | 0.25 |
| Use of visual cues should be encouraged in ASDs | 0.23 |
| 2 | Surveillanced | Intellectual disability (IQ)status in children with Autistic Disorders | 0.72 | 19.8 |
| The role of medications in managing challenging behaviours in children with Autistic Disorders | 0.93 |
| Change in prevalence of Autistic Disorders in school aged children versus preschoolers | 0.61 |
a Initial EFA extracted six factors but parallel analysis smoothed the results and highlighted two main sub-domains of knowledge regarding autistic disorder as theoretically most relevant to GPs, b Questions presented in this Table are slightly modified statements of the questions asked in the original survey, c Only questions loading into factors with coefficients >0.2 were selected for this scale, Q 3 and Q5 were rogue items, d Items on this dimension need further development
For the perceptions scale four factors with Eigen value >1.0 were loaded and explained more than 62 % variance. Out of four, three were group factors. These factors loaded items of confidence of GPs for autistic disorders into one, GPs belief in prescribing medications and their awareness of community resources into second [Table/Fig-7]. Correlation was evident for these factors (0.3-1.8). Parallel analysis confirmed this scale to be a single construct.
Exploratory factor analysis (EFA) to understand the constructs of relevance and perceptions scale
| Relevance scale | |
|---|
| Factor | Clinical construct | Items loaded | Coefficienta | %variance explained |
|---|
| 1 | Relevance of autistic disorders to GPs | Autism in care | 0.64 | 47 |
| New diagnosis made/year | 0.65 |
| Perceptions scale |
| 1 | Self-Perceived Confidence | Confidence/competence screening autistic disorder | 0.59 | 24.4 |
| Confidence/competence diagnosis autistic disorder | 0.57 |
| Confidence managing behaviour associated with autistic disorder | 0.61 |
| 2 | Self-Belief in prescribing medications, community resources | Prescribe medications in autistic disorders | 0.78 | 37.8 |
| Prescribe on recommendation of specialist | 0.61 |
| Awareness of services | 0.61 |
a Questions loading onto factors with coefficients >0.3 were selected, Factor covariance matrix showed correlation of factors of perceptions scale, Parallel analysis confirmed perceptions scale to be a single construct
For the relevance scale one factor was extracted on which two items (autism under care and new autism diagnosis/year loaded and accounted for almost 50% of variation with Eigen value of 1.4 [Table/Fig-7].
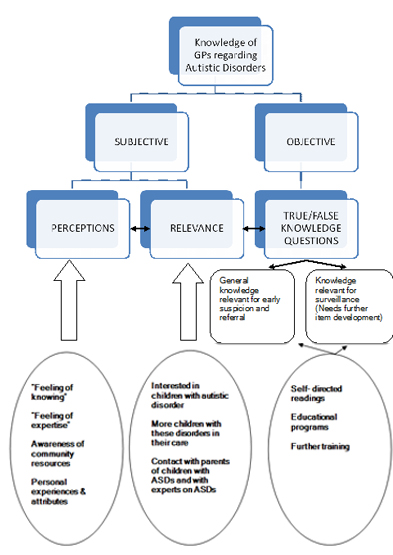
Emerging Model of Knowledge Construct
EFA revealed knowledge scale as bi-dimensional and the potential influences of perceptions and relevance items on this. Qualitative analysis of comments made by GPs supported this model. A wide range of sources were reported as a source of knowledge for these disorders. Some stated gaining knowledge from their personal experiences from interactions with parents and specialist diagnostic teams (allied health professionals, paediatricians, psychiatrists) while others cited children in their extended family members to be a source of knowledge. Some reported self-directed readings of articles pertaining to ASDs in primary care while others cited attendance at paediatric specific educational programs such as Diploma in Child Health as main sources of information. Some GPs also reported websites of local community resources and schools and programs providing early interventions for children with ASDs as a valuable source of knowledge. A model to understand the knowledge and educational needs of GPs regarding autistic disorders emerged from qualitative and quantitative data and is highlighted in [Table/Fig-8].
Emerging model to understand the nature of knowledge of GPs for autistic disorders
Educational Needs
The main themes identified for education from qualitative data are highlighted in the following quotes of GPs:
Screening/Diagnosis
“Clues to alert to the diagnosis, co-morbidities, ongoing management issues, interactive workshops using case studies”
“(features of) Asperger’s syndrome, less severe ends of spectrum, diagnosis what to look for.....”
Referral Pathways/Services/Resources
“Need to know at a very basic level, recognition and referral pathways locally”
Psychopharmacology Knowledge/Competence
“Don’t have good understanding of medications used in children with these disorders...”
“I am concerned when to cease, interactions, inappropriate use, school management, continued substance abuse, adequate adult person supervision, and cluster usage groups”
Uncertainty in diagnosis and evidence (aetiology, medications)
“Like other community health professionals wonder whether it is a behavioural problem or a biochemical one, single parents seem overrepresented amongst the few patients I have had exposure to”
“I feel there is a huge discrepancy amongst paediatricians and psychiatrists in what they will prescribe”
Role of GPs
Some GPs lamented their only role for passive utilisation for completing forms for the families. This is highlighted in the following quote by a GP practicing for 19 years in a regional area of NSW.
“Children tend to be picked up in play groups, see community/developmental paediatricians, then circulate through range of resources......Many patients actually bypass the GP and come back to us to complete forms”
Perceptions Regarding Health System Factors
Some GPs from rural areas commented on the lack of adequate services in their regions. Inadequate services were also cited for school aged children and adolescents with ASDs. Many GPs reported waiting times to access diagnostic and early intervention services to be a major issue. This was often reported by parents to their GPs.
Only few GPs reported early childhood centres and nurses as important resources for families and health professionals. Some GPs reported lack of clarity of pathways to access new funding programs rolled out for children with disabilities and ASDs by the federal government.
Discussion
We evaluated the relevance, perceptions, knowledge and educational needs of 2.2% of GPs in the state of NSW using a pre-tested questionnaire. The complex multidimensional nature of knowledge of ASDs and the likely influence of perceptions and relevant items was noted from the qualitative comments made by GPs of their interactions with parents and extended family members with children with ASDs as a source of knowledge. These interactions are a tacit source of knowledge acquisition and are often influenced by personal beliefs of families and practitioners. The subjective knowledge acquired from such sources is often difficult to separate from objective knowledge [40].
A theoretical model of knowledge of ASDs for GPs emerged from the data and involved both subjective and objective sources [Table/Fig-8]. This model gains support from an insightful ethnographic study with GPs in the UK, where “knowledge in practice” was shown as a social construct and knowledge acquisition by GPs was informed by their own and colleague’s experiences, their interactions with opinion leaders and patients and other tacit sources of knowledge [41].
This emerging model adds to the existing body of literature on knowledge of primary care practitioners regarding ASDs, which has mostly focused on objective knowledge testing often not taking into account GPs own beliefs, relevance and interest in these disorders [20, 25, 42]. The study thus enhances our understanding of knowledge of GPs using the known selectors of knowledge viz. subjective, inter-subjective and objective domains [40]. This model is similar to the nature of knowledge in other disciplines such as social work [43] and helps in reinforcing the importance of considering context bound information such as practitioners with interest and greater awareness of these disorders in service delivery of children with ASDs [44].
Currently increasing awareness of these disorders and establishing clear pathways for management is the envisioned strategy for service delivery of children with ASDs [45, 46]. The study reinforced that this is appropriate and is likely to be associated with greater knowledge of GPs. In addition the study also emphasises two primary target areas for education of GPs. These include the “general knowledge” dimension relevant for early suspicion and referral and a “surveillance” dimension is important for expanding the role of GPs. This dimension needs to developed further to include items for surveillance for co-morbid medical conditions(such as sleeping difficulties, anxiety, depression), ongoing support to families in managing schooling options, monitoring of changing abilities, medications and ongoing management of challenging emotional and behavioural disturbance associated with ASDs. This model also suggests need for future research for developing specific educational models for ASDs acknowledging previous experiences of practitioners [47].
Although, the relevance of autistic disorders to responding GPs was evident in the present study, variability was demonstrated amongst their knowledge of these disorders. GPs with an interest and knowledge of ASDs responded more. These findings are consistent with studies done in the UK [48] and Canada [49], where an increased “interest and concern” of practitioner accounted for a large proportion of variance in their ability to identify psychiatric illness. Similarly more response from female GPs in the present study is consistent with their ability to be better at delivering preventative activities [50, 51]. Due to small number of responses from practitioners of culturally diverse backgrounds and with primary medical qualifications from developing countries it is difficult to make conclusions on the impact of this factor on knowledge. This is important to research in future studies as there are known gaps in the knowledge of health staff from developing countries in the field of developmental milestones due to more focus on topical diseases of interest [25, 52, 53]. Pham et al., has shown Canadian and local medical graduates to deliver better preventative health care to Medicaid beneficiaries in North America [54]. However, contrary findings have been shown in a survey of GPs in Victoria (Australia) where practitioners receiving basic medical qualifications outside Australia reported more involvement in child public health issues [51]. Rahbar et al., have highlighted in a survey of 348 GPs from Pakistan that only 44.6% had even heard of autism [42].
Lian et al., in a survey of 48 GPs from Singapore has shown their knowledge of autism as less than ideal and some myths to be believed as true [25]. In their study only about one-third achieved cut-off criteria for knowledge items, this is significantly less than 62 % in the present study using the same criteria. In the present study about 8% of GPs reported that Measles, Mumps, Rubella (MMR) vaccine should be withheld in children suspected with ASDs. Although, there were no differences in the knowledge scores for this small subgroup of GPs, this is somewhat concerning as epidemiological studies have not shown such an association [55]. Falagas in a systematic review of literature highlighted conflicting information provided by health professionals as a factor for suboptimal compliance to vaccinations in children in developed countries [56].
In present survey some GPs reported that the diagnosis of autistic disorders could be established by parental report alone. This highlights a gap in their knowledge as maladaptive behaviours associated with these disorders are often pervasive in nature and occur across settings. Thus, educational programs for GPs should stress the need to gather information from other sources such as pre-schools, extended family members and playgroups to validate carers concerns.
Education regarding knowledge of screening tools and early signs of these disorders was perceived as a priority by GPs in present survey. Some GPs (5%) reported using screening tools for autistic disorders within their practices. This finding is similar to 8% screening reported for ASDs in a survey of 255 primary general pediatric providers in Delaware and Milwaukee, North America [8]. The main reasons reported for sub-optimal screening in this study were lack of familiarity with tools, referral made to the specialist or inability to devote enough time for screening. A point that is unclear from this study is the basis on which the primary pediatric providers provided referral to the specialist. It would have been useful to know whether screening for early signs and red flags of these disorders were used to screen children for autism. This is currently considered to be the best screening approach for ASDs in primary care. Chawarska et al., have identified children failing to adopt anticipatory postures such as reaching out to be picked up, less visual attention to social stimuli, smiling in response to others, vocalization and object exploration as early signs of autism [57]. Fillipek and colleagues [10] have identified five red flags mandating immediate referral for further investigations (a) Does not babble or coo by 12 months of age, (b) Does not gesture (point, wave, grasp, etc.) by 12 months of age (c) Does not say single words by 16 months of age (d) Does not say two-word phrases on his or her own (rather than just repeating what someone says to him or her by 24 months of age and (e) Has any loss of any language or social skill at any age.
In NSW routine developmental surveillance is recommended using Parents Evaluation of Developmental Screening (PEDS) tool, which is present in the personal health record of children (commonly referred to as “Blue Book”). This is a broad parent based screening tool and can help in the early identification of ASDs. In a study of 427 children between 18 and 59 months performance patterns on PEDS have been shown to reduce over-referrals for further screening using autism specific tool [58]. In NSW training for PEDS is currently limited to child and family health nurses due to lack of consensus among educators and administrative reasons. This is not an optimal situation as only about a quarter of children more than one year are regularly seen by early childhood nurses in NSW (NSW Ministry of Health 2012). Thus, educational programs for GPs should include training in primary developmental screening tools. Also the utility and effectiveness of autism specific screening tools such as Modified Checklist for Autism in Toddlers (M-CHAT) and Social Communication Questionnaire (SCQ) in primary care settings has to be emphasised [59]. Due to large diverse backgrounds of GPs, cultural beliefs of health professionals for developmental screening need to be recognized and explored further [60–62].Collaborative models of care for supporting delivery of preventative activities using screening tools by primary providers also need further exploration [63].
The other identified issue for education was regarding evidence for early intervention models. In present study uncertainty was reflected in the views of GPs regarding efficacy of early intervention. This is critical as current evidence suggests an early-individualized intervention program as the best practice for management of these children [1, 64, 65]. In a systematic review of controlled studies, Lovaas-based approaches, early intensive behavioral intervention variants and the Early Start Denver Model (ESDM) have been shown to improve cognitive performance, language skills, and adaptive behavior skills in young children with ASDs [1]. A recent uncontrolled study has also demonstrated community dissemination of the ESDM using a group-based intervention as effective [66].
The other perceived area of education was psychotropic prescribing for children with autistic disorders particularly evidence base regarding indications and the best practice for surveillance. Most GPs expressed concerns about the overuse of psychotropic medications in children in the present study. This is a valid concern as population based studies have shown inappropriate use of psychotropic medications [67,68]. Fremont and colleagues have highlighted prescribing behaviours of family physicians and pediatricians for psychotropic medications in children [69]. Pediatricians were reported to be more comfortable in prescribing stimulants, atomoxetine and alpha-2 adrenergic agonists while family physicians were more comfortable prescribing antidepressant medications. Similar prescribing pattern is reported by GPs in the present study. The role of psychopharmacology in children with ASDs is well documented now. A number of studies have shown that psychotropic medications in ASDs are often used to target co-morbid symptoms and maladaptive behaviors such as aggression, self-injury, repetitive mannerisms (e.g., perseveration, obsessions, compulsions, and stereotypic movements), mood lability, irritability, anxiety, hyperactivity, inattention, destructive and disruptive patterns [70–74]. In an internet based national database of 5181 children (sample consisting of 49% older children 6-11 years, 83% male and 39% with one or more co-morbidity), 35.3% used at least one psychotropic medication [75].
Age of GPs and years of practice were noted to have an inverse relationship with knowledge regarding ASDs. There are three likely explanations for this observation. Firstly, there is an increasing recognition and prevalence of these disorders in the last two decades [13]. Secondly, there is an increased focus on learning disabilities and developmental problems in undergraduate medical curriculum [76]. Thirdly, it is known from studies in North America and Netherlands that factual knowledge not used after five to ten years of certification becomes redundant for daily practice [77, 78].
Awareness of community resources and greater knowledge of ASDs was positively associated with self-perceived competence in developmental disorders. This is supported by studies where self-confidence has been shown to be a related construct with learning abilities of an individual [79].
Limitations/Strengths of the Study
The response rate of present survey is low. This is not unusual for surveys done with GPs and family physicians worldwide. An earlier study done in Australia have highlighted time constraints, increased paper work load, multiple surveys, low priority for an individual GPs practice and lack of reimbursement as main reasons for low response rates [80].
The representativeness and generalisability of findings are limited and results from present study should be interpreted with caution. Although some of the baseline characteristics of GPs in our sample look deviant [Table/Fig-2], rural and regional practitioners from different age groups were represented. We did not use weighting methodologies to overcome the problem of non-response bias in our study as only a weak relationship has been shown to exist between non-response rate and non-response bias [81]. Also as no information was available on the characteristics of non-respondents who received the survey versus those who didn’t (due to outdated addresses) meant that weighting was an inappropriate strategy.
True/false questions were used in the study, which have a lower sensitivity and specificity (due to 50% chance of guessing) compared to clinical vignettes, and multiple choice questions for knowledge assessment [82–84]. This was also evident in the present study from explicit comments made by GPs on the questionnaires acknowledging that they guessed some of the responses rather than being certain of the correct answer [79]. However, this is a frequent strategy used in a number of previous studies with GPs where time constraints are an important issue [25, 34, 77, 85].
Strength of our study is that we highlighted the educational needs of GPs using objective knowledge testing and used qualitative data to explain findings. This gave insights into GPs understanding and experiences with children of these disorders.
We performed an EFA to understand the validity of brief true/false knowledge questionnaires to GPs. A bi-dimensional construct of knowledge and the likely influences of items of perceptions scales reflected the complexity of these constructs, necessitating further refinement using confirmatory factor analysis. The items of the “surveillance” dimension of knowledge scale need further development and testing. Also convergent validity of knowledge scale using true/false questions with Stone’s autism survey scale [24] need to be established.
Some of the factors such as the potential impact of the type of practice setting on relevance and knowledge were not explored in the current study. The average age at which GPs considered diagnosis of ASDs within their practices was also not specifically explored.
Conclusions and Implications for Further Research
A significant proportion of GPs consider a diagnosis of autistic disorder within their diverse clinical practices in NSW. Variability in knowledge regarding autistic disorders is affected by a complex set of factors. Age, an increased interest in ASDs, country of qualification, awareness of community resources, and self-perceived confidence in these disorders appear to be relevant. Awareness of community resources emerged as an independent factor influencing knowledge in the present study. There is a need for education in the dimensions of general knowledge focused on early identification and referral (early signs and utilisation of screening tools for autistic disorders, emphasis on importance of early intervention) and further expansion of role in ongoing surveillance activities such as psychopharmacology and outcomes. This is important as current evidence shows that delay in identification and early intervention of children with ASDs lead to poorer outcomes later in life such as placement in special education settings, residence in group home settings, poorer mental health outcomes, employment status and other related co-morbidities such as epilepsy and mortality. Further validation studies using larger sample sizes are needed to test the knowledge model highlighted in the study.
A lack of published literature on child health surveillance at primary care in Australia was noted. A larger multi-site, multi-partners “Watch Me Grow” study is currently underway in NSW. This study has both qualitative and quantitative arms and is exploring perspectives of primary care providers such as GPs, child and family health nurses, practice nurses and users (parents) regarding surveillance for developmental disorders in different contexts. A large cohort of children from newborns to 18 months is prospectively enrolled in this study to understand factors affecting developmental surveillance. Future research should also explore data from national and state surveys and Medicare claims for items specific to child health surveillance and ASDs. In depth case studies of different setting general practices for factors affecting delivery of child health surveillance activities will increase our theoretical understanding for service delivery for children with autistic disorders in primary care.
a186 GPs completed the knowledge scale, Missing response to questions on knowledge scale were taken as wrong bThe wording of DSM IV criteria was changed to “onset after 3 years” instead of “onset prior to age 3 years
a Some characteristics (variables) have less than 191 responses b GP Practice workforce statistics accessed from the Australian Government, Department of health and ageing website and includes GP registrars in training. The total number includes those GPs providing at least one claim for Medicare health service (public funded health insurance scheme for Australian citizens and residents),p- values are calculated in comparison to survey respondents c Statistically significant using Chi-square test for comparison of proportions