Since its first recognition in 1981, Human Immunodeficiency virus (HIV) infection has emerged as a global pandemic. The disease has a potential to cause serious derangement of the immune mechanism of the host, thus, leading to severe opportunistic infections and unusual malignancies affecting all major organ systems including lungs. About 33.3 million people worldwide are suffering from HIV infection and associated complications [1]. An estimated 2.27 million people in India are living with HIV infection [2].
Pulmonary infections, remain a leading cause of morbidity and mortality and one of the most frequent causes of hospital admission in HIV infected people worldwide. An incidence of 20–25 episodes per 100 hospital admissions per year has been observed [3]. The HIV-associated pulmonary conditions include both opportunistic infections and neoplasms. Majority of the pulmonary complications of HIV positive patients are infectious in origin including various bacterial, viral, fungal and protozoal infections [4,5]. These infections depend mainly on the CD4 count of the individual, different disease spectrum is seen at different range of CD4 count. Apart from these opportunistic infections, non-infectious conditions like Kaposi’s sarcoma, malignancies of lymphatic system like non-Hodgkin’s lymphoma are also prevalent. Lymphocytic interstitial pneumonia and non-specific interstitial pneumonia are also seen sometimes [4,5].
Todo et al., in 1982, initially described technique of High Resolution Computed Tomography (HRCT) for diffuse lung disease and described the potential benefits of the technique in assessment of various lung diseases [6]. HRCT brought revolution in pulmonary imaging where resolution reached the secondary pulmonary lobule or the functional unit of lung. HRCT allows delineation of the lung parenchyma down to the level of secondary pulmonary lobule. High-resolution computed tomography (HRCT) is both very sensitive and accurate, with an overall diagnostic accuracy of 92% [7]. Due to these features, HRCT has become an important diagnostic tool in pulmonary medicine and provides valuable information about various focal and diffuse lung diseases [8]. HRCT may be useful in the evaluation of patients with suspected pulmonary disease when the initial diagnostic workup fails to ascertain the diagnosis and when there is no agreement between clinical and radiological data [9].
To determine the High Resolution Computed Tomography spectrum of lung parenchymal and interstitial imaging findings in HIV infected patients presented with chest symptoms on the following features:
Materials and Methods
This study was conducted in a tertiary health care centre, New Delhi, India. The study consisted of 45 patients. The cases were selected from indoor and outdoor admissions based on the following criteria:
Inclusion Criteria
HIV positive adult (>18 years) patients of both sexes who have presented with a lung disease on the basis of clinical profile and plain radiography.
Exclusion Criteria
Immunocompromised patients who have suspected lung disease but are HIV negative.
Pregnant HIV positive patients.
The primary clinical features were weight loss, fever, cough (both productive and non-productive) and dyspnoea.
Methods
A thorough clinical history of all the HIV positive patients presenting with suspicion of pulmonary disease was taken. Duration of symptoms was also recorded. General physical and respiratory system examination of all patients was done. Then a meticulous record of all the available laboratory investigations including HIV status, CD4 counts, routine blood examination, sputum examinations, pleural fluid analysis, FNAC, and other available investigations was kept. Chest x-rays of the patients were studied for the presence of any abnormality.
HRCT scans of the chest were done in all the cases taken in the study.
Patient Preparation
The procedure and objectives of performing the high resolution CT scan was explained to the patient and written consent of the patient was taken. Prior fasting was not advocated as the procedure did not warrant the need for contrast injection. The patient was explained and demonstrated the procedure of breath holding during the acquisition of HRCT scans.
Hrct Protocol
Patient Position
The patient was kept supine on the gantry table and was scanned cephalocaudal in the axial axis. Scans obtained with patients supine were adequate in most instances. Prone scans were taken when needed. The scanogram or topogram was first taken and then the whole lung was scanned from apex to the base. The scans were performed on Siemens Somatom Emotion 16 Slice Multidetector scanner using the following protocol.
Collimation = 1 mm
Feed = 10mm
Scan time =1 sec
KVp = 120 – 140
mA = 240
Matrix size = 512 x 512
Windows- window mean/ width values = -600 to -700/ 1000 to 1500
Reconstruction Algorithm
High spatial frequency algorithm was used. It reduces image smoothening and increases spatial resolution, making structures appear sharper. Thus, small vessels and bronchi are better seen in HRCT.
Results
Maximum number of patients was in age group 31-40 years (24 cases). Out of 45 patients included in our study, 32 (71%) were male and 13 (29%) were female. Male to female ratio was 2.4: 1.
Spectrum of Pulmonary Diseases Noted in Our Study
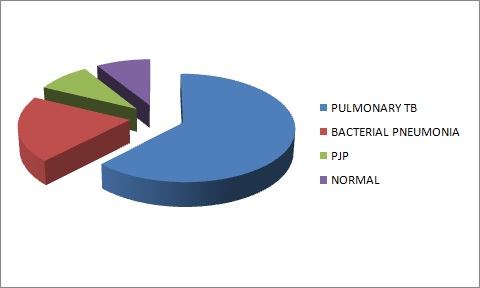
In our series of 45 patients, 62.2% of patients were diagnosed as having pulmonary tuberculosis, followed by bacterial infection in 20% cases and Pneumocystis jiroveci pneumonia (PJP) in 8.9% patients, while 8.9% of the study did not reveal any significant abnormality [Table/Fig-1]. These diagnosis were made considering the imaging findings along with clinical complaints of the patients and laboratory investigation findings.
1. Pulmonary Tuberculosis: A total of 28 patients in our study were diagnosed to be suffering from pulmonary tuberculosis. The CD4 count in these patients varied from 21 to 395 cells/mm3 with a mean count of 189 cells/mm3. Fifteen patients had CD4 counts less than 200 cells/ mm3. Different HRCT pattern and their frequency, obtained in given study, in tabulated in [Table/Fig-2].
HRCT Patterns and their frequency in Pulmonary Tuberculosis cases
| HRCT Findings | No. of Patients | Percentage |
|---|
| Scans with Single finding | 07 | 25 |
| Nodules | 06 | 21.4 |
| Lymphadenopathy | 01 | 3.5 |
| Scans with two findings: | 07 | 25 |
| Consolidation with nodules | 02 | 7.1 |
| Consolidation with cavitation | 01 | 3.5 |
| Consolidation with pleural effusion | 03 | 10.7 |
| Nodules with pleural effusion | 01 | 3.5 |
| Scans with three findings | 10 | 35.7 |
| Consolidation +nodules +lymphadenopathy | 01 | 3.5 |
| Consolidation + nodules+ pleural effusion | 02 | 7.1 |
| Consolidation+cavitation+nodules | 01 | 3.5 |
| Consolidation+Nodules +GGO | 01 | 3.5 |
| Nodules + lymphadenopathy | 01 | 3.5 |
| Nodules+ lymphadenopathy+pleural effusion | 03 | 10.7 |
| Nodules+ GGO+ pleural effusion | 01 | 3.5 |
| Scans with four findings | 04 | 14.2 |
| Nodules+consolidation+cavitation+lymphadenopathy | 01 | 3.5 |
| Nodules+cavitation+ GGO+ lymphadenopathy | 03 | 10.7 |
Maximum number (22/28) of patients with pulmonary tuberculosis were indentified to have nodular opacities. The size of the nodules in all the cases was <1 cm with majority of them being 1-5 mm in size; more than 5 nodules were noted in 20 cases (90.9%) and no nodules were found in six cases. The nodules were ill defined in 14(86.3%) patients. Well defined nodules are noted in two patients only. Well defined nodules as well ill defined with cavitation and well defined nodules and ill defined without cavitation was noted in three patients each. Centrilobular pattern of distribution was noted in 68.1% of cases and it was associated with tree in bud opacity in 54.5% of cases [Table/Fig-3]. Miliary pattern was noted 21.4% of the cases [Table/Fig-4].
Scan showing areas of consolidation with cavitation within (arrows). Multiple centrilobular nodules showing clustering and tree-in-bud pattern (thick arrow). Case of pulmonary tuberculosis

Nodules distribution in TB cases
| Distribution of Nodules | No. of Patients |
|---|
| Centrilobular | 03 |
| Centilobular + Tree in bud | 08 |
| Clustered +Centilobular +tree in bud | 04 |
| Random | 06 |
| Clusters | 01 |
Consolidation was lobar in nine patients and diffusely distributed patches were noted in one patient only while patchy along with lobar consolidation were noted in two patients.
Cavitation was thick walled in four patients and thin walled in 2 patients. The location of these cavities was in right upper lobe in 4 cases, while in left upper lobe in two cases. All the patients having cavitation had CD4 count >200 cells/mm3.
Lymphadenopathy was noted in the hilar region in three patients, mediastinal in five while three patients had both hilar and mediastinal lymphadenopathy. Subsequent contrast enhanced scans were done in three cases. Lymph nodes showed peripheral rim enhancement with low attenuation centre suggestive of caseating necrosis due to tubercular infection.
Eight patients had unilateral and two had bilateral pleural effusion. Among the patients with unilateral pleural effusion 5 had right-sided and 3 had left sided pleural effusion.
Bronchiectasis was noted in 12 out of 28 patients with pulmonary tuberculosis. It was accompanied by bronchial wall thickening in 8 cases.
Fibrotic opacities were noted in eight cases suggestive of old healed infective process in addition to the active pathology.
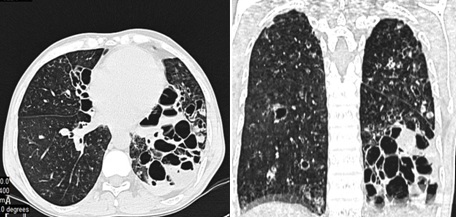
2. Bacterial Infection: [Table/Fig-5]: A total of nine patients in our study were diagnosed to be suffering from bacterial infection. The CD4 count in these patients varied from 121 to 366 cells/mm3, with a mean count of 195 cells/mm3. The most common HRCT finding in bacterial infection was lobar consolidation [Table/Fig-6]. Bronchiectasis of predominantly cystic in nature was noted in left lower lobe and was associated with air fluid level suggestive of secondary infection in one case of our study [Table/Fig-7].
HIV-positive patient with bacterial pneumonia. Axial HRCT (a) lung window (b) mediastinal window. Area of consolidation seen involving posterior segment of right upper lobe with adjacent areas of ground glass opacity

HRCT patterns and their frequency in bacterial infection
| HRCT Findings | No. of Patients | Percentage |
|---|
| Lobar Consolidation | 06 | 66.6% |
| Nodular Opacity | 02 | 22.2% |
| Bronchiectasis | 01 | 11.1% |
Axial HRCT image (a) and coronal reformatted (b) images show cystic bronchiectasis with air fluid level in left lower lobe. Areas of bronchiectasis are also seen in both the upper lobes. Diagnosis: Bronchiectasis with secondary bacterial infection
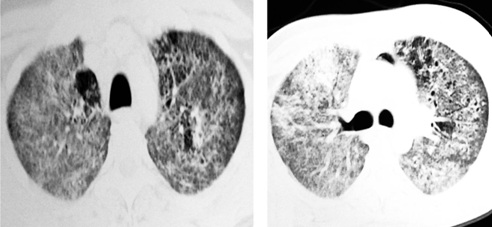
3. Pneumocystis jiroveci Pneumonia (PJP): A total of four patients in our study were diagnosed to be suffering from Pneumocystis jiroveci pneumonia. The most common HRCT finding was diffuse ground glass opacities in mosaic pattern of distribution. Few tiny cystic lesions were also noted in one case in bilateral upper lobes [Table/Fig-8]. All of these patients were in severe immunocompromised stage with CD 4 counts < 200 cells/mm3, ranging from 24-47 cells/mm3 with a mean count of 34 cells/mm3. The nodules were randomly distributed, measured 1-5mm in size, >5 nodules were noted.
HRCT Patterns and their frequency in Pneumocystis jiroveci Pneumonia
| HRCT Findings | No. of Patients | Percentage |
|---|
| Diffuse Ground Glass Opacity | 01 | 25% |
| Consolidation and GGO | 01 | 25% |
| Crazy paving and GGO | 02 | 50% |
Discussion
Respiratory illnesses are one of the major causes of morbidity and mortality in HIV-positive patients. A total of 45 HIV positive patients were studied, who presented with chest symptoms like cough, dyspnoea with/ without positive findings on chest radiograph.
The disease activity, pattern, degree of involvement and associated complications were better evaluated with the help of HRCT examination.
The total number of people living with HIV/AIDS (PLHIV) in India is estimated at around 20.9 lakh in 2011. Among which 86% are in the age group of 15-49 years. Of all HIV infections, 39% (8.16 lakh) are among women [10]. The adult HIV prevalence (males and females together) in India, in 2009 is estimated as 0.31% with uncertainty bounds 0.25–0.39%. Genderwise, HIV prevalence was estimated at 0.25% for women and 0.36% for men [11]. This section of the population is more affected because they are sexually more active and the social structure is patriarchal. Females do not seek medical care fearing ostracism and loss of family support.
Spectrum of pulmonary diseases
I. Pulmonary Tuberculosis
A total of 28 patients in our study were diagnosed to be suffering from pulmonary tuberculosis and was the most common disease noted in our study accounting for 62.2% of the cases.
The World Health Organization (WHO) reported that among the 9.27 million incident cases of tuberculosis, an estimated 14.8% occurred in HIV-positive patients, with 456,000 deaths from tuberculosis among HIV-infected patients [12]. The African region accounted for most HIV-positive tuberculosis cases (79%), followed by the Southeast Asia region (mainly India), which had 11% of total.
According to NACO annual report 2012-2013 “fatality rate among HIV infected TB cases remain 13-14% against less than 4% in HIV negative TB cases” [12].
Computer Tomography (CT) is considered the gold standard for assessing the morphological changes of lung parenchyma [13].
In our study 78.5% patients demonstrated presence of nodular opacities followed by Consolidation (46.4%), Lymphadenopathy (35.7%), Pleural effusion (35.7), Ground Glass Opacity and Cavitation (21.4% each) [Table/Fig-2].
Hatipoglu et al., observed that centrilobular nodular or linear structures (91%), “tree-in-bud” appearance (71%) and macronodules (69%) were the most common HRCT findings seen in active pulmonary tuberculosis [14] [Table/Fig-9].
Multiple nodules are seen in the visualized lung fields. Most of the nodules are evenly spaced and not touching the pleural surface. Few areas show clustering of nodules. Centrilobular nodules in a case of pulmonary tuberculosis

Feng et al., showed that weight loss, miliary nodules, necrotic lymph, lobar consolidation, and tree-in-bud sign were independent predictors for AIDS-related PTB [15].
In their article on images of lung manifestations of HIV/AIDS, authors have described that features of reactivation MTB are patchy consolidation, including involvement at unusual sites, e.g. lower lobes, cavitation, nodularity, effusions and adenopathy. TB lymph nodes are typically markedly enlarged and of low attenuation on CT, often demonstrating rim enhancement following contrast administration. Primary MTB manifests as focal unilateral, often lower lobe consolidation and adenopathy. Cavitation is less common at lower CD4 counts. Patients in this range also have an increased incidence of miliary MTB, with diffuse, randomly distributed nodules on CT [7].
In the study by Naseem et al., HRCT findings included centrilobular nodules in 92% cases, lobular consolidation in 84%, cavitation in 76%, and ‘tree-in-bud’ appearance in 68%, lymphadenopathy in 8% and military nodules in 4% cases [16].
Hilar and mediastinal lymph node enlargement is commonly seen on HRCT in patients who have active tuberculosis. Mediastinal lymphadenopathy is more commonly seen in HIV-positive patients as compared to HIV-negative patients who present more commonly with lung parenchymal opacities and cavitations [17]. In the study by Feng et al., the presence of lymphadenopathy was a significant finding in which lymphadenopathy could be observed in 44 (77.2%) of 57 patients with TB [15]. Pleural effusion is a common complication in pulmonary tuberculosis. Effusion is mostly exudative in nature. Unilateral effusion is more common than bilateral.
In study of 3263 patients with definite or suspicious TB, Taiwan, 24.27% had tuberculosis pleurisy [18].
Bronchiectasis
Bronchiectasis is generally defined as localized, irreversible bronchial dilatation, often with thickening of the bronchial wall. A bronchus is considered to be dilated if the broncho-arterial ratio exceeds 1.
In a 17 year study conducted in Shanghai, China, Pulmonary Tuberculosis was found to be main cause of bronchiectasis (13.17%) [19].
Our findings fairly correlate with the findings of the various studies.
II. Bacterial Infection
20% cases were diagnosed to be suffering from bacterial infection.
The most common HRCT finding in bacterial infection was lobar consolidation seen in 66.6% patients, Magnenat et al., and Boiselle et al., reported that focal consolidation was observed in approximately 45-60% of patients with pyogenic infection [20,21].
Selwyn et al., found that the combination of focal consolidation of chest radiography and a history of fever for fewer than seven days were associated with a sensitivity of 48% and a specificity of 94% for the diagnosis of bacterial pneumonia [22].
Carolyn M. Allen et al., reported that abnormalities may be detected on HRCT in the absence of any CXR findings These include bronchiectasis and evidence of small airway disease, with ill-defined centrilobular micronodularity and branching structures or tree-in-bud appearance secondary to mucus impaction in the bronchioles. Mosaic attenuation may also be present due to air trapping [7].
III. Pneumocystis jiroveci Pneumonia
A total of four patients in our study were diagnosed to be suffering from Pneumocystis jiroveci pneumonia. The diagnosis was established on the basis of HRCT findings and the clinical profile of the patients along with the findings of bronchoalveolar lavage (BAL) [Table/Fig-10].
29 year old HIV-positive patient. HRCT axial images (a) through upper lobes (b) subcarinal level shows areas of crazy paving and multiple tiny cysts. Focal area of consolidation is also seen in right side. Pneumomediastinum is also noted. Pneumocystis jiroveci pneumonia
Benito et al., reported that High-resolution computed tomography (HRCT) has a high sensitivity for PCP (100%) and a specificity of 89% [3].
Pneumocystis pneumonia typically presents with extensive ground-glass attenuation that may be patchy or diffuse with a central, perihilar and upper lobe predominance. Accompanying findings may be the thickening of the interlobular septae and rarely the “crazy paving” pattern. Less common manifestations may include the upper lobe lung cysts and areas of consolidation. Differentiating findings from HP may be the presence of upper lobe cysts and the associated “crazy paving” pattern. History of immunosuppression, and especially AIDS, favours the diagnosis of Pneumocystis pneumonia [23].
HRCT is very sensitive, the hallmark being ground-glass attenuation, seen in over 90% of the cases and often has a geographic or mosaic distribution, reflecting accumulation of intra-alveolar fibrin, debris, and organisms [7].
In a multi-center retrospective study by S Tasaka et al., CT showed diffuse or widespread ground-glass opacity (GGO) in all of the patients evaluated [24].
Conclusion
HRCT is a highly sensitive tool for detecting lung parenchymal and interstitial lesions and allows better characterization of the lesions. The lesions which are not detected or are equivocal on plain radiographs are identified and can be categorized as being active or inactive and thus helps to plan timely management, thereby reducing the morbidity and mortality from respiratory diseases.
Recommendations
HRCT findings should always be correlated with clinical findings, CD4 counts and other available investigations before arriving at a diagnosis or differential diagnosis.
Finally the authors suggest that HRCT has the potential to be incorporated into the management protocols of HIV/AIDS patients coming with suspected pulmonary illness.