Atrophic Rhinitis Presenting with Ethmoidal Mucocele: A Case Report
Manjunath Dandinarasaiah1, Jyotirmay Hegde2, Srinish G3, Bijiraj V V4, Prajna L. Salian5
1Assistant Professor, Department of ENT, Karnataka Institute of Medical Sciences, Hubli,Karnataka, India.
2Assistant Professor, Department of ENT, SDM Medical College and Hospital, Sattur, Dharwad, Karnataka, India.
3Assistant Professor, Department of ENT, Sree Mookambika Institute of Medical Sciences, Kulasekhram, Kanyakumari,Tamil Nadu India.
4Junior Resident, Department of ENT, Karnataka Institute of Medical Sciences, Hubli,Karnataka, India.
5Junior Resident, Department of ENT, Karnataka Institute of Medical Sciences, Hubli,Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manjunath Dandinarasaiah Block No.11, KIMS GO QRTS, KIMS Campus, Vidyanagar, Hubli, Karnataka- 580022, India.
Phone: 9900520748,
E-mail: drmanjud@gmail.com
Atrophic rhinitis (AR) is a chronic debilitating nasal mucosal disease predominantly prevalent in tropical countries. In the present case a 70-year-old female presented with a swelling in the right medial canthal area for six months and had features of Atrophic rhinitis with large septal perforation leading to saddle nose deformity. Computed tomography pictures were suggestive of ethmoidal mucocele and was later decompressed endoscopically. The sequelae and complications of AR like nasal septal perforation, saddle nose deformity, chronic rhinosinusitis (CRS), local and systemic spread of infection, atrophic pharyngitis, laryngitis, dacryocystitis and nasal myiasis have been reported in literature. To the best of our knowledge, this is the first reported case of AR presenting with ethmoidal mucocele. A case of AR with CRS is to be treated with caution as it can lead to complications as it is often neglected.
Atrophic rhinitis, Mucocele
Case Report
A 70-year-old female presented to the Ear, Nose and Throat (ENT) Department with a swelling in the area of the right medial canthus for six months [Table/Fig-1]. It was insidious in onset and gradually progressed over six months. It was not painful and there was no history of watering from the eye or alteration in the vision. The patient had foul smelling nasal discharge, crusting in the nose and loss of smell for more than 10-years. There was associated external nasal deformity since five years. Patient had not received any treatment for the same.
On examination a swelling measuring 2.5x2cm was visualised in the area of the right medial canthus. It was firm in consistency, nontender and nonfluctuant. Saddle nose deformity was noticed. Anterior rhinoscopy revealed roomy nasal cavities with a large septal perforation involving both anterior and posterior parts of the nasal septum. There was atrophy of lateral wall of nose bilaterally associated with crusts in nasal cavity. The ocular movements were normal. On diagnostic nasal endoscopy a diffuse bulge was noticed in the anterior part of the right middle meatus.
A computed tomographic (CT) scan of the paranasal sinuses revealed well-defined, non enhancing fluid dense lesion in the right anterior ethmoidal region extending laterally into the right orbit with the destruction of the lamina papyracea [Table/Fig-2]. The right eye ball was displaced laterally. There was opacification in bilateral frontal, ethmoidal and maxillary sinuses and left sphenoid sinus.
Based on clinical and radiological findings a diagnosis of ethmoidal mucocele was made. It was decompressed endoscopically under general anesthesia. About 3 to 4 cc of yellow coloured pus was drained and the cavity was marsupialised. Immediate reduction in the size of the swelling was visualised intraoperatively [Table/Fig-3]. Biopsy from the nasal mucosa was taken in the same sitting which revealed features suggestive of AR. The pus and the core culture of the tissue yielded Klebsiella ozaenae. There was no recurrence in swelling at the end of three months of follow-up.
Pre-operative photograph of Ethmoidal mucocele and Saddle nose deformity
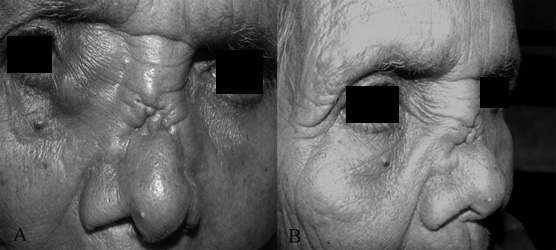
Post-operative photograph at the end of three months
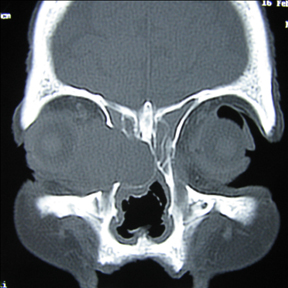
CT Paranasal sinuses - Coronal cut

Discussion
We are reporting the present case at the best of our knowledge, AR presenting with ethmoidal mucocele has not been reported in the literature so far.
The destruction of the nasal bone and cartilage predominantly occurs in severe cases of AR which if left untreated, eventually leads to septal perforation and saddle nose deformity. Whether the CRS is the cause or an effect of AR is not known, but is an association which is well established [1] .
Mucocele is an accumulation of the products of secretion, desquamation and inflammation within the paranasal sinus, with distention of the walls of the sinus [2] .
Mucoceles of the paranasal sinuses are well-known complication of CRS in adults [3] They arise more frequently at the level of frontal and ethmoidal sinuses while being less frequent within the sphenoid and maxillary sinuses [4] . The presence of CRS in the present case probably might have led to the formation of ethmoidal mucocele. Every ethmoidal cell may be a starting point for the mucocele formation which presses the surrounding lamellae. Anterior ethmoidal mucoceles are more common. The oculo-orbital symptoms which commonly occur are diplopia, chemosis and external displacement of eye ball.
In tropical countries, it is believed that the sinus surgeries for CRS in cases of AR can further aggravate the disease. This has led to the adoption of conservative treatment as a preferred modality over surgical management. Cases of Primary AR with evidence of obvious infections like cloudy sinus images, presence of mucopus in the sinuses and positive culture for Klebsiella ozaenae, had good recoveries following endoscopic sinus surgery (ESS).Candidate selection is a critical factor for the success of ESS in AR [5] . Hence it is imperative to consider surgical line of management for CRS whenever indicated.
The surgeon has to be aware of the possibility of performing Endoscopic sinus surgery in cases of Atrophic rhinitis associated with CRS in order to prevent the complications.
Conclusion
The presence of associated CRS has to be kept in mind while treating a case of AR. If neglected, CRS can lead to an array of complications. Hence it is important to manage CRS appropriately in every case of AR.
[1]. SN Dutt, M Kameswaran, The aetiology and management of atrophic rhinitisJ Laryngol Otol. 2005 119(11):843-52. [Google Scholar]
[2]. C Evans, Aetiology and treatment of fronto-ethmoidalmucoceleJ Laryngol Otol. 1981 95:361-75. [Google Scholar]
[3]. MD Guttenplan, Wetmore RF.Paranasal sinus mucocele in cystic fibrosisClin Pediatr (Phila) 1989 28(9):429-30. [Google Scholar]
[4]. PJ Conboy, NS Jones, The place of endoscopic sinus surgery in the treatment of paranasal sinus mucocelesClin Otolaryngol 2003 28(3):207-10. [Google Scholar]
[5]. SY Fang, YT Jin, Application of endoscopic sinus surgery to primary atrophic rhinitis? A clinical trialRhinology. 1998 36(3):122-7. [Google Scholar]