Case Report
A 21-year-old female came with a chief complaint of irregularly placed teeth in the upper and the lower front region. She had no medical and dental history. Her intra oral examination revealed mild crowding in relation to upper and lower anteriors and an increased overbite [Table/Fig-1,2] . She was decided to be treated by a nonextraction approach with a fixed appliance (M.B.T .022 slot). The bonding of the second molars with the “ Express prepared buccal tube bonding technique” was carried out because of inability to band the left second mandibular molar and frequent debonding of buccal tubes. We employed this bonding technique to correct the buccal occlusion and establish “ Andrews first key to occlusion that is intra arch alignment.
Both the mandibular 2nd molars were bonded using this custom technique for a better bond strength and to provide maximum resistance against being dislodged by the force of a higher dimension stainless steel wire as it is a requisite for levelling.
The increased surface area and adherence to anatomic details effect the bonding strength of the buccal tubes and ensure minimal breakage due to torsional stress.
Fabrication steps
1. Separating medium applied with a camel brush on the stone 1. model of the tooth to be bonded [Table/Fig-3] , The attachment surface base is coated with a home/ freshly prepared concentrated molten sugar solution [Table/Fig-4] . This solution can be conviniently made by adding sugar in boiling water and heating till it forms a sticky paste. The advantage of using sugar solution is its ease of availability and preperation and also the fact that its removal only requires water
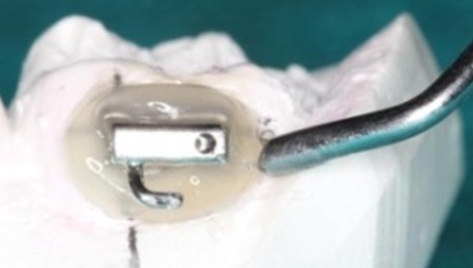
2. Light-cure composite resin (without the primer) paste*** is 2. adapted around the non-bondable surface of the base of the molar tube extending the same on the tooth surface mesio-distally and after removal of the excess [Table/Fig-5] ,maintaining the patency of the tube, the resin is partially cured [Table/Fig-6] . The light cure resin has to be adapted and spread evenly around the buccal tube so that a scaffold or template is built around it. Marginal adaptation of the composite can be carried out with a Teflon coated plastic filling instrument which shall be adapting the composite on the cast
3. The prepared customized base plus the molar tube are 3. removed en masse and the sugar coating is removed using a moisturized paint brush [Table/Fig-7] . This coating can easily be removed by water using a brush.The resin is trimmed and smoothened to reduce chances of plaque accumulation [Table/Fig-8] . Lower molar tubes with fabricated bases for enhanced bond-strength [Table/Fig-9] .
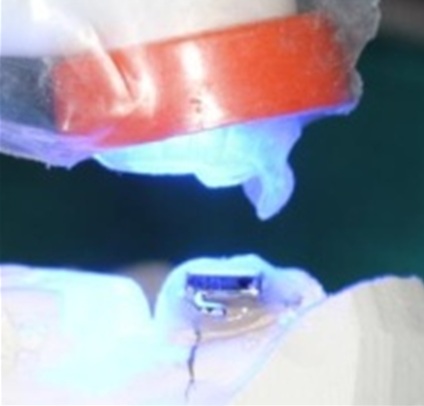
4. Bond the expressly fabricated molar tubes [Table/Fig-10] using light-cure adhesive.
*Victory series, 3M Unitek, Monrovia, CA, USA
**Millenium International, New Delhi, India
*** Transbond XT, 3M, Monrovia, CA, USA
Discussion
The advances in any specialty of dentistry enable the clinician to overcome previous generation limitations of materials used, be more efficient in terms of quality work and save clinical time.
These advances exist in harmony with innovations in biomaterials and various techniques employed in formulations and usage.
Likewise, orthodontic bonding has replaced banding for majority of the teeth present in dentition, though with its own limitations which include unacceptable bond strengths for various clinical situations as well as the constraint of isolation in the molar region.
Molar attachments were bonded using the premier indirect bonding technique by Silverman and Cohen [1] .
Debonding and subsequent delay in treatment time is so common that it tends to co exist as a nightmare for many practitioners. In one of the research studies, the survival analysis demonstrated molar bonds were more likely to fail compared with molar bands [2] .
In the United States a systematic study showed that only 22- 30% of the orthodontists bond the molars [3] . This fact is contributed to the clinical failure rate of 14.8% of this procedure [4,5] .
The various forms of bondable molar tube base designs* and areas** [Table/Fig-11,12] have been reformed to overcome the aforementioned clinical shortcomings, thus reducing the failure rate.
Molar bonding has even been regarded as more cost-effective when compared to banding [6] . This generally owes to the fact of reducing the large inventory that one comes across when banding is employed for molars.
Bonding ensures less time and less pain for the patient as the requirement for separation is nullified. Involvement of pain during banding procedures also cannot be ruled out which gives bonding an upper edge when seen from the patient’s perspective
The pre-formed base concavity on the bracket/ molar-tube bases undoubtedly plays a critical role in retention property but a custommade base especially for bonding molar-tubes in the region of problematic isolation would be a method of choice.
Inadequate adaptability and non-approximation is a very common reason for bond failure. Complex anatomy of teeth especially third and second molars, attributes to this consequence.
Bonding of molar tubes is often preffered over banding owing to the fact that chances of periodontal problems and occurrence of proximal caries is negated
One of the most common sequelae of banding is proximal caries and periodontal insult if the band surfaces cause impingement of the gingival tissues. The fact of carrying a large inventory for covering various sizes also adds on to the delimma and decision of banding.
It has been mentioned in the literature that in spite of improvements in orthodontic biomaterials, there is still a need to improve existing bonding procedures [7] .
Besides the techninal and gingival problems encountered with banding of teeth, one major factor owes to the time taken for banding procedures. Forcing seperators and subsequently waiting for the space leads to a loss of time that most of the times is a top priority of the patient. The non feasability of regular appointments in a consulting practise also leads to an increased preference of bonding attachments.
The problems that are encountered with bonding of attachments on posterior teeth however cannot be overlooked. Difficulty in maintaining a dry field at the posterior region is challenging. High masticatory forces also pose a threat for regular debonding of the molar tubes. These limitations lead to reccurent debondings and susequent time delay in treatment. Banding has an edge over bonding as the banded auxillaries seldom need repair. The only problem encountered is occasional loosening of bands which can be recemented.
The failure rates of bonding molar tube attachments can definitely be reduced by using the expressly fabricated molar bonding technique used. Though this would require a more statistical and quantitative measurement approach which calls for further research.
A minimum permissible bond strength had been suggested by Reynolds to be 5.88 – 7.85 MPa [8] . On the other hand, the maximum bond strength should be less than a maximum of 16 MP in order to avoid damage to enamel during debonding [9] . Transbond XT employed as bonding adhesive agent has been used both at the tube base as well as the scaffold. Mean shear bond strength of Transbond XT in the dissertation by Bharali have shown to be >10MPa which is only at the tube base [10] . The shear bond strength during debonding should not exceed the limit to enamel fracture (hence the importance of ARI scores). Therefore, the use of Transbond XT (which is an established bond material both in terms of initial bond strength as well as shear bond strength as a mean) as bonding material and for fabrication of the molar surface scaffold can be justified. Banding however poses its own technical problems at times. The complex anatomy of the second and third molar renders the clinician a great deal of inability to band. It is in such cases that bonding becomes preferrable along with its preferential incline for clinical practise.
The very reason for using the “Express Fabrication” technique was to increase the bond strength and reduce breakage of molar tubes.
The template or scaffold of resin that is bulit around the molar tube is carefully adapted on to the molar surface initially by indirect bonding [Table/Fig-5] . It is thoroughly adapted checked and adjusted before being directly bonded on to the tooth surface [Table/Fig-9] . Indirect bonding gives an edge over direct as the anatomy of the tooth can be adhered to and precise fit of the composite resin extensions take place on the cast followed by the tooth surface. The molar tubes bonded in the case shown [Table/Fig-10] stayed throughout the treatment without any event of debonding.
The increased mesiodistal coverage by the composite resin not only ensured a better bond strength, it also ensured a more precise fit when compared to the usage of molar bands. This study aims in assisting the clinician to bond attachments in a similar way when posterior anatomy is a concern and bond strength is of maximum consideration.
Intra oral frontal view (Pre Treatment photographs)

Intra oral occlusal views mandibular and maxillary (Pre Treatment photographs)

Separating medium applied

Sugar solution application on molar tube base

Composite scaffold formed around tube (Follow up photographs)
Easy removal of sugar solution easily from tube base.

Composite scaffold being trimmed and shaped (Follow up photographs)

lower Right and Left sides tube prepared

The prepared molar tubes bonded on mandibular second molars

Bondable molar tube design and shape area (Follow up photographs)

A different base design and shape area (Follow up photograph)

Conclusion
Bonding molar tubes has always been a dilemma for the orthodontist. The technique described in the present article has lucidly described the manner to overcome the relative demerits of bonding over molar banding.
An effective and handy method for establishing an extended surface area for molar tube bonding can be used for
(i) second molar region,
(ii) lingual molar tubes
(iii) teeth with abnormal morphology,
(iv)teeth with accompanying gingival enlargements due to their distal location in the oral cavity making it difficult to maintain oral hygiene and
(v) the added issue of increased inflammation caused during/ post banding procedure(s) is also prevented.
A short and quick laboratory work is required for the said technique, but is worth the efforts put in when the overall success and advantages of bonding seem to overpower the virtues of the molar casing (banding procedure).
There is scope for a further improvement in the article as the bond strength with this technique can be assesed using a universal testing machine to adequately compare bond strength with normal bonding procedures.
[1]. E Silverman, M Cohen, The twenty-minute full strap-up.J Clin Orthod. 1976 10:764-8. [Google Scholar]
[2]. M Nazir, T Walsh, NA Mandall, S Matthew, D Fox, Banding versus bonding of first permanent molars: a multi-centre randomized controlled trial.J Orthod. 2011 38:81-9. [Google Scholar]
[3]. RG Keim, EL Gottlieb, AH Nelson, DS Vogels, 2002 JCO study of Orthodonticdiagnosis and treatment procedures. Part 1. Results and trends.J Clin Orthod. 2002 36:553-68. [Google Scholar]
[4]. RA Linklater, PH Gordon, NH Olsen, JJ Hefferren, Bond failure patterns in vivoAm J Orthod Dentofacial Orthop. 2003 123:534-9. [Google Scholar]
[5]. N Pandis, L Christensen, T Eliades, Long-term clinical failure rate of molar tubes bonded with a self-etching primer. Angle Orthod. 2005 75:1000-2. [Google Scholar]
[6]. PG Murray, DT Millett, M Cronin, Bonded molar tubes: a survey of their use by specialist orthodontists.J Orthod. 2012 39:129-35. [Google Scholar]
[7]. A Pasquale, M Weinstein, AJ Borislow, LE Braitman, In-vivo prospective comparison of bond failure rates of 2 self-etching primer/adhesive systems. Am J Orthod Dentofacial Orthop. 2007 132:671-4. [Google Scholar]
[8]. Reynolds A review of direct bonding orthodontics.Br J Orthod. 1975 2:171-8. [Google Scholar]
[9]. C Jose, Castro De, Areas requiring further research in testing of orthodontic shear bond strengths. J Clin Orthod. 2007 41(3):135-7. [Google Scholar]
[10]. T Bharali, PJ Sheridan, An Evaluation Of Mean Shear Bond Strength Of Molar Tubes With Various Bonding Materials-An In Vitro Comparative Study [unpublished dissertation]. Rajiv Gandhi University of Health SciencesJ Periodontol 2005 [Google Scholar]