Churg Strauss Syndrome – A Case Report
Mallikarjun Shetty1, Ramakrishna Janapati2, Krishnaprasad A3, Nageshwara Rao M4
1Assistant Professor, Department of Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India.
2Senior Resident, Department of Cardiology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India.
3Professor, Department of Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India.
4Professor, Department of Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramakrishna Janapati, Senior Resident, Department of Cardiology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana-500082, India.
A male aged 45-years presented with complaints of fever for 7days, cough, breathlessness for 4 days, tingling of hands, feet and weakness of both hands and feet for 4 days duration. He was a known asthmatic with history of recurrent sinusitis in the past. On examination he had bilateral polyphonic wheeze and evidence of distal asymmetric sensory neuropathy with motor weakness. And on investigation he had eosinophilia, pulmonary function test showed reversible airway obstruction,nerve conduction studies revealed mononeuritis multiplex, muscle biopsy suggestive of eosinophilia infiltration, nerve biopsy suggestive of vacuities, 2DECHO showed RWMA in inter ventricular septum, Coronary angiogram showed narrowing in distal LAD territory. In view of sinusitis, asthma, eosinophilia, tissue infiltration by eosinophils we made a diagnosis of Churg Strauss syndrome.
Churg Strauss syndrome (CSS), Regional wall motion abnormality (RWMA), Left anterior descending artery (LAD), Pulmonary function test (PFT)
Case Report
A 45-year-old male patient presented with complaints of fever and myalgias for 7 days duration, parasthesias and weakness of both hands and feet for 4 days, cough and breathlessness and wheeze for 4 days duration. He had difficulty in holding objects with the hands and difficulty in walking. He had history of sinusitis in the past underwent sinus surgery seven years and then two years back. He was a known asthmatic on intermittent inhaler use since five years. He had history of exacerbation of asthma one month back, treated with Methylprednisolone, Monteleukast, IV antibiotics and other supportive measures. He had no history of Diabetis mellitus, Hypertension, coronary artery disease in the past.
His general examination was unremarkable. Pulse rate was 108/minutes, respiratory rate 28/minutes and blood pressure was 120/70 mm Hg. Respiratory system examination revealed bilateral expiratory Ronchi. Nervous system examination revealed bilateral asymmetrical distal muscle weakness with sensory loss. Deep Tendon Reflexes were not elicitable in both upper and lower limbs, except the Biceps reflexes. Other system examination were normal.
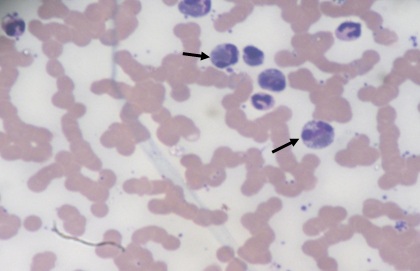
Investigations revealed hemoglobin 11.7 gm/dl, total Leukocyte count 21,700 cells/mm3, (Neutrophils 64%, Lymphocytes 15%, Monocytes 1% and Eosinophils 20%) [Table/Fig-1], platelet count 3.0 lakhs/mm3, ESR 70 mm and absolute eosinophil count was 4000cells/mm3. Renal function tests were normal but had mild Hepatopathy. Creatinine phosphokinase was 532U/L (normal upto 200 U/L) CPK-MB is normal, Troponin T-test was negative. There was sinus tachycardia in Electrocardiogram but Echocardiogram showed hypokinesia in septum and anterior wall. Coronary angiogram showed mild single vessel disease in Left anterior descending coronary artery territory. Chest radiograph was normal. There were no ova and cysts in stools. Smear for microfilaria was negative. ANA, anti dsDNA and c-ANCA were negative. P-ANCA (perinuclear antineutrophil cytoplasmic antibody) (ELISA) was positive.
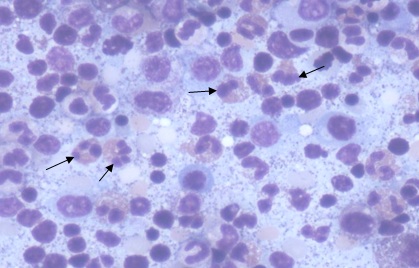
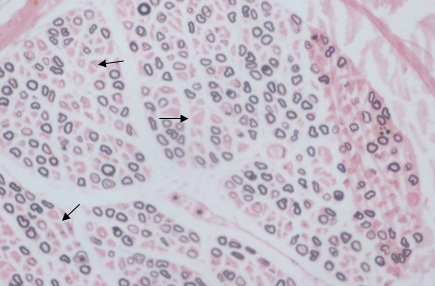
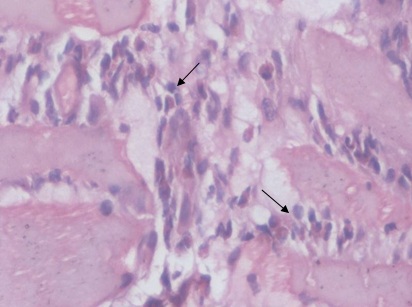
Nerve conduction Studies were suggestive of mononeuritis multiplex. There was reversible airway obstructive abnormality on spirometry. His base line FEV1 was 68% of predicted value witch increased to 90% of predicted FEV1 after bronchodilator testing suggestive of reversible airway obstruction. Bone marrow study revealed increased number of eosinophils and their precursors. There was no blast prominence [Table/Fig-2]. Nerve biopsy showed features of chronic axonopathy with patchy demyelination [Table/Fig-3]. Muscle biopsy showed infiltration by eosinophilic infiltrate with features of eosinophilic vaculitis [Table/Fig-4].
He was treated with intra venous Methyl Prednisolone 1gram once a day for three days and Cyclophosphamide 750 mg intravenously (15 mg/kg) once in two weeks x three doses, once in three weeks x three doses. Followed by maintenance with Azathioprine 100mg once daily and oral Prednisolone in tapering doses. And other medication with aspirin, statins, ACE inhibitors, isosorbide mononitrate, physiotherapy. Patient improved and able to walk without any support from a bed bound state. No recurrence of symptoms since two years of follow up.
Discussion
Our patient satisfied the diagnostic criteria of Churg-Strauss syndrome with asthma, eosinophilia and a vasculitis involving the peripheral nerves, muscle, heart, supported by positive p-ANCA and characteristic sural nerve biopsy findings. The diagnosis of CSS made based on ACR 1990 [1]. Criteria for the Classification of Churg-Strauss syndrome. The criteria includes asthma,eosinophilia >10%, neuropathy, non-fixed Pulmonary infiltrates, Paranasal sinus abnormality, Extravascular eosinophils. For classification purposes, a patient shall be said to have Churg-Strauss syndrome (CSS) if at least four of these six criteria are positive. The presence of any four or more of the six criteria yields a sensitivity of 85% and a specificity of 99. 7% (Masi et al.,) [1]. Although not a criterion of CSS diagnosis, the presence of ANCA, especially MPO‐ANCA, is frequent in CSS [2]. Regularly, a history of asthma and rhinosinusitis precedes the appearance of the syndrome itself [3]. In our case asthma was present years before the CSS. Cardiac involvement occurs frequently in CSS, and results in significant morbidity and mortality [4]. Cardiac involvement may result from vasculitis- related ischemia affecting small myocardial vessels and coronary arteries, and from eosinophilic myocardial infiltration. Our case also had regional wall motion abnormality in 2D echocardiography but Coronary angiogram did not reveal any significant disease this patient may had vasulitis involving small myocardial blood vessels. The pattern of neurological involvement may be that of mononeuritis multiplex, symmetrical or asymmetrical polyneuropathy [5]. In our case it was Fulminant form of mononeuritis multiplex. Muscle biopsy helps in the demonstration of systemic vasculitis [6], as in our case insert as muscle biopsy also proven that the presence of extravasular eosinophils and it was one of the criteria for diagnosis of CSS. Corticosteroids are the first-line recommended treatment for CSS and adjuvant immunosuppressants are used for severe disease [7,8]. Our patient was considered to have severe disease and he was thus treated with combination therapy immediately Intravenous cyclophosphamide was preferred as it has been shown to cause fewer adverse effects than oral cyclophosphamide. Corticosteroids and immunosuppressants, especially cyclophosphamide, have considerably improved the prognoses and overall survival rates in patients with systemic vasculitis.
Peripheral smear showing Eosinophilia
Bone marrow aspirate showing marrow eosinophilia
Nerve biopsy shows patchy demyelination of Neurons
Muscle biopsy shows infiltration by eosinophils
Conclusion
We conclude that, Churg-Strauss syndrome complicated frequently with Fulminant form of polyneuropathy, and Cardiac involvement. Remission depends on early aggressive immunosuppressive therapy and long term follow-up. Overall the prognosis of a treated case of CSS appears good with adequate treatment with immunosuppressive medication.
Acknowledgements
Patient and his family members, all my teachers and colleagues. Srinivasan VR, Manmadha Rao T, Narsimhulu, Liza Rajasekhar, Varaprasad, Megha S Uppin, Rukmini Mridula, Seshagiri Rao D.
[1]. AT Masi, GG Hunder, JT Lie, BA Michel, DA Bloch, WP Arend, The AmericanCollege of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome .(allergic granulomatosis and angiitis). Arthritis Rheum. 1990 33:1094-100. [Google Scholar]
[2]. GS Hofman, U Specks, Antineutrophil cytoplasmic antibodies.Arthritis Rheum. 1998 41:1521-37. [Google Scholar]
[3]. YJ Jeong, K Kim, IJ Seo, Eosinophilic lung diseases: a clinical radiologic, and pathologic overview.Radiographics. 2007 27:617-37. [Google Scholar]
[4]. L Guillevin, P Cohen, M Gayraud, Churg–Strauss syndrome. Clinical study and long-term follow-up of 96 patients.Medicine (Baltimore). 1999 78:26-37. [Google Scholar]
[5]. E Kararizou, P Davaki, K Spengos, N Karandreas, A Dimitracopoulos, D Vassilopoulos, Churg-Strauss syndrome complicated by neuropathy: a clinicopathological study of nine cases.Clin Neuropathol. 2011 30(1):11-7. [Google Scholar]
[6]. B Hervier, C Durant, A Masseau, T Ponge, M Hamidou, JM Mussini, Use of muscle biopsies for diagnosis of systemic vasculitides.J Rheumatol. 2011 0338(3):470-4. [Google Scholar]
[7]. M Gayraud, L Guillevin, P Toumelin, The French Vasculitis Study Group. Long term follow-up of polyarteritis nodosa, microscopic polyangiitis and Churg– Strauss syndrome. Analysis of four prospective trials including 278 patients.Rheum. 2001 44:666-75. [Google Scholar]
[8]. AQ Rana, A Adlul, Delay in diagnosis of Churg-Strauss syndrome: a case report.Scott Med J. 2012 57(4):247 [Google Scholar]