To Study the Levels of C - Reactive Protein and Total Leucocyte Count in Patients Operated of Open and Laparoscopic Cholecystectomy
Ritesh Kohli1, Ekta Bansal2, Ashwani K Gupta3, Prithpal S Matreja4, Kulwinder Kaur5
1Ex-Resident, Department of General Surgery, Government Medical College and Rajindra Hospital, Patiala, India.
2ID Fellow,Carilion Roanoke Memorial Hospital, Virginia, U.S.A.
3Associate Professor, Department of Pharmacology,Gian Sagar Medical College, Ram Nagar, Rajpura, Patiala, India.
4Associate Professor, Department of Pharmacology,Gian Sagar Medical College, Ram Nagar, Rajpura, Patiala, India.
5Medical Officer,Civil Hospital, Amritsar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prithpal Singh Matreja, Associate Professor, Department of Pharmacology, Gian Sagar Medical College and Hospital, Ramnagar, Rajpura, Patiala, India.
Phone: + 91-9855001847; Fax: +91-1762-520024,
E-mail: drpsmatreja@yahoo.co.in
Background: The recovery from laparoscopic cholecystectomy (LC) is rapid and most of the patients are discharged on the 1st post-operative day. There is an increased concentration of certain serum proteins, known as acute-phase reactive proteins (APRP) during the post-operative period depends on the degree of tissue damage and the inflammatory reaction. There is a direct positive correlation between the concentrations of APRP, especially C-reactive protein (CRP), and the severity of inflammation. This study was done to study the levels of C - reactive protein and Total Leucocyte Count in patients operated either by Open Cholecystectomy (OC) and Laparoscopic Cholecystectomy (LC).
Materials and Methods: This prospective study was conducted on 50 patients after approval from the Institutional Ethics Committee. Twenty five patients underwent open cholecystectomy and the other 25 had laparoscopic cholecystectomy. The pre and post operative concentrations of serum C-reactive protein (CRP) and total leukocyte count (TLC) were compared in both the groups.
Results: There were no differences in the preoperative serum CRP and TLC concentrations – in both the groups. Serum CRP rose significantly following OC compared to that of patients who underwent LC (10.52 ± 1.96 mg% vs. 8.88 ± 1.23 mg %). There were also significant differences in the post-operative TLC ( 9.49 ± 1.05 m/mm3 for the OC group vs. 8.57 ± 1.31 m/mm3 for the LC group), and the post-operative hospital stay (5.5 ±1.5 days vs. 1.9 ± 0.9 days). There was no correlation between serum CRP concentrations and the other post-operative parameters.
Conclusion: The study provided the biochemical evidence supporting the clinical observation that LC is far less traumatic to the patient than OC.
Cholecystectomy, Laparoscopy, Patients, Surgery
Introduction
The recovery from LC is rapid and most of the patients are discharged on the 1st post-operative day [1-3]. The post-operative hospitalization period following LC (2days) is shorter than that following OC (2.4 ± 0.57 days). Injury or inflammation of the human body results in increased concentrations of certain serum proteins, known as acute-phase reactive proteins (APRP). The main influence on the concentration of APRP during the post-operative period depends on the degree of tissue damage and the inflammatory reaction associated with the repair and regeneration processes which act to restore the integrity of the injured tissue [4]. There is a direct positive correlation between the concentrations of APRP, especially C-reactive protein (CRP), and the severity of inflammation [5,6]. CRP is very consistent in response and is, therefore, the most satisfactory single screening test for an “acute phase” reactant [5]. CRP is a component of normal serum [7], which rises more dramatically than any other protein after surgical trauma [8-10,11]. CRP begins to rise 4-12 h post-operatively, reaches the peak level after 24-72 h, and returns to normal after 2 weeks [8,1213,14]. Hence, this study was done to quantify the difference in tissue damage between open cholecystectomy (OC) and laparoscopic cholecystectomy (LC).
Materials and Methods
This prospective study was conducted on 50 patients during the 6-months period (November 2008 to April 2009) at Government Medical College and Rajindra Hospital, Patiala, India after approval from the Institutional Ethics Committee. Patients undergoing either open or laproscopic cholecystectomy in the age group of 18-60 years and willing to give written informed consent were included in the study. All patients undergoing concomitant common duct exploration or any additional procedures, jaundice patients, and patients with acute cholecystitis, patients who were converted from laparoscopic cholecystectomy to open cholecystectomy, a history of steroids intake, a history of chemotherapy, on oral contraceptive, and requiring blood transfusion were excluded from the study. Pregnant and lactating females were not included in the study.
All patients with chronic, symptomatic cholelithiasis as proven by ultrasonography underwent surgery under general anaesthesia. OC was performed through a right sub costal incision, while a four-cannula technique was used for LC. Serum samples were collected from all patients before the operation and 24 h post-operatively. CRP levels were measured by immunoturbidimetric assay (AXIS– SHIELD PoC AS Norway), TLC was also assessed. The duration of post-operative hospitalization was estimated.
Statistical Analysis
Student’s t-test used to find statistically significant difference and results were expressed as means +SD. Linear correlation analysis used for evaluation of results of CRP and other post operative parameters.
Results
All the patients enrolled in the study underwent cholecystectomy for chronic, symptomatic cholelithiasis confirmed by ultrasonography. OC was performed in 25 patients and LC was performed in similar number of patients. The group treated by OC comprised four men and 21 women with an age range of 23 to 43 years and mean age of 35.72 ± 4.558 years, whereas the group treated by LC included three men and 22 women in range of 22 to 42 years, and a mean age of 36.36 ± 3.463 years. Both the groups were comparable in demographic profile at baseline.
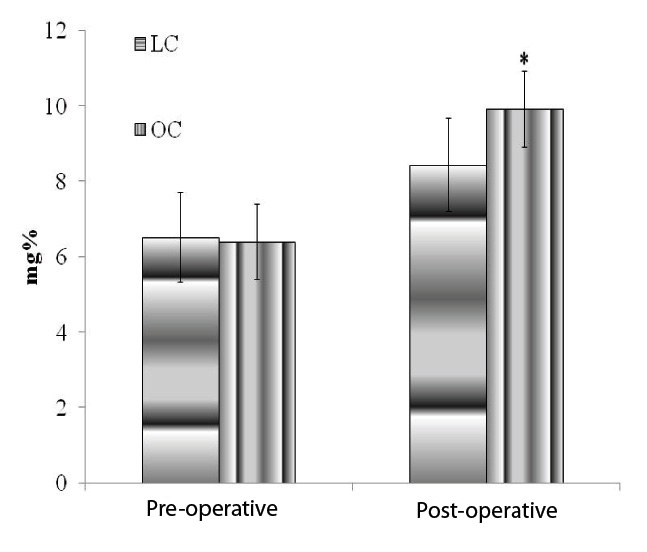
Serum CRP concentrations
The preoperative CRP concentration was comparable in groups, 6.52 ± 1.194 mg% for the LC group and 6.4 ± 1.041 mg% for the OC group. The post-operative CRP concentration for patients treated by LC was 8.44 ± 1.227 mg% and for patients undergoing OC it was 9.92 ± 1.913 mg% [Table/Fig-1]. Hence, there was a significantly higher increase in serum CRP levels in the patients following OC compared to following LC (p < 0.001).
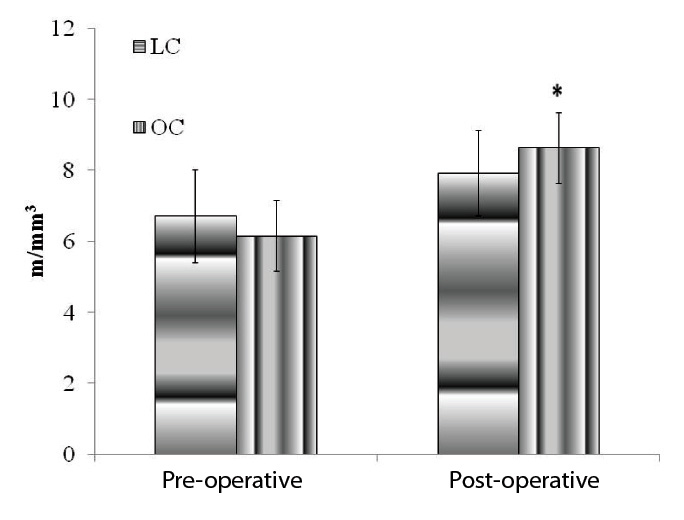
Serum CRP concentrations
The preoperative total leukocyte count was comparable at baseline, for the LC group were 6.724 ± 1.302 m/mm3 and 6.161 ± 0.983 m/mm3 for the OC group. The post-operative count was significantly higher in both groups, for the LC group was 7.9128 ± 1.198 m/mm3, p < 0.01 when compared to the preoperative count. The post-operative count for the OC group was 8.6368 ± 1.047 m/mm3, p < 0.001 when compared to the pre-operative count. Statistical analysis shows significantly higher post-operative counts for patients undergoing OC (p < 0.001) [Table/Fig-2].
Comparison of CRP in both groups
Comparison of TLC in both groups
Discussion
Since the introduction of LC into our institution, we have been amazed to see how easily and rapidly patients recover from surgery as compared to those undergoing OC. It was estimated that the injury to the skin, abdominal wall, and peritoneum would be larger during OC and searched for an objective, quantitative parameter with which to evaluate the differences in surgical trauma. It was observed that serum CRP concentration was the most suitable parameter for this purpose because it is the plasma protein which rises most dramatically and consistently after surgical trauma [5,9].
Our study confirmed our preliminary hypothesis that OC causes a major tissue trauma when compared to LC. In patients undergoing OC, rise in CRP was significantly high compared to LC group [10,11]. Another study showed no significant difference in the CRP levels [15]. Although significant differences in post-operative WBC counts are observed, there is no significant correlation between it and serum CRP concentrations. Aronson et al.,[8] have already established that leucocytes are not involved in the increased synthesis of APRP, as the same response was seen in patients with agranulocytosis. As in other comparative studies [1,2,3,16,17], the post-operative hospital stay of our patients undergoing LC was markedly shorter than those undergoing OC.
Although the study was a prospective one, the patients were not randomized to either group. However, since every patient was his own control, the lack of randomization has had no effect on the results. Moreover, the baseline CRP levels in both groups were similar, and changed only following surgery. The magnitude of the acute-phase response on 1st post-operative day in the LC group was less pronounced as compared to OC group and this may be one of the indicators of reduced tissue trauma in LC. The present study reflects the impact of surgical access on post-operative levels of stress markers (TLC and CRP). Thus, the reduced tissue trauma, probably may be considered as one of the contributory factors in labeling LC as “Gold Standard” operation for cholelithiasis.
[1]. BD Schirmer, SB Edge, J Dix, MJ Hyser, JB Hanks, RS Jones, Laparoscopic cholecystectomy. Treatment of choice for symptomatic cholelithiasis.Ann Surg. 1991 213:665-76. [Google Scholar]
[2]. M Airan, M Appel, G Breci, AJ Coburg, M Cohen, A Cuschieri, Retrospective and prospective multi-institutional laparoscopic cholecystectomy study organized by the Society of American Gastrointestinal Endoscopic Surgeons.Surg Endosc. 1992 6:169-76. [Google Scholar]
[3]. KA Zucker, RW Bailey, TR Gadacz, AL Imbembo, Laparoscopic guided cholecystectomy.Am J Surg. 1991 161:36-44. [Google Scholar]
[4]. PG Shakespeare, AJ Ball, ED Spurr, Serum protein changes after abdominal surgery.Ann Clin Biochem. 1989 26:49-57. [Google Scholar]
[5]. RA Crockson, CJ Payne, AP Ratcliff, JF Soothill, Time sequence of acute phase reactive proteins following surgical trauma. Clin Chim Acta. 1966 14:435-41. [Google Scholar]
[6]. D Thompson, A Milford-Ward, JT Whicker, The value of acute phase protein measurements in clinical practice.Ann Clin Biochem. 1992 29:123-31. [Google Scholar]
[7]. DR Claus, AP Osmand, H Gewurz, Radioimmunoassay of human C-reactive protein and levels in normal sera. J Lab Clin Med. 1976 87:120-8. [Google Scholar]
[8]. KF Aronsen, G Ekelund, CO Kindmark, CB Laurell, Sequential changes of plasma proteins after surgical trauma.Scand J Clin Lab Invest Suppl. 1972 124:127-36. [Google Scholar]
[9]. M Werner, D Odenthal, Serum protein changes after gastrectomy as a model of acute phase reaction. J Lab Clin Med. 1967 70:302-10. [Google Scholar]
[10]. M Grande, GF Tucci, O Adorisio, A Barini, F Rulli, A Neri, Systemic acute phase response after laparoscopic and open cholecytectomy.Surg Endosc. 2002 16:313-16. [Google Scholar]
[11]. K Janicki, J Bicki, E Radzikowska, R Madej, B Burdan, C-reactive protein (CRP) as a reponse to post-operative stress in laparoscopic cholecystectomy using the abdominal wall lift, with performed pneumoperitonium (CO2), and in open cholecystectomy.Ann Univ Mariae Curie Sklodowska Med. 2001 26:397-402. [Google Scholar]
[12]. JG Conner, PD Eckersall, J Ferguson, TA Douglas, Acute phase response in the dog following surgical trauma. Res Vet Sci. 1988 45:107-10. [Google Scholar]
[13]. H Ohzato, K Yoshizaki, N Nishimoto, A Ogata, H Tagoh, M Monden, Interleukin-6 as a new indicator of inflammatory status: detection of serum levels of interleukin-6 and C-reactive protein after surgery.Surgery. 1992 111:201-9. [Google Scholar]
[14]. EA Pullicino, F Carli, S Poole, B Rafferty, ST Malik, M Elia, The relationship between the circulating concentrations of interleukin 6 (IL-6), tumor necrosis factor (TNF) and the acute phase response to elective surgery and accidental injury.Lymphokine Res. 1990 9:231-8. [Google Scholar]
[15]. F Froghi, MH Sodergren, VJ Wright, R Coomber, AP Courtney, A Darzi, Single-Center experience in systemic stress and short-term morbidity of singleincision cholecystectomy. Surg Innov. 2012 19:117-22. [Google Scholar]
[16]. PA Grace, A Quereshi, J Coleman, R Keane, G McEntee, P Broe, Reduced post-operative hospitalization after laparoscopic cholecystectomy. Br J Surg. 1991 78:160-2. [Google Scholar]
[17]. NJ Soper, JA Barteau, RV Clayman, SW Ashley, DL Dunnegan, Comparison of early post-operative results for laparoscopic versus standard open cholecystectomy.Surgery, Gynecology & Obstetrics. 1992 174:114-7. [Google Scholar]