The effective elimination of the plaque mass and the microorganisms by scaling and root planing have been well documented, but the inability to access deep and tortuous pockets has proven to be a major drawback [1]. This had led to the adjunctive use of antimicrobial agents usually in the form of irrigants or systemic antibiotics to overcome the limitations of conventional treatment. These procedures however were questionable as antimicrobial irrigants did not seem to be effective enough and subjecting a patient to a long term systemic administration of antibiotics was not feasible. It was for this reason that local drug delivery systems evolved, in order to achieve antimicrobial activity at the base of the pocket and remain active for a time to inhibit growth of pathogenic bacteria [2].
Initial studies on the oral use of chlorhexidine suggested that this dicationic bisbiguanide demonstrated a plaque inhibitory effect [3].This resulted primarily from the binding of the antiseptic to anions present on the tooth surface. As a result of the considerable affinity of chlorhexidine to oral structures, the formation of reservoirs of this antiseptic was proposed. Slow releases from these reservoirs were thought to create a bacteriostatic milieu around the teeth. Chlorhexidine possesses most of the characteristics of the ideal antimicrobial described by Van der Ouderaa [4]. Therefore, a locally delivered system containing chlorhexidine along with conventional therapy can be expected to control periodontal disease progression more effectively.
One such product, the Periochip TM (manufactured by Perioproducts Ltd, Jerusalem, Israel and is currently marketed in the US under the sponsorship of ASTRA. USA Inc.) [Table/Fig-1] is a biodegradable, local delivery system that contains 2.5 mg of chlorhexidine gluconate in a gelatine vehicle. Concentrations of the drug insitu were found to remain above the minimum inhibitory concentration for more than 99% of periodontal pocket flora for upto nine days.
This study was undertaken to estimate the inherent benefits of a biodegradable gelatin chip containing chlorhexidine in controlling chronic periodontitis.
Materials and Methods
This study was conducted in the Department of Periodontics Coorg Institute of Dental Sciences, Virajpet, Kodagu and the study was completed in a period of 12 months. The study consisted of 15 patients (45sites), both sexes;( males-6, females-9) in the age group between 35-55 years having moderate to severe chronic periodontitis (pocket depth of 5-8 mm). This study was approved by institutional ethical committee. Written and informed consent was obtained from all the participants. In each patient the treatment sites were divided randomly into three groups, randomization was done by coin toss method. The sample size was calculated adjusting the minimum acceptable power of the study at 80% and maximum allowable alpha error at 5%.
GROUP A - The periodontal pocket was treated by scaling and root planing alone.
GROUP B - The periodontal pocket was treated with scaling and root planing plus the placement of chlorhexidine chip (Periochip) [Table/Fig-2].
Placement of Periochip into Periodontal pocket after SRP

GROUP C – the periodontal pocket was treated with placement of chlorhexidine chip alone.
Criteria for patient selection
Subjects with moderate to severe chronic periodontitis characterized by atleast three sites with a probing depth of 5-8 mm. Diagnosis of periodontal disease was based on the 1999 classification of periodontal disease and condition. The study was carried from January to December 2008. Presence of minimum 15 natural teeth (minimum of atleast 4 teeth per quadrant), Subjects in a good state of health without any systemic disorder were considered for the study. On the other hand the exclusion criteria consisted of subjects with the history of allergy to chlorhexidine, systemic antibiotic therapy in the last six months, known history of systemic diseases that would alter the healing response of oral tissues, individuals who had undergone surgery in relation to the site within six months prior to the study and pregnant women.
Acrylic stents were made with cold cure clear acrylic material over the occlusal third which would act as a reference for probing [Table/Fig-3]. Oral prophylaxis was performed using ultrasonic scalers to remove the supra-gingival plaque. Root planing of the control and one test site was carried out using Gracey curettes before the chip placement; the other test site consisted of placement of chip without root planing.
Acrylic stunt placed on the occlusal one third for measuring PD

The patients were recalled after one month and three months for follow up wherein the clinical parameters were recorded [Table/Fig-4].
Post operative after 3 months of placement of periochip

The following clinical parameters were assessed at the same follow up appointments
Plaque index (PI) (Silness and Loe 1964) [5].
Gingival index (GI) (Loe and Silness 1963) [6].
Bleeding on probing (BOP).
Probing depth (PD).
Clinical attachment level (CAL).
Statistical Analysis
Descriptive statistical analysis has been carried out in the present study. T-test (two tailed, dependent) has been used to find the significance of study parameters. Analysis of variance (ANOVA) has been carried out in the present study. The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1,Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables.
Results
The plaque index was determined in order to assess the overall oral hygiene status of the patient. The results indicate a highly statistically significant reduction (p<0.001) of index scores between baseline and the 90th day [Table/Fig-5].
Descriptive statistics for plaque index (pi)
| Mean ± Sth. Deviation | n |
|---|
| Base pi | 1.3529 ± 0.49330 | 15 |
| Day 30 pi | 1.0067 ± 0.40662 | 15 |
| Day 90 pi | .9907 ± 0.37752 | 15 |
The mean gingival index [Table/Fig-6] score at baseline was: 1.7153 ± 0.620. and at 90 days was 1.094 ± 0.344.The results indicate a statistically significant reduction (p=0.05) of index scores between baseline and the 90th day.
Descriptive statistics for gingival index (gi)
| Mean ± Std. Deviation | n |
|---|
| Base gi | 1.7153 ± 0.62018 | 15 |
| Day 30 gi | 1.1407 ± 0.37653 | 15 |
| Day 90 gi | 1.0940 ± 0.34465 | 15 |
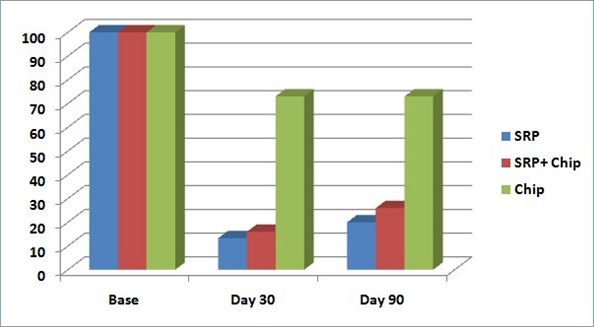
All three selected sites demonstrated bleeding on probing [Table/Fig-7] at baseline. Group A: (SRP) The percentage reduction of bleeding on probing between 0-90th day was 86.7%, (p<0.001) which was highly statistically significant. Group B: (SRP+ CHX chip). The percentage reduction of bleeding sites was 73.3%.also statistically very highly significant (p <0.001). Group C: (CHX chip)Sites with bleeding on probing were reduced by 26.7%.
Changes in bleeding on probing
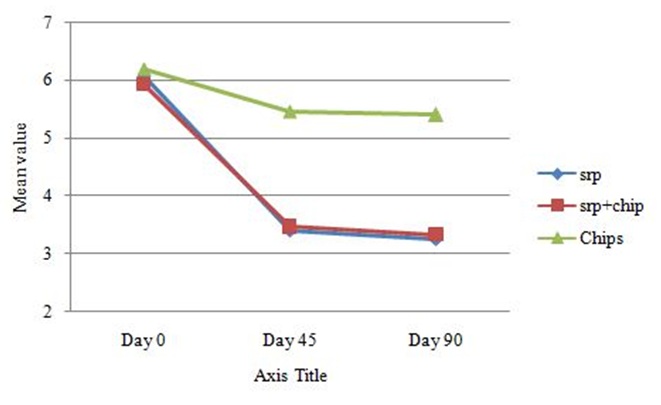
The probing depth [Table/Fig-8] in Group A: (SRP) At baseline the values were 6.06± 0.79 at day 30 the values were 3.40 ± 1.05, at 90 days the value was 3.26 ± 1.09 The statistics (p- value) of pocket depth reduction showed a highly significant reduction between 0-30th day and 0-90th day which was highly statistically significant. The p-value between the 30th and 90th day was not significant p= 0.16.Group B: (SRP+ CHX chip) Baseline values were 5.93 ± 0.59 at day 30 the values were 3.46 ± 1.18 and at 90 days were 3.33 ± 1.23.The statistics (p- value) of pocket depth reduction between 0-30th day, 0-90th day which was highly statistically significant. Group C: (CHX chip) Baseline values were 6.20 ± 0.56, at day 30 the values were 5.46 ±0.91 and at 90 days were 5.40 ± 0.98.The statistics (p-value) of pocket depth reduction between 0-30th day, 0-90th day were p= 0.00 which was statistically significant.
Changes in mean probing depth
At baseline the clinical attachment [Table/Fig-9] values for Group A: (SRP)were 6.0667 ± 0.79881 at day 30 the values were 3.40 ± 1.05 and at 90 days the value was 3.26 ± 1.09. The statistics (p- value) for gain in clinical attachment levels between 0-30th day and 0-90th day were p <0.001 which was highly statistically significant. The p-value between the 30th to the 90th day was p=0.164 which was not significant statistically.
Changes in mean clinical attachment level (CAL)
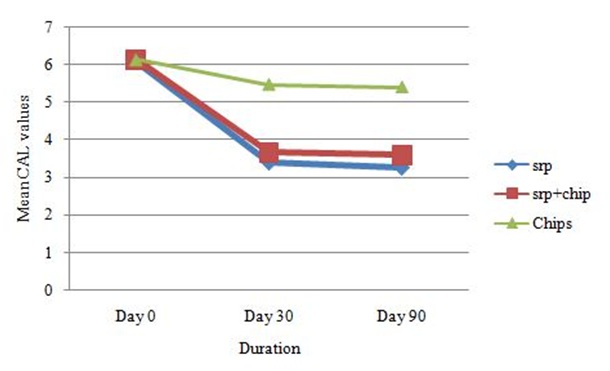
Group B: (SRP+ CHX chip)Baseline values were 6.13 ± 0.63, at day 30 the values were 3.66 ± 1.34 and at 90 days were 3.60 ± 1.35.The statistics (p- value) of clinical attachment gain between 0-30th day, 0-90th day were p= 0.00 which was statistically very highly significant but was not significant between 30 to 90 days; p= 0.334
Group C: (CHX chip) Baseline values were 6.13 ± 0.63, at day 30 the values were 5.46 ± 0.915 and at 90 days were 5.40 ± 0.98.
The statistics (p- value) of clinical gain in attachment between 0-30th day, 0-90th day were p= 0.00 which was statistically significant; between the 30th and 90th day there were no statistically significant changes the p-value was 0.582.
The results between Group A and Group B were not found to be statistically significant the probability values were, p= 0.551 at 30 days and p= 0.465 at 90 days.
Discussion
The role of bacteria in the pathogenesis of periodontal disease has been well documented. An essential component of therapy is to eliminate or control these pathogens. Traditionally this has been accomplished through mechanical methods i.e., scaling and root planing. In some instances SRP is not effective in removing sub-gingival biofilms especially in difficult to reach areas such as deep periodontal pockets. Over the past decade locally delivered, anti-infective pharmacological agents mostly employing sustained release vehicles have been introduced to achieve this goal. Evidence is suggestive that sustained release devices can indeed add to clinical benefits achieved by SRP [7].
The present study was carried out with the objective to evaluate the efficacy of a chlorhexidine containing local delivery system (Periochip) over scaling and root planing for a period of three months. All the parameters were recorded at baseline, 30th day and at three months.
The three month time frame was chosen because the effects of locally delivered chlorhexidine has been shown to be evident for eleven weeks after administration and also three months corresponds to the typical recall interval for patients after periodontal treatment [2].
Plaque index scores reflect the oral hygiene status of the patient. In the present study the full mouth plaque index scores from baseline to 30th day and 90th day was taken into consideration. There was a reduction in plaque index scores, which was statistically significant.
These findings are in accordance with the results obtained in studies conducted by Soaskolne et al., [8], Jeffcoat et al., [2], Heasman et al., [3]. This reduction in the scores can be attributed to scaling and root planing as well as adherence to oral hygiene instructions.
The gingival index scores were reduced significantly in both the groups from baseline till 90th day which were statistically highly significant The results are in accordance with the findings observed by Soskolne et al., [8], Jeffcoat et al., [2], Heasman et al., [3]. This reduction in the scores can also be attributed to scaling and root planing as well as education and motivation of the patient.
Reduction in bleeding on probing was similar in all three sites. This can be attributed to the elimination of local factors with scaling and root planing in Groups A and B respectively, which is in conjunction with Carvalho et al., [9]. Group C, wherein root planing was not performed prior to chip insertion also demonstrated a reduction in sites with bleeding this may be attributed to the disruption of the biofilm following the insertion of the chip resulting in a more favorable clinical status as stated by Jan Cosyn and Iris Wyn [10] and also due to an improvement in the overall oral hygiene status.
The periodontal probe is the most widely used diagnostic tool for the clinical assessment of connective tissue destruction in periodontitis. Increased probing depth and loss of clinical attachment are pathognomic for periodontitis and hence pocket probing is a crucial and mandatory procedure in diagnosing periodontitis and evaluating the success of periodontal therapy.
There was a highly significant reduction in probing pocket depth in the Groups A and B from baseline to 30 days. However, comparatively the reduction in probing depth from 30 days to 3 months was not as significant. This is in accordance with the results of the studies conducted by Jeffcoat et al., [11] Heasman et al., [3].
Group C demonstrated a significant reduction in probing depth from baseline to 30 days, but was not significant from 30 to 90 days. Although, mechanical therapy was not provided at this site, by inserting the chip the biofilm would be disrupted resulting in “a temporary stagnation of the clinical status or even in improvement” Grisi et al., [12].
The intergroup probing depth values when compared between the three groups showed no statistical difference between the groups A and B at three months from baseline. This is in accordance with the results of the studies by Jeffcoat et al., [11] Heasman et al., [3] where significant difference was noted between the groups only at nine months from baseline. The results are also in conjunction with Grisi DC [10] wherein the probing depths at 3,6 and 9 months did not show any significant differences between the control and test groups. Results obtained from another study by Gomes Rodrigues et al., [13] also demonstrated that at six months both treatment groups were equally effective. This is also in accordance with Azmak et al., [14]. However, the findings are not in agreement with Soskolone et al., [8] wherein, statistically significant differences were found between test and control groups at 3 and 6 months. This may be attributed to differences in study design and sample size. A point to be considered is that in both multi-center studies the period of scaling and root planing was confined to a one hour period without administration of local anaesthetic [2,8]. In a study carried out by Badersten et al., in which SRP was carried out with no time limit and under local anaesthesia, sites showed improvements in probing depth and clinical attachment gain greater than those obtained in the controlled pockets. The results are also in conjunction with Carvalho et al., [9] in which the study failed to observe any adjunctive effect of sub gingivally placed chlorhexidine chips in comparison with scaling and root planing. The study has also reiterated the fact that time limitation may have affected the quality of root planing.
In comparison with Group C, both Group A and Group B showed a statistically significant reduction in probing depth. This can be explained by the fact that root planing was not done in this group prior to the insertion of the chip.
In the present study the clinical attachment level values followed a trend similar to probing depth reduction, improvement in attachment levels were observed in all groups when compared with pretreatment values. Therefore when comparisons were made between Group A and Group B the results obtained with SRP plus CHX chip were similar to those obtained with SRP alone; while group C did not achieve values close to either groups.
The results between group A and group B are in accordance with Grisi et al., [12] wherein although the values were not statistically significant the SRP group showed a slightly greater gain in attachment at three and six months. This is also in conjunction with Jeffcoat et al., [11], Heasman et al., [3] where significant difference was noted between the groups only at six months from baseline. The results are also in conjunction with Carvalho et al., [9] in which the study failed to observe any adjunctive effect of subgingivally placed chlorhexidine chips in comparison with scaling and root planing. This is also in accordance with Azmak et al., [14] wherein the chip was once inserted at baseline. Therefore, it is debatable as to whether the changes found in favour of the chip were confined to studies wherein residual test pockets were treated every three months using the chip while the control sites were not exposed to additional therapy.
In Group C, as was the case with probing depth reduction the mean attachment gain showed improvement at 30 and 90 days, although not comparable to Group B and Group A further emphasizing the benefits of conventional treatment modalities.
Conclusion
Based on the findings of this study the chlorhexidine chip did not provide additional benefits beyond that achieved with conventional scaling and root planing after a three month period. However, it should be acknowledged that the chlorhexidine chip by itself did provide clinical benefits although not statistically significant. Although the present study indicated that SRP with or without the placement of the Chlorhexidine chip produced a significant reduction in the probing depth, bleeding on probing and a gain in clinical attachment level, the limitations of the study need to be appreciated. A larger sample size could have been a distinguishing factor in the statistical analysis. Secondly, most investigations on the chip have carried out a double or multiple insertion protocol during the frame of the study; this could influence the final outcome. Therefore a standardization of the dosing schedule would be beneficial.