Primary Ovarian Mucinous Carcinoma with Signet Ring Cells – Report of A Rare Case
Jaya Ganesh P1, Vimal Chander R2, Kanchana M P3, Lakshmi Narasimhan4
1Associate Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Chennai, India.
2Assistant Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Chennai, India.
3Professor, Department of Pathology, Institute of Obstetrics and Gynecology, Chennai, India.
4Professor, Department of Oncology, Institute of Obstetrics and Gynecology, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vimal Chander R, Assistant Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Chennai – 602105, India.
Phone: 09444471905,
E-mail: nalini.kadgi@gmail.com
Presence of signet ring cells in ovarian neoplasms are commonly encountered in Krukenberg tumours of ovary. Unusual presence in primary ovarian mucinous tumours may create a diagnostic difficulty. To the best of our knowledge only very few such cases have been reported in the literature indicating their rarity. We report a case of primary ovarian mucinous carcinoma with signet ring cells. The purpose of this presentation is to sensitize the pathologists to consider primary mucinous carcinoma as a differential diagnosis in tumours with signet ring cells.
Mucinous carcinoma ovary, Signet ring cells
Case Report
A 38-year-old woman presented with abdominal pain and distension for the past three months. Abdominal examination showed a firm mobile mass measuring 18x18 cm in the pelvic region. Per vaginal examination revealed the same mass and per rectal examination showed no deposits in pouch of Douglas. Breast examination was normal. Abdominal ultrasonogram showed a large cystic lesion with solid areas and internal echoes measuring 18.9 x 20.1 cm in the pelvis. Computed tomography of abdomen revealed a malignant abdomino-pelvic cystic mass with internal septations and solid components measuring 20 x 20 cm arising from the right adnexa.Computed tomography using oral and intravenous contrast did not reveal any lesion in the gastrointestinal tract. CA-125 level was 72units/ml. Upper gastrointestinal endoscopy showed features of pangastritis. Patient then underwent total abdominal hysterectomy with bilateral salphingo-oophorectomy and infracolicomentectomy.
Intraoperatively,a cystic lesion in the right ovary containing extensive mucoid material and papillary excrescences in some areas were seen. Liver and spleen were normal. The left ovary, uterus and cervix grossly appeared normal.
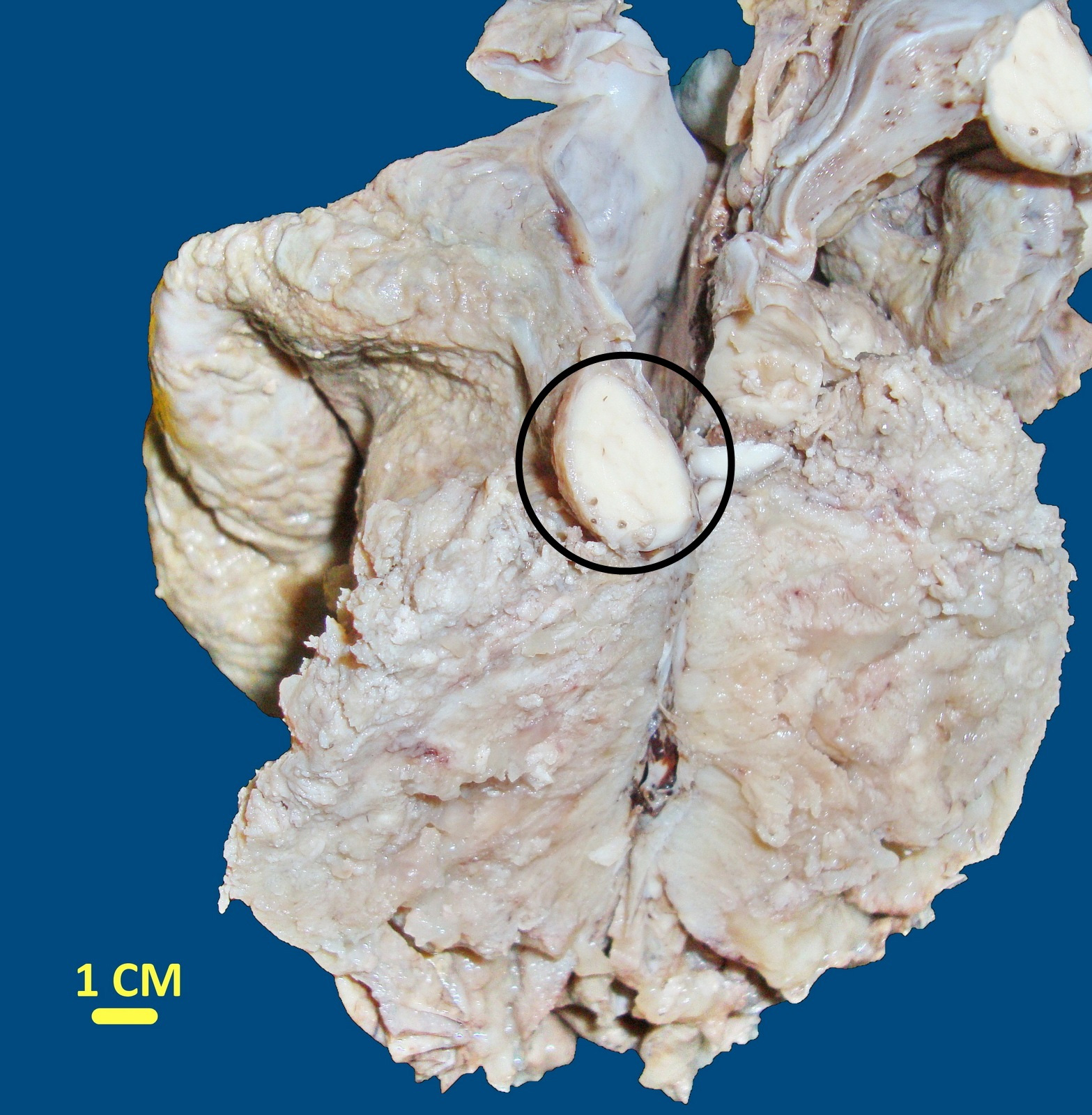
Macroscopically, uterus with cervix measured 8 x 5 x 3 cm. Right ovarian tumours measured 20 x 17 x 17 cm with external surface appearing smooth with focal nodular areas. Cut section showed a solid and cystic tumours with multilocularity and mucoid material within. There were areas showing multiple papillary projections with a whitish solid nodule measuring 3 cm in diameter [Table/Fig-1].
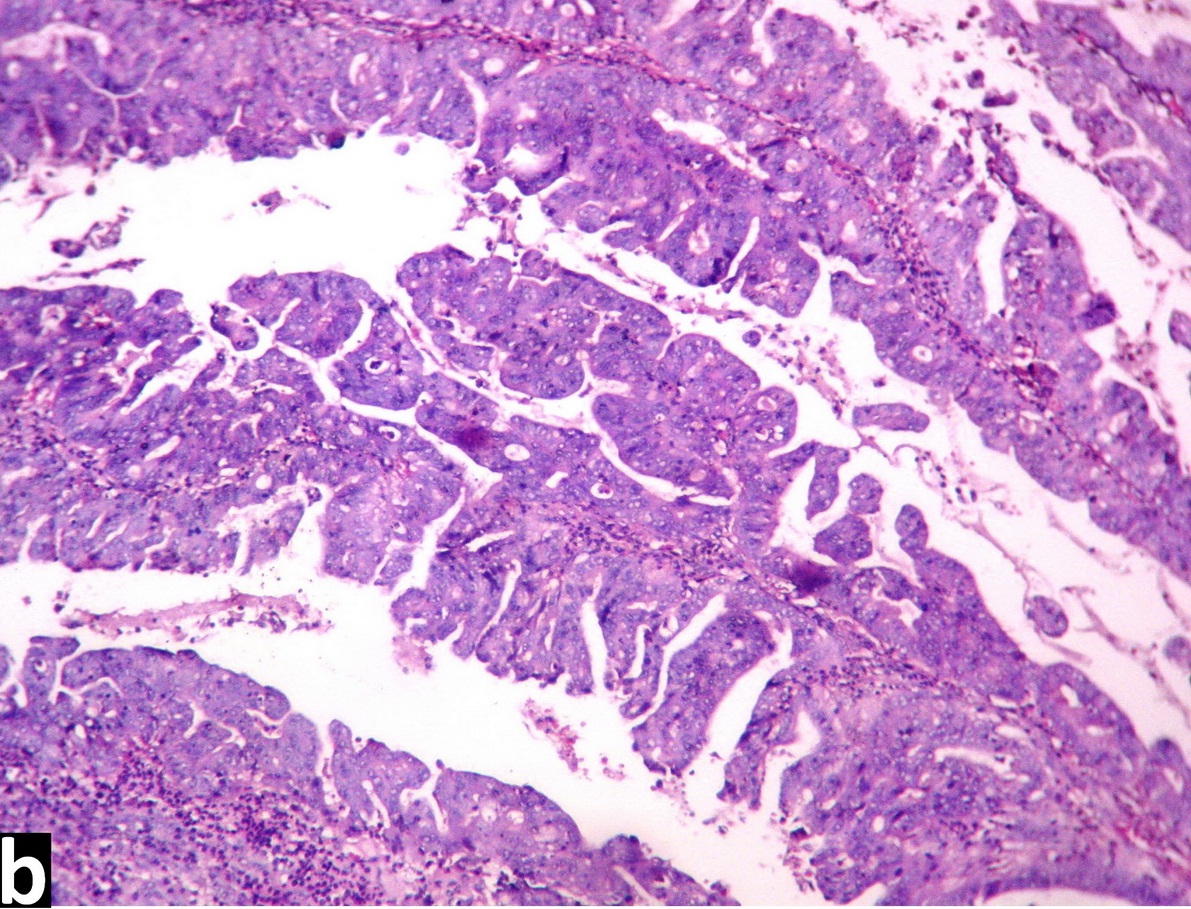
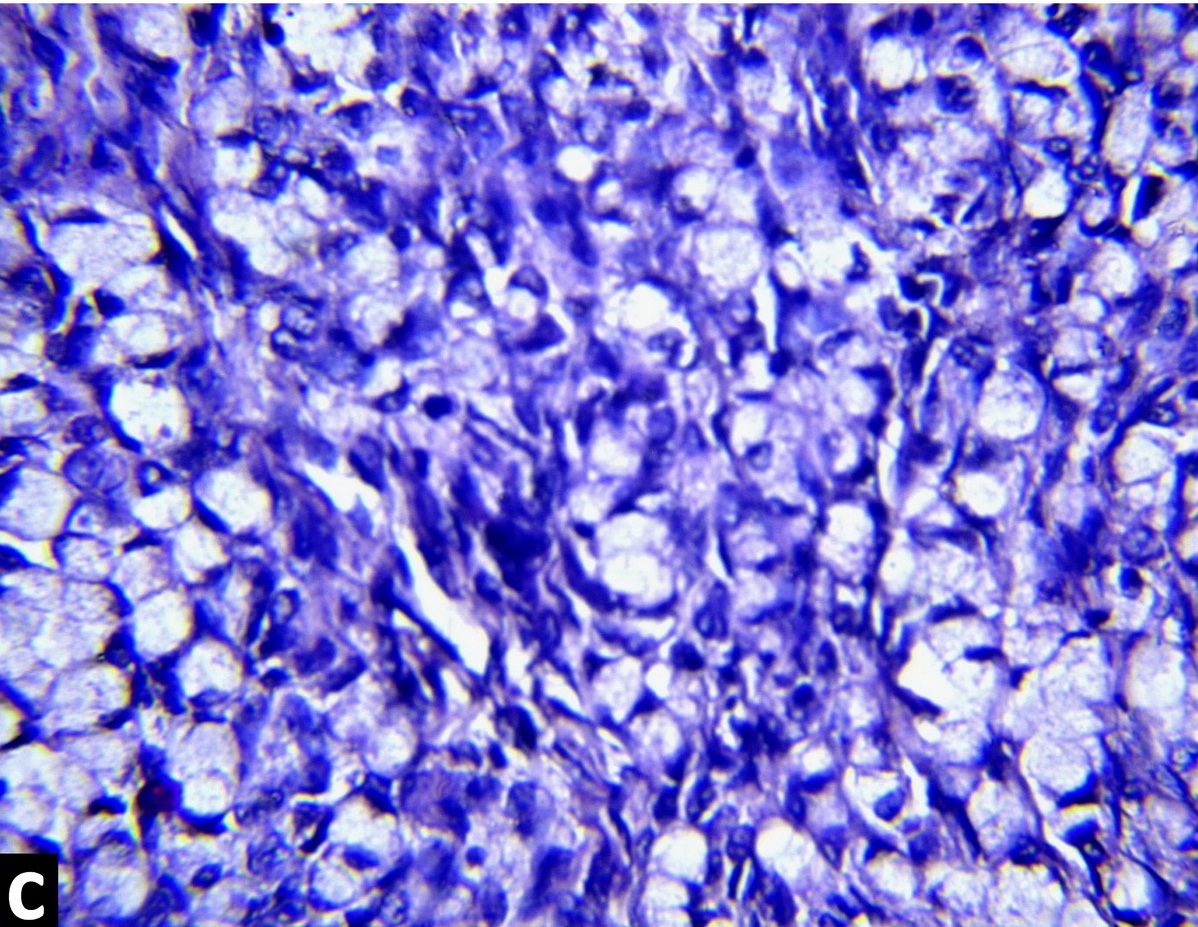
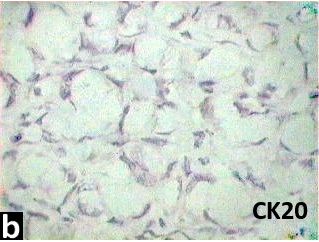
Microscopically, sections showed a neoplasm composed of malignant mucinous epithelial cells arranged in glandular and papillary patterns with evidence of intracellular and extracellular mucin secretion [Table/Fig-2a,2b]. Sections from the solid nodule showed sheets of signet ring cells with scanty intervening stroma [Table/Fig-2c]. Immunostaining showed CK7 positivity and CK20 negativity which confirmed the diagnosis as primary mucinous carcinoma ovary with signet ring cells [Table/Fig-3a,3b]. Cytology of peritoneal fluid was positive for malignancy. A diagnosis of primary ovarian mucinous carcinoma with signet ring cells - stage I C was made. The patient was advised regarding oncologist’s opinion for further management but the patient lost further follow-up.
Gross photograph of the cystic ovarian tumour showing solid whitish nodule
Photomicrograph showing glandular and papillary patterns (H and E x40);
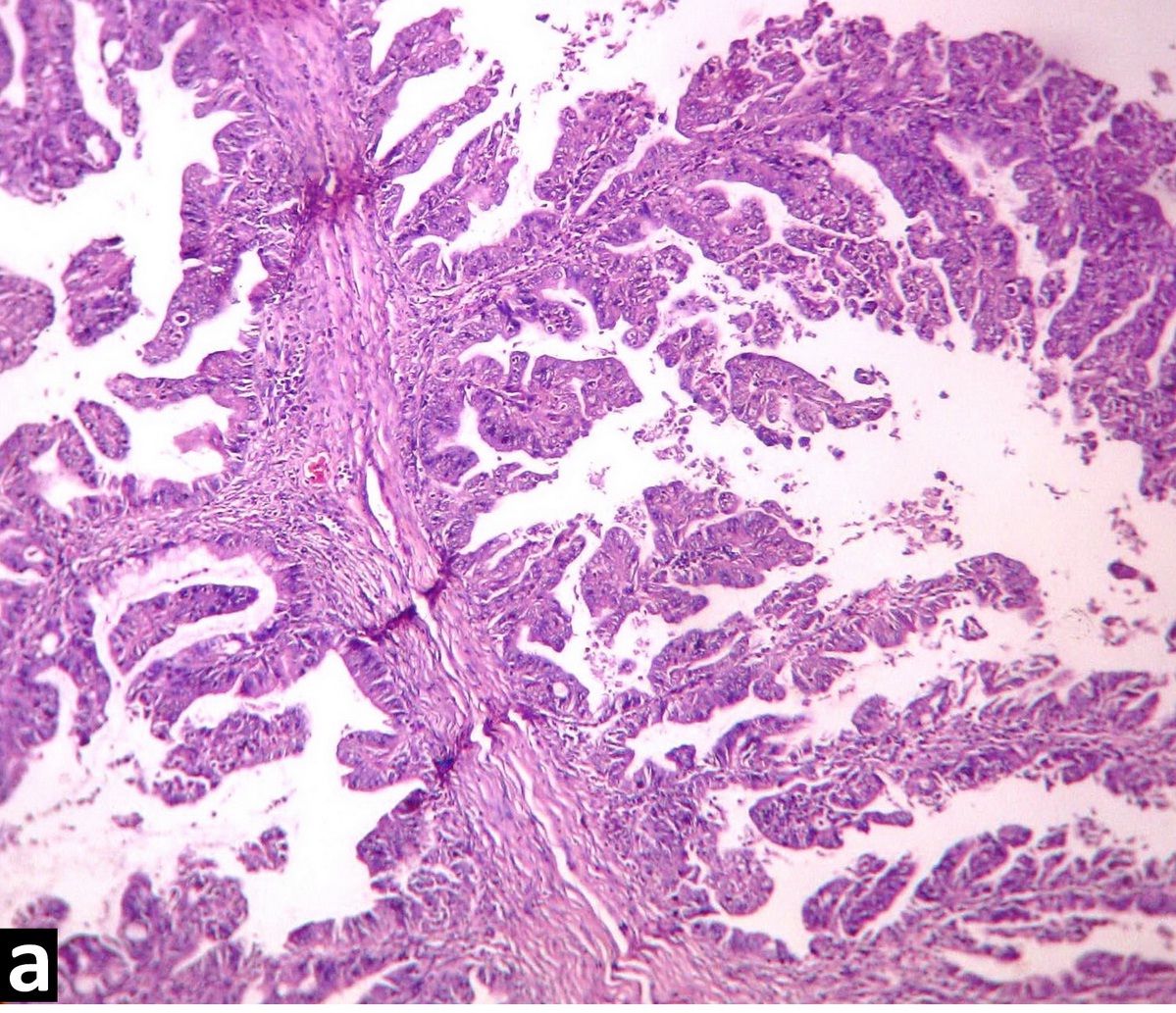
Glandular and papillary patterns (H and E x100);
Sheets of signet ring cells (H and E x400)
CK7 immunostaining showing positivity;

CK20 immunostaining showing negativity
Discussion
Primary ovarian mucinous carcinoma constitutes 2 to 3% of ovarian epithelial neoplasms [1]. Out of 145 ovarian mucinous tumours in this institute during the last five years, majority were benign mucinous cyst adenoma (111cases). 21 cases were mucinous carcinoma and 13 were borderline mucinous tumours. Metastatic tumours comprised 6 cases. This was the first case of primary ovarian mucinous carcinoma with signet ring cells reported in this institute. Signet ring cells exclusively seen in Krukenberg tumours has been reported in only three cases of primary ovarian mucinous carcinoma in the recent review of literature [2]. Presence of unexpected signet ring cells in a primary ovarian mucinous carcinoma can create a great diagnostic difficulty. The presence of signet ring cells in primary ovarian tumours and the proliferation of such cells mimicking the metastatic signet ring cell carcinoma has long been a topic of discussion [3]. Presence of signet ring cells in an ovarian mucinous carcinoma is mostly suggestive of a metastatic neoplasm, the most likely primary sites being in the gastrointestinal tract [4,5]. Presence of signet ring cells is one of the main features in a mucinous ovarian carcinoma which strongly favours a metastatic rather than a primary neoplasm. The features suggestive of a secondary mucinous neoplasm, in addition to the signet ring cells, include bilaterality, small size, destructive stromal invasion, microscopic stromal involvement, tumour cells floating in mucin, single cell stromal invasion and extensive lymphovascular invasion [6].
In this case, unilaterality, malignant glands in a fibrous stroma, absence of surface implants, large size and absence of lymphovascular invasion favours a primary mucinous carcinoma rather than a metastatic tumour. Immunohistochemistry,though of limited value in distinguishing between primary and secondary mucinous carcinoma in the ovary, can be considered as an additional point favouring the diagnosis.
Primary ovarian mucinous carcinomas express CK20, CA19.9, Carcinoembryonic antigen and CDX2 at least focally, although they typically retain their diffuse CK7 positivity [7,8]. In the present case, diffuse CK7 positivity and CK20 negativity favours more a primary ovarian mucinous carcinoma rather than a metastatic tumour.
There have been several reports especially in the older literature of primary ovarian mucinous carcinoma with signet ring cells, the so called primary Krukenberg tumour [3]. The main argument against accepting the entity of primary ovarian Krukenberg tumour is the possibility of missing a small occult primary neoplasm in an organ like stomach.
Conclusion
The designation of primary ovarian Krukenberg tumour should not be used for a neoplasm like primary ovarian mucinous carcinoma with signet ring cells but rather they should be classified according to the underlying background neoplasm with a special note concerning the signet ring cell component. This case is presented to sensitize the pathologists to consider primary mucinous carcinoma as a differential diagnosis in cases of ovarian tumours with signet ring cells.
[1]. JD Seidman, KR Cho, BM Ronnett, RJ Kurman, Surface Epithelial Tumours of the Ovary. In: Kurman RJ. Blausteins pathology of female genital tract 2010 17th EditionNew YorkSpringer.:745-9. [Google Scholar]
[2]. S El-Safadi, U Stahl, HR Tinneberg, A Hackethal, K Muenstedt, Primary signet ring cell mucinous ovarian carcinoma: a case report and literature reviewCase Rep Oncol. 2010 3:451-7. [Google Scholar]
[3]. WG McCluggage, RH Young, Primary ovarian mucinous tumours with signet ring cells: report of 3 cases with discussion of so-called primary Krukenberg tumourAm J SurgPathol 2008 32:1373-9. [Google Scholar]
[4]. T Kiyokawa, RH Young, RE Scully, Krukenberg tumours of the ovary: a clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestations.Am J SurgPathol. 2006 30:277-99. [Google Scholar]
[5]. RH Young, From Krukenberg to today: the ever present problems posed by metastatic tumours in the ovary: Part I. Historical perspective, general principles, mucinous tumours including the Krukenberg tumourAdv Anat Pathol 2006 13(5):205-27. [Google Scholar]
[6]. JD Seidman, RJ Kurman, BM Ronnett, Primary and metastatic mucinous adenocarcinomas in the ovaries: incidence in routine practice with a new approach to improve intraoperative diagnosis.Am J Surg Pathol. 2003 27:985-93. [Google Scholar]
[7]. WG Mc Cluggage, RH Young, Immunohistochemistry as a diagnostic aid in the evaluation of ovarian tumours.Semin Diagn Pathol 2005 22:3-32. [Google Scholar]
[8]. SY Park, HS Kim, EK Hong, WH Kim, Expression of cytokeratins 7 and 20 in primary carcinomas of the stomach and colorectum and their value in the differential diagnosis of metastatic carcinomas to the ovaryHum Pathol. 2002 33:1078-85. [Google Scholar]