Introduction
The latest KDIGO 2013 guidelines define Chronic kidney disease (CKD) by the presence of kidney damage or decreased kidney function (GFR) for three or more months, irrespective of the cause [1] [Table/Fig-1]. The term End Stage Renal Disease (ESRD) is used to refer to a chronic kidney disease which requires renal replacement therapy. This term came up with the widespread use of KDOQI guidelines introduced in 2002 [2]. These staged CKD into five categories [3] [Table/Fig-2]. ESRD was defined as CKD stage 5 requiring dialysis [3]. However the latest KDIGO guidelines suggest that dialysis be initiated when one or more of the following are present: symptoms or signs attributable to kidney failure (serositis, acid-base or electrolyte abnormalities, pruritus); inability to control volume status or blood pressure; a progressive deterioration in nutritional status refractory to dietary intervention; or cognitive impairment [1].The KDIGO staging of CKD is different from the KDOQI staging and it is worthwhile to have a look at it [Table/Fig-3].Hypotension is the most common complication observed in dialysis patients [4] and is observed in 15-50% of the cases [5]. The other complications include muscle cramps, itching, fever, chills, pyrogen reactions, disequilibrium syndrome, nausea and vomiting, itching, headache and hypertension [6].
Criteria for diagnosis of chronic kidney disease [3]
| Markers of Kidney Damage (One or more) | Albuminuria (AER<30mg/24 hours; ACR<30mg/g [=3mg/mmol] Urine sediment abnormalities Electrolyte and other abnormalities due to tubular disorders Abnormalities detected by histology Structural abnormalities detected by imaging History of kidney transplantation |
| Decreased GFR | GFR<60ml/min/1.73m2 (GFR categories G3a–G5) |
KDOQI Guidelines for staging of CKD [3]
| CKD Stage | GFR |
|---|
| Stage 1 | >90 |
| Stage 2 | 60-89 |
| Stage 3 | 30-59 |
| Stage 4 | 15-29 |
| Stage 5 | <15 |
KDIGO guidelines for CKD classification [1]
| GFR STAGE | GFR (mL/min/1.73 m2) |
|---|
| G1 | >90 |
| G2 | 60-89 |
| G3a | 45-59 |
| G3B | 30-44 |
| G4 | 15-29 |
| G5 | <15 |
| ALBUMINURIA STAGE | AER (mg/day) |
| A1 | <30 |
| A2 | 30-300 |
| A3 | >300 |
Low risk =G1A1, G2A1
Moderately increased risk=G1A2, G2A2, G3aA1
High risk=G3A1, G3A2, G3bA1, G3aA2
Very high risk =G4A1, G5A1, G3bA2, G4A2, G5A2,G3aA3, G3bA3, G4A3, G5A3
Hypertension in Dialysis Patients
It is a known fact that the presence of hypertension in the population is directly proportional to cardiovascular morbidity and mortality [7]. However it is surprising and interesting to know that CKD patients demonstrate what is known as an ‘inverse epidemiology’ [8,9]. Higher longevity of hypertensive patients receiving dialysis has been noted in many studies [10]. Both higher and lower blood pressures have been found to be detrimental in these group of patients and therefore recommendations to achieve a target blood pressure have been set forth. `However there are no strict guidelines and they vary from patient to patient [11].
How to measure Blood Pressure in dialysis patients. In a US study on 2535 hemodialysis patients, 86% were found to be suffering from hypertension. Even in those patients who received antihypertensive medications, 58% had poorly controlled Blood Pressure and 12% had refractory hypertension [12].The bloodpressure in these patients can be assessed by taking blood pressures pre-dialysis, during dialysis and post-dialysis. In most cases, the pre-dialysis and post-dialysis systolic blood pressure are found to be 10 mm Hg more and 10 mm Hg less than the interdialytic blood pressure respectively [13]. The other way is to educate the patient to routinely measure blood pressure at home, and look for a composite reading over 1-2 weeks [14,15]. But by far the best way to monitor the blood pressure in these patients would be at home by the patient by an automatic ambulatory blood pressure monitoring [16,17].
Target Blood Pressure
Till now there have been no randomized prospective trials evaluating the target blood pressure in dialysis patients.Some studies suggest that the goal of bloodpressure be a pre-dialysis value of below 140/90 mmHg and a post-dialysis value of 130/80 mmHg [18–23].In patients undergoing dialysis; a normal blood pressure may be defined as the mean ambulatory blood pressure less than 135/85 mmHg during the day and less than 120/80 mmHg by night. Some studies have postulated keeping the systemic blood pressure low leads to enhanced mortality so a J or U shaped curve has been observed [19,24–27].
Hypertension: protective or not: Effect on morbidity and mortality
Fifty percent deaths in CKD stage 5 patients are found to be from cardiovascular diseases [28]. The complications from CKD such as anemia, hyperhomocysteinemia, hyperparathyroidism, oxidative stress, hypoalbuminemia, chronic inflammation, prothrombotic factors are all responsible for high morbidity and mortality in these group of patients. Furthermore, in patients who receive dialysis, there is higher risk of cardiovascular diseases and mortality than the general population. Patients who receive renal transplantation have been shown to have improved cardiovascular survival [29]. When studying the effect of high blood pressures, 50 to 60 percent of the patients on hemodialysis are hypertensive and the value can be as high as 85 % as seen in various studies [12,30,31]. Persistent hypertension reflects imperfect volume control despite initiation of dialysis [12,31–33].
Lower blood pressures (pre dialysis systolic Blood Pressure <110 mm Hg) was found to be associated with higher mortality whereas higher blood pressures (pre dialysis systolic Blood Pressure 150-159) have also been reported to have higher mortality [9,26]. Kalantar-Zadeh et al., studied a cohort of 40,933 hemodialysis patients for a 15 months period and found that the hazard ratio was 1.60 in the patients with pre-dialysis systolic blood pressure <110 mmhg and pre-dialysis diastolic blood pressures <50 mmHg was 2.00 [8]. Another study in 16,939 patients followed for 1-2 years found an increased mortality with a systolic blood pressure greater than 150 mm Hg [34]. Another retrospective study in peritoneal dialysis patients found that higher blood pressures were protective [35].
Pathophysiology
Concept of Dry Weight : DW is the post-dialysis weight in which the patient remains normotensive without antihypertensive medication until the next dialysis [36], or as that body weight at the end of dialysis below which further reduction results in hypotension [37]. Dry weight is measured by biochemical markers, bioimpedence analysis, bioimpedence spectroscopy, and vena caval diameter. Biochemical markers include cyclic guanidine monophosphate and ANP. Chronic kidney disease is a catabolic state and is associated with progressive nephron destruction. The progressive nephron loss causes extra cellular volume enlargement and sodium retention. This leads to weight gain but paradoxical reduction in lean body mass.
Hypervolemia occurs in chronic renal disease because of decrease in GFR, which results in positive sodium balance and extracellular fluid expansion. This is coupled with excessive dietary sodium and fluid intake. There is also secretion of ouabain like inhibitors of Na-K ATPases, which lead to elevation of intracellular calcium; causing increase in vascular resistance [38].
Other causes include renin angiotensin system overactivity. It occurs due to regional renal ischemia and scarring due to CKD which consequently causes increased renin release; further increasing systemic vascular resistance. Increased sympathetic activity, due to increased levels of Angiotensin 2; also plays important role by increasing vascular resistance and systemic Blood Pressure. It is also attributed to asymmetric dimethyl arginine; the role of which is not properly understood [39–41]. The other implicated factors include uremia,endothelin-1, administration of erythropoietin for the treatment of anemia of chronic kidney disease, hyperparathyroidism and increased pulse pressure. Uremia due to the Chronic Kidney disease causes a neural reflex which stimulates cardiovascular centers in brainstem. Endothelin-1; a potent vasoconstrictor; accumulates as a result of decreased renal clearance. Erythropoeitin administered subcutaneously in chronic anemia is known to increase blood pressure by 10 mm Hg in patients with chronic renal failure [42]. Hyperparathyroidism is another cause of increase Blood Pressure in patients with CKD. Calcification of arterial tree causes an increase in vascular resistance, causing increased pulse pressure, which also has an important role in pathogenesis of hypertension.
Management
The management is centered on the control of volume status, lifestyle modification, dialysis and antihypertensive agents.
Lifestyle modifications include weight reduction to achieve dry weight, salt and fluid restriction and adherence to strict salt diet (1000-1500 mg salt/day) [43]. Physical exercise decreases blood pressure, reduces peripheral vessel resistance and reduces vessel rigidity [Table/Fig-4]. Alcohol abuse as documented by MAST study (Michigan Alcohol Screening test); which studies the effect of alcoholism in patients undergoing hemodialysis found that alcohol abuse was associated with lower serum albumin levels and increased dialysis dependence so alcohol abuse must be adequately treated [44,45].
Management algorithm (KDOQI Guidelines) [3]
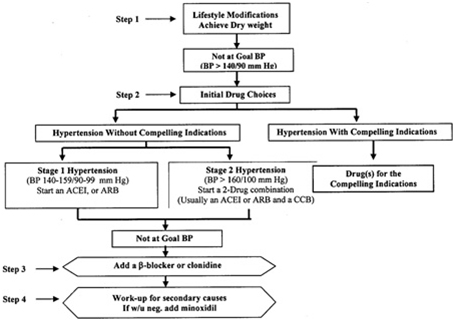
If during the interdialytic period blood pressure remain normal and it does not exceed 160/95 mmHg immediately before the next dialysis session, it is reasonable to keep antihypertensive therapy withheld [45]. Diuretics are not commonly used because of lack of efficacy. The choice of antihypertensive depends upon the coexsisting comorbidities, patient demographic characterstics, risk profile and lifestyle [45–48]. The K/DOQI guidelines suggest that the ACE inhibitors or angiotensin II receptor blockers provide greater benefits in terms of reducing left ventricular mass [49]. A recent observational study stated that there was no significant blood pressure eduction between the treated and untreated groups on ACE inhibitors. However in the treated patients, the mortality was significantly decreased with a risk reduction of 52%.The postulated mechanism of action maybe reducing the mean arterial pressure, pulse wave velocity and aortic systolic pressure and left ventricular hypertrophy.The adverse effects include hyperkalemia due to inhibition of excretion of potassium in the colon or cellular uptake of potassium [50]. However more evidence is required that ACE inhibitors decrease mortality among chronic haemodialysis patients and younger patients as well [49].
Recommendation from the KDOQI also suggest that the large interdialytic weight gains should be discouraged which can be accomplished by low sodium intake, increased dialysis treatments [49]. Other interventions include the fixed lower dialysate sodium concentration in combination with dietary salt restriction will help in controlling hypertension [51].
In cases of refractory hypertension,minoxidil may be effective. However bilateral nephrectomy may be considered in the rare non compliant individual with life threatening hypertension, this can be seen in a study in which it was found that after nephrectomy the diastolic blood pressure dropped to less than 90 mm Hg ; 3 to 6 months after nephrectomy [52]. Refractory hypertension may be observed due to altered nitric oxide/endothelin-1 balance and/or endothelial dysfunction [53]. The drug carvedilol may be effective in this setting to decrease the blood pressure, as suggested by a pilot study done in a 12 week period in which initiation of carvedilol titrated to 50 mg twice daily was associated with a decrease in the frequency of intradialytic hypertensive episodes from 77 to 28 percent .
Conclusion
The most important management strategy in these patients is the attainment of dry weight. A combination of lifestyle changes, antihypertensives and management of the comorbidities is to be achieved. The lack of any cardiovascular events until blood pressure reaches 180 mm Hg is puzzling. Poor ventricular function in patients with lower blood pressure may be the cause of higher mortality, whereas higher risk hypertensive patients may not have survived to enter the study thus leading to a survival bias.
Low risk =G1A1, G2A1Moderately increased risk=G1A2, G2A2, G3aA1High risk=G3A1, G3A2, G3bA1, G3aA2Very high risk =G4A1, G5A1, G3bA2, G4A2, G5A2,G3aA3, G3bA3, G4A3, G5A3
[1]. KDIGO. Chapter 1: Definition and classification of CKD. Kidney Int Suppl 2013; 3:19. http://www.kdigo.org/clinical_practice_guidelines/pdf/CKD/KDIGO_2012_CKD_GL.pdf [Google Scholar]
[2]. Eckardt KU, Berns JS, Rocco MV, Kasiske BL, Definition and classification ofCKD: the debate should be about patient prognosis--a position statement from KDOQI and KDIGOAm J Kidney Dis 2009 53(6):915-20.doi:10.1053/j.ajkd.2009.04.001. Epub 2009 May 5. PubMed PMID: 19406541 [Google Scholar]
[3]. National Kidney FoundationK/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAm J Kidney Dis 2002 39:S1 [Google Scholar]
[4]. Cases A, Coll E, Chronic hypotension in the dialysis patientJ Nephrol 2002 15(4):331-5.Review. PubMed PMID: 12243360 [Google Scholar]
[5]. Orofino L, Marcén R, Quereda C, Epidemiology of symptomatic hypotension in hemodialysis: is cool dialysate beneficial for all patients?Am J Nephrol 1990 10:177 [Google Scholar]
[6]. Bregman H, Daugirdas JT, Ing TS, Complications during hemodialysisIn: Handbook of Dialysis, Dauugirdas JT, Ing TS (Eds) 1994 New YorkLittle, Brown:149 [Google Scholar]
[7]. Lewington S, Clarke R, Qizilbash N, Age-specific relevance of usual blood pressure to vascular mortality: Ameta-analysis of individual data for one million adults in 61 prospective studiesLancet 2002 360:1903-13. [Google Scholar]
[8]. Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: The 58th annualfall conference and scientific sessionsHypertension 2005 45:811-17. [Google Scholar]
[9]. Zager PG, Nikolic J, Brown RH, “U” curve association of blood pressure and mortality in hemodialysis patients. Medical Directors of Dialysis Clinic, Inc [pub-lished erratum appears in Kidney Int 1998; 54(4):1417]Kidney Int 1998 54:561-69. [Google Scholar]
[10]. Udayaraj UP, Steenkamp R, Caskey FJ, Blood pressure and mortality risk on peritoneal dialysisAm J Kidney Dis 2009 53:70 [Google Scholar]
[11]. K/DOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis PatientsAm J Kidney Dis 2005 45(Suppl 3):S49 [Google Scholar]
[12]. Agarwal R, Nissenson AR, Batlle D, Prevalence,treatment, and control of hypertension in chronic hemodialysis patients in the United StatesAm J Med 2003 115:291-97. [Google Scholar]
[13]. Coomer RW, Schulman G, Breyer JA, Shyr Y, Ambulatory blood pressure monitoring in dialysis patients and estimation of mean interdialytic blood pressureAm J Kidney Dis 1997 29:678 [Google Scholar]
[14]. Tripepi G, Fagugli RM, Dattolo P, Prognostic value of 24-hour ambulatory blood pressure monitoring and of night/day ratioinnondiabetic, cardiovascular events-free hemodialysis patientsKidneyInt 2005 68:1294-302. [Google Scholar]
[15]. Zoccali C, Tripepi G, Ambulatory monitoring and clinic Blood Pressure measurements for predicting left ventricular mass in patients withchronic renal diseasesNephrol Dial Transplant 1999 14:240-1. [Google Scholar]
[16]. Alborzi P, Patel N, Agarwal R, Home blood pressures are of greater prognostic value than hemodialysis unit recordingsClin J Am SocNephrol 2007 2:1228 [Google Scholar]
[17]. Agarwal R, Andersen MJ, Bishu K, Saha C, Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patientsKidney Int 2006 69:900 [Google Scholar]
[18]. Tozawa M, Iseki K, Iseki C, Takishita S, Pulse pressure and risk of total mortality and cardiovascular events in patients on chronic hemodialysisKidney Int 2002 61:717 [Google Scholar]
[19]. Tentori F, Hunt WC, Rohrscheib M, Which targets in clinical practice guidelines are associated with improved survival in a large dialysis organization?J Am SocNephrol 2007 18:2377 [Google Scholar]
[20]. Covic A, Goldsmith DJ, Venning MC, Ackrill P, Long-hours home haemodialysis--the best renal replacement therapy method?QJM 1999 92:251 [Google Scholar]
[21]. Converse RL Jr, Jacobsen TN, Toto RD, Sympathetic overactivity in patients with chronic renal failureN Engl J Med 1992 327:1912 [Google Scholar]
[22]. Agarwal R, Systolic hypertension in hemodialysis patientsSemin Dial 2003 16:208 [Google Scholar]
[23]. K/DOQI Clinical Practice Guidelines and Clinical Practice Recommendations 2006 Updates Hemodialysis adequacy Peritoneal Dialysis Adequacy Vascular AccessAm J Kidney Dis 2006 48(Suppl 1):S1 [Google Scholar]
[24]. Port FK, Hulbert-Shearon TE, Wolfe RA, Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patientsAm J Kidney Dis 1999 33:507 [Google Scholar]
[25]. Schömig M, Eisenhardt A, Ritz E, Controversy on optimal blood pressure on haemodialysis: normotensive blood pressure values are essential for survivalNephrol Dial Transplant 2001 16:469 [Google Scholar]
[26]. Port FK, Hulbert-Shearon TE, Wolfe RA, Predialysis bloodpressure and mortality risk in a national sample of maintenance hemodialysis patientsAm J Kidney Dis 1999 33:507-17. [Google Scholar]
[27]. Li Z, Lacson E Jr, Lowrie EG, The epidemiology of systolic blood pressure and death risk in hemodialysis patientsAm J Kidney Dis 2006 48:606 [Google Scholar]
[28]. Rocco MV, Yan G, Gassman J, Comparison of causes ofdeath using HEMO Study and HCFA end-stage renal disease death notification classification systems. The National Institutes of Health-funded Hemodialysis. Health Care Financing AdministrationAm J Kidney Dis 2002 39:146-53. [Google Scholar]
[29]. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patientsAm J Kidney Dis 2005 45:S1-153. [Google Scholar]
[30]. HCFA-1995. 1995 Annual Report. ESRD core indicators project. Opportunities to improve care for adult in-center hemodialysis patients. Baltimore, MD, Health Care Financing Administration, DHHS, January 1996 [Google Scholar]
[31]. Rahman M, Dixit A, Donley V, Factors associated with inadequate blood pressure control in hypertensive hemodialysis patientsAm J Kidney Dis 1999 33:498 [Google Scholar]
[32]. Zucchelli P, Santoro A, Zuccala A, Genesis and control of hypertension in hemodialysis patientsSemin Nephrol 1988 8:163 [Google Scholar]
[33]. Rahman M, Fu P, Sehgal AR, Smith MC, Interdialytic weight gain, compliance with dialysis regimen, and age are independent predictors of blood pressure in hemodialysis patientsAm J Kidney Dis 2000 35:257 [Google Scholar]
[34]. Stidley CA, Hunt WC, Tentori F, Changing relationship of blood pressure with mortality over time among hemodialysis patientsJ Am SocNephrol 2006 17:513-20. [Google Scholar]
[35]. Sankaranarayanan N, Santos SF, Peixoto AJ, Blood pressure measurement in dialysis patientsAdv Chronic Kidney Dis 2004 11:134-42. [Google Scholar]
[36]. Charra B, Laurent G, Chazot C, Clinical assessment of dry weightNephrol Dial Transplant 1996 11(Suppl 2):16-19. [Google Scholar]
[37]. Campese VM TA, Hypertension in dialysis patients 2004 PhiladelphiaLippincott Williams & Wilkins [Google Scholar]
[38]. Santos SF, Peixoto AJ, Hypertension in dialysisCurr Opin Nephrol Hypertens 2005 14:111-8. [Google Scholar]
[39]. Yoshino M, Kuhlmann MK, Kotanko P, International differences in dialysis mortality reflect background general population atherosclerotic cardiovascular mortalityJ Am SocNephrol 2006 17:3510-19. [Google Scholar]
[40]. Lozano A, Benavides B, Quiros P, Control of arterial hypertensionby means of a regimen of hemodialysis on alternate days(HDAA or EODD: “Every Other Day Dialysis”) versus 2 conventionalregiments of 4 and 5 hours per session 3 times a week with72 hours without sessions during the weekendsNefrologia 2006 26:695-702. [Google Scholar]
[41]. Augustyniak RA, Tuncel M, Zhang W, Sympathetic overactivity as a cause of hypertension in chronic renal failureJ Hypertens 2002 20(1):3-9. [Google Scholar]
[42]. Hamburger RJ, Christ PG, Morris PA, Hypertension in dialysis patients: does CAPD provide an advantage?AdvPerit Dial 1989 5:91-6. [Google Scholar]
[43]. Ahmad S, Dietary sodium restriction for hypertension in dialysis patientsSemin Dial 2004 17:284-7. [Google Scholar]
[44]. Hegde A, Veis JH, Seidman A, High prevalence of alcoholism in dialysis patientsAm J Kidney Dis 2000 35:1039-43. [Google Scholar]
[45]. Gueye AS, Chelamcharla M, Baird BC, The association between recipient alcohol dependency and long-term graft and recipient survivalNephrol Dial Transplant 2007 22:891-8. [Google Scholar]
[46]. Kalantar-Zadeh K, Kopple JD, Obesity paradox in patients on maintenance dialysisContrib Nephrol 2006 151:57-69. [Google Scholar]
[47]. Fishbane S, Natke E, Maesaka JK, Role of volume overload in dialysis-refractory hypertensionAm J Kidney Dis 1996 28:257-61. [Google Scholar]
[48]. Horl MP, Horl WH, Drug therapy for hypertension in hemodialysis patientsSemin Dial 2004 17:288-94. [Google Scholar]
[49]. Efrati S, Zaidenstein R, Dishy V, ACE inhibitors and survival of hemodialysis patientsAm J Kidney Dis 2002 40:1023-9. [Google Scholar]
[50]. Knoll GA, Sahgal A, Nair RC, Renin-angiotensin system blockade and the risk of hyperkalemia in chronic hemodialysis patientsAm J Med 2002 112:110-14. [Google Scholar]
[51]. Krautzig S, Janssen U, Koch KM, Dietary salt restriction and reduction of dialysate sodium to control hypertension in maintenance haemodialysis patientsNephrol Dial Transplant 1998 13:552 [Google Scholar]
[52]. Zazgornik J, Biesenbach G, Janko O, Bilateral nephrectomy: the best, but often overlooked, treatment for refractory hypertension in hemodialysis patientsAm J Hypertens 1998 11:1364 [Google Scholar]
[53]. Chou KJ, Lee PT, Chen CL, Physiological changes during hemodialysis in patients with intradialysis hypertensionKidney Int 2006 69:1833 [Google Scholar]