Acanthamoeba Detection in the Anterior Chamber after Therapeutic Penetrating Keratoplasty
RK Agarwal1, Garima Mittal2, Anuradha Raj3, Shalini Gupta4
1Professor and HOD, Department of Microbiology, Himalayan Institute of Medical Sciences Jolly Grant, Dehradun, (Uttarakhand), India.
2Assistant Professor, Department of Microbiology, Himalayan Institute of Medical Sciences Jolly Grant, Dehradun, (Uttarakhand), India.
3Assistant Professor,Department of Ophthalmology, Himalayan Institute of Medical Sciences Jolly Grant, Dehradun, (Uttarakhand), India.
4Junior Resident, Department of Microbiology, Himalayan Institute of Medical Sciences Jolly Grant, Dehradun, (Uttarakhand), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Garima Mittal, Assistant Professor Department of Microbiology, Himalayan Institute of Medical Sciences, HIHT University, Swami Ram Nagar, Jolly Grant, P.O. Doiwala, Dehradun (Uttarakhand)-248140, India.
Phone: 0091-135-2471577; 0091-9759075607,
E-mail: garimamittal80@gmail.com
Acanthamoeba infection has been recognized in almost all parts of the world. With most of the literature focusing on contact lens related Acanthamoeba keratitis, ophthalmologists may hesitate to diagnose this entity in patients without lenses. We report the case of a patient with Acanthamoeba infection of the anterior chamber, unrelated to contact lens wear, diagnosed by examination of aqueous tap following penetrating therapeutic keratoplasty.
Acanthamoeba, Aqueous tap, Corneal ulceration, Keratitis
Case Report
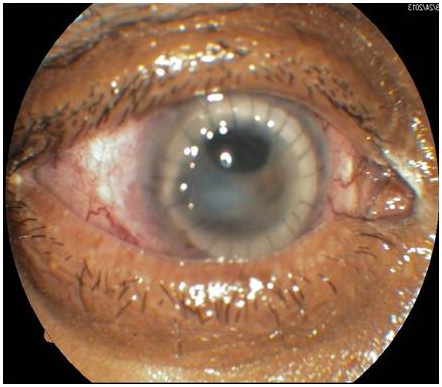
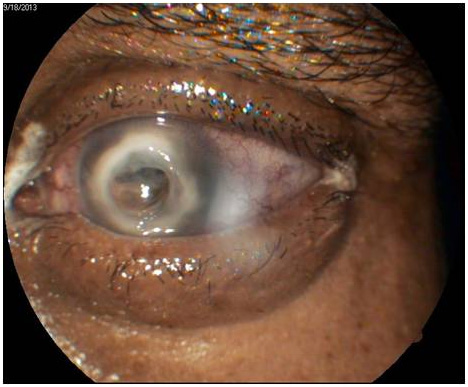
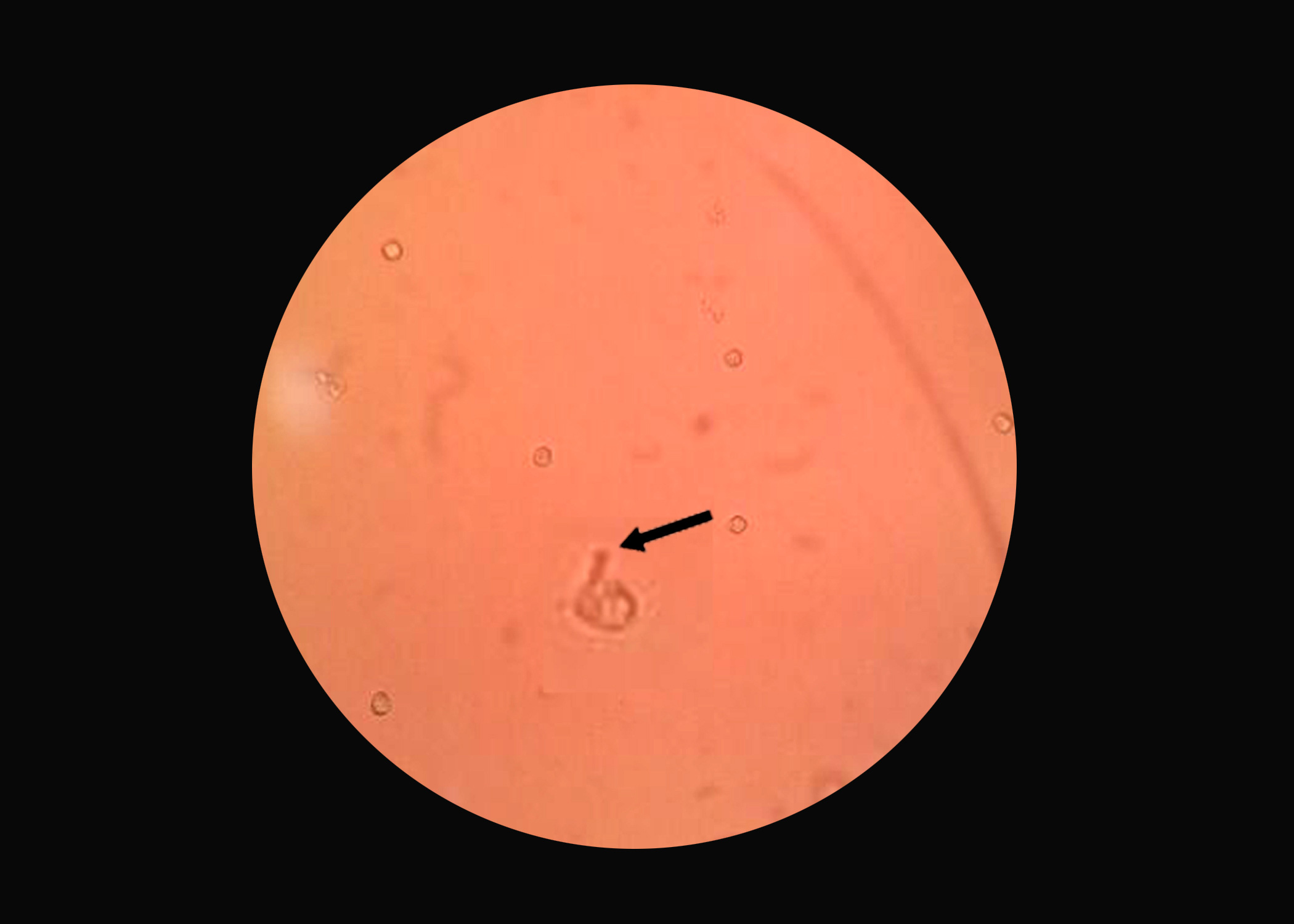
A 35-year-old male presented to the outpatient department of ophthalmology of a tertiary care hospital, Dehradun, India in December 2013, with complaints of pain, redness of eye, diminution of vision and photophobia, which was preceded by injury with a stone, one and a half month ago. He was treated by a local practitioner with topical antibiotic drops, ciprofloxacin 0.3%. Family history, past history and contact lens wear history was unremarkable. On examination his visual acuity was 6/6 for right eye and hand movements close to face for left eye. On examination there was a corneal perforation about 4x5mm at the centre of cornea. The area of perforation was surrounded by deep stromal infiltrates [Table/Fig-1]. Anterior chamber was flat. There was an area of ciliary staphyloma at about 11-1`0 clock position. Therapeutic penetrating keratoplasty was done. The corneal button of recipient showed no organism in Gram`s stain and KOH mount. Bacterial culture also did not reveal any organism. On fifth postoperative day, he was discharged from the hospital with healthy graft and clear anterior chamber [Table/Fig-2]. On tenth post-operative day he came back to outpatient department with graft edema, graft ectasia and exudates in anterior chamber. Anterior chamber tap of 0.1 ml was taken and sent for Gram`s stain and KOH mount which were negative for any finding. However on wet mount, trophozoites with thorny appearance showing tapering pseudopodia were seen measuring around 20-40 μm in size which moved slowly without any direction consistent with Acanthamoeba as shown in [Table/Fig-3]. Sample was also cultured on non-nutrient agar spread with lawn of gram negative bacteria i.e E. coli. Culture plate was incubated at 300C. Cultures were checked under light microscope and tyre like tracks were seen indicating migration of Acanthamoeba. Patient was started on topical voriconazole, oral prednisolone, tobramycin and cycloplegic eye drops. One month after continuing treatment, visual acuity of the patient improved up to counting finger 2 metres. Oral predinisolone was tapered successfully. Exudates in the anterior chamber cleared with graft clarity of grade 2. The graft remained clear with no evidence of recurrence at 3 months.
Corneal perforation surrounded by deep stromal infiltrates
Clear anterior chamber, on fifth postoperative day
Wet mount showing Acanthamoeba trophozoite with tapering pseudopodia
Discussion
Acanthamoebae are free-living, ubiquitous pathogenic amoebae with pointed pseudopodia (spiny amoeba). The organism exists as active trophozoites and resistant cysts [1]. Clinical suspicion is one of the important steps in diagnosing Acanthamoeba infection. Risk factors like contact lens wear or trauma and water exposure to eye usually give a hint towards diagnosis [2]. The mode of infection to humans and animals is through breaks in the skin or through the upper respiratory tract by cysts carried by air [3]. Acanthamoeba causes granulomatous amoebic encephalitis (GAE) in debilitated and immunosuppressed patients. In healthy persons, it may cause keratitis and corneal ulceration which can lead to blindness. Another case report from Geneva, Switzerland had documented Acanthamoeba keratitis detected from anterior chamber but the predisposing factor was contact lens wear [4]. Our patient probably got Acanthamoeba infection after trauma to the eye and contaminated water exposure. Diagnosis of Acanthamoeba keratitis infection can be made by identifying trophozoites and cysts in corneal scrapings or by cultures of contact lens disinfectants [5].
To conclude, we report a case of Acanthamoeba infection following penetrating therapeutic keratoplasty confined to the anterior chamber in a non-contact lens wearer where aqueous tap was helpful in the diagnosis and treatment.
Conclusion
It is noteworthy that Acanthamoeba infection of the anterior chamber of the eye is rare. To the best of our knowledge, this case is the first of its kind to be reported from India. This case highlights the fact that Acanthamoeba should be thought of in cases of ocular infection and efforts should be made to prevent its spread.
[1]. A Aksozek, K McClellan, K Howard, JY Niederkorn, H Alizadeh, Resistance of Acanthamoeba castellanii Cysts to Physical, Chemical, and Radiological Conditions.J Parasitol 2002 88(3):621-3. [Google Scholar]
[2]. B Clarke, A Sinha, DN Parmar, E Sykakis, Advances in the diagnosis and treatment of Acanthamoeba KeratitisJ ophthalmol 2012 :1-6. [Google Scholar]
[3]. DT John, Opportunistic amebae. In: Cox FEG, Wakelin D, Gillespie SH, Despommier DD, editorsHodder Arnold 2005 10th EditionLondonHodder Arnold:226-40. [Google Scholar]
[4]. NPL Dang Burgener, E Baglivo, B Farpour, C Brozou, A Dosso, A Safran, Acanthamoeba detection in the anterior chamberBr J Ophthalmol 2006 90(5):649-50. [Google Scholar]
[5]. I Claerhout, A Goegebuer, C Van Den Broecke, P Kestelyn, Delay in diagnosis and outcome of Acanthamoeba keratitis.Graefes Arch Clin Exp Ophthalmol 2004 242:648-53. [Google Scholar]