Case Report
A 48-year-old male patient presented with a growth over the chest wall in front on the left side since two years. Initially it was a small nodule beneath the skin of size 0. 5cm x 0. 5cm gradually progressed to present size of 8cm x 6cm the surface was ulcerated. Not associated with pain, fever or any other swellings anywhere in the body. No similar growth seen in the past elsewhere in the body, no history of surgical excision in the past. No significant family history. The middle aged man was moderately built and nourished. No lymphadenopathy. A proliferative ulcerated growth 10cm x 6cm x 6cm noted around 7cm lateral to midline on left side in third intercostal space. Its superior margin was 7cm below the clavicle in midclavicular line on left side. Surface was pinkish in appearance, irregular, raw and local areas of haemorrhage noted. All the borders were distinct and there was a groove all around growth and skin [Table/Fig-1,2a,2b]. The connecting stalk was 3cm x 2cm. The growth was non tender, firm in consistency and bled on touch. On contracting the pectoralis major muscle the growth was mobile in all directions. The surrounding skin was normal. The range of movements of left upper limb was normal. Dermato fibrosarcoma protuberance was suspected. Biopsy was not done and wide local excision was done.
An ulceroproliferative growth 10cm x 6cm x 6cm noted around 7cm lateral to midline on left side in third intercostal space

Surface is pinkish in appearance and irregular. All the borders were distinct

Surface is raw with local areas of haemorrhage. A groove was seen all around growth

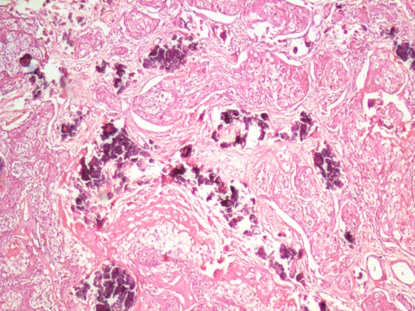
Histopathology
[Table/Fig-3,4]
Areas of necrosis, calcification acute on chronic inflammation and hemorrhage were also seen
Pleomorphic,multivacuolated, highly atypical epithelial cells arranged in nests in the dermis. Centrally located scalloped nucleus with foamy, multivacuolated cytoplasm secondary to intracytoplasmic lipid
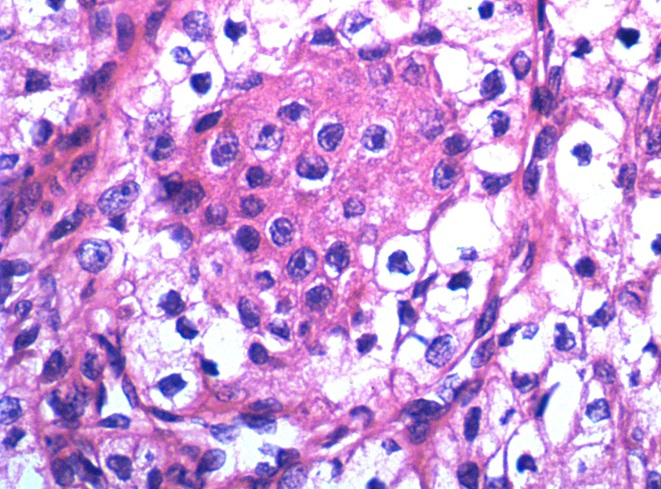
Histopathology revealed inconclusive pattern. When repeated sampling was done and oncopathologist was consulted they reported sebaceous carcinoma in Hematoxylin and eosin stains and refused for Immunohistochemical stains. It showed of stratified squamous lining epithelium with underlying tissue showing pleomorphic, multivacuolated, highly atypical epithelial cells arranged in rounded nests in the dermis [1,2]. Nucleus and nucleoli showed high grade pleomorphism, hyperchromatism, atypical mitotic figures including scalloped [3], centrally located nuclei with foamy, multivacuolated cytoplasm, secondary to intracytoplasmic lipid [4,3]. Areas of necrosis, acute on chronic inflammation and hemorrhage were also seen [1].
To rule out neoplasm that may be associated with Muir-Torre syndrome, the patient was screened. All haematological and biochemical parameters were within normal range. The tumour marker CEA was not elevated in the serum. Chest X-Ray, Ultrasound abdomen, Upper GI Endoscopy and colonoscopy were normal. Patient was discharged on 7th postoperative day. Patient was reviewed after one week and every three months after that till date. There were no features suggestive of local recurrences or distant metastasis till date [Table/Fig-5]. If there was a recurrence on the scar, after confirmation by biopsy radiotherapy was planned. For distant metastases chemotherapy was the first option.
Scar tissue with no features of local recurrences after three months

Discussion
Sebaceous gland carcinoma is a rare aggressive skin cancer derived from the epithelium of sebaceous glands [1,2,4]. Sebaceous carcinoma accounts to <1% of cutaneous malignancy [1]. Sebaceous carcinomas are generally divided into those occurring in ocular (75%) or extraocular locations. Ocular sebaceous carcinoma account for only 0. 2 to 0. 7 % of all eyelid tumour and it constitutes 75% of sebaceous carcinoma [5,6]. The upper eyelid is affected two to three times more often than the lower eyelid due to the greater number of Meibomian glands. Extra ocular sebaceous carcinoma constitutes for only 25% hence being still rare [5,7,8].
Extraocular sebaceous carcinoma most commonly arises in the head and neck region because it contains the highest density of sebaceous glands in the body [1,4,9]. Other reported locations include the external genitalia, the parotid and submandibular glands, the external auditory canal, the trunk, the extremities, the laryngeal and pharyngeal cavities, the uterine cervix and ovaries, the nasal vestibule and the oral mucosa [4,10]. So far only 180 cases are reported in extraocular sites [11]. A total of six cases are reported with sebaceous carcinoma over the chest wall with varied presentation.
According to [Table/Fig-6] which consists of the previous reported cases of sebaceous carcinoma of chest wall most of the cases were Males. (M:F;6:1). All patients were above 45 years. The presenting features were varied. The provisional diagnosis made in all cases were different. This shows the difficulty in diagnosing a case of sebaceous carcinoma. Two cases had lymph node metastasis and one was a recurrent case. Our case is the seventh reported with a huge exophytic growth of size 10cm x 6cm x 6cm.
| S. No | Authors | Year | Country | Age in yrs | Sex | Presentation on the chest wall | Size | Provisional diagnosis | Metastasis | Follow-up |
|---|
| 1 | Shah SN et al., [12] | 2009 | India | 65 | Male | Ulceroproliferative growth | Not mentioned | Squamous Cell Carcinoma | Nil | Not documented |
| 2 | Torres JS et al., [13] | 2012 | Brazil | 59 | Male | Ulcer | 20 x 18cm2 | Basal Cell Carcinoma, pyoderma gangrenosum | Nil | Not documented |
| 3 | Panjwani PK et al., [10] | 2012 | India | 44 | Male | Cystic nodule | 1 x 2.5cm2 | Epidermal cyst | Nil | 2 years, no recurrence and alive |
| 4 | Panjwani PK et al., [10] | 2012 | India | 48 | Male | Axillary lump | 5 x 4cm2 | Secondaries in axilla? Ca Breast | Axillary Lymph nodes | 18 months, no recurrence and Alive |
| 5 | Panjwani PK et al., [10] | 2012 | India | 78 | Female | Erythematous nodule with plaque | 6 x 4cm2 | Known case (previously operated) reccurence | Not specified | Not documented |
| 6 | Khan S et al.,[14] | 2014 | India | 45 | Male | Swelling | 5 x 7cm2 | Infected sebaceous cyst | Axillary lumph nodes | Not documented |
| 7 | Present study | 2014 | India | 48 | Male | Exophytic growth | 10 x 6 x 6cm3 | Dermatofibrosarcoma protuberance | Nil | 14 months, no recurrence and alive |
Worldwide sebaceous carcinoma is more common among Asians [8]. It occurs with greatest frequency in older adults in their sixth or seventh decade of life [8]. Few studies say there is no sex predilection [3]. Few studies concluded women tend to be affected 57-77% more than men [8,10].
Pathogenesis is inactivation of the tumour suppressor gene p53 or loss of the cell cycle mediator p21 may play a role in the pathogenesis of sebaceous carcinomas [4]. Radiation is a well-documented risk factor for the development of sporadic sebaceous carcinomas (i.e., those not associated with the Muir-Torre syndrome) [4]. Involvement of human papillomavirus (HPV) [3] has been suggested as a possible aetiologic factor. Patients on thiazide diuretics are also more prone [4].
Sebaceous carcinoma may be associated with syndromes like “MUIR TORRE SYNDROME“ [1,2,4]. The Muir-Torre syndrome is an autosomal dominant genodermatosis consisting of sebaceous neoplasms (sebaceous adenomas, sebaceous carcinomas, and sebaceous epitheliomas) with or without keratoacanthomas and visceral malignancies [2].
Definitive diagnosis is only by pathology. The tumour frequently exhibits diverse clinical presentations and histologic patterns, often resulting in a delay in an accurate diagnosis [6]. Histology may mimic BCC, SCC or may be uncertain [1]. In such cases initial thorough evaluation for search of occult internal malignancy in breast, bone, pelvic lymph node, rectum, etc [2]. Thus mammography, IVU, Chest X-Ray, CT Abdomen, pap smear, CEA, PSA, Complete blood picture, ESR, Renal and liver function tests, stool for occult blood and colonoscopy may be required [2]. Lifelong surveillance is required every 3 months [2,5,9].
It has been reported that extra-ocular and ocular sebaceous carcinoma are positive for Human milk fat globules subclass 1 (HMFG 1) [2], Human milk fat globule subclass 2 (HMFG 2) [2], Breast carcinoma antigen 255 (BCA 225) [2], Epithelial membrane antigen (EMA) [2,5,10]. They are negative for Carcinoembryonic antigen (CEA) [2], PAS [2], Alcian blue staining [2], S100 [5]. This enables sebaceous carcinoma to be distinguished from other tumours.
Although extraocular sebaceous carcinomas are generally viewed as less locally aggressive with a reduced tendency to metastasize than are the ocular tumours [6], there have been reports of local and regional as well as distant visceral metastases with this malignancy [1]. First to the draining lymph nodes [6,8]. Incidence of local recurrence is 9% to 36% within 5 yrs [8]. Sites of distant metastasis include the liver, lungs, bones, and brain [6,8,10]. Incidence of metastasis is equal among both ocular and extra ocular sebaceous carcinoma [8]. Metastasis has been reported to occur as late as five years after the initial diagnosis, lending support to the continual surveillance of patients with sebaceous carcinoma. Around 20-25% of cases show distant metastasis [6,8,10].
Treatment includes Local resection with 1cm margin [2,5,7], Cryotherapy, Topical Chemotherapy with agents like 5-FU [5,7], Radiotherapy [5], Isotretinoin 0.8mg/kg/day prevents cutaneous recurrence in the leision [2]. Multimodal approach is preferable.
Mohs micrographic surgery is well-accepted therapeutic modalities for sebaceous carcinoma [5,7]. Radiation therapy should be reserved for patients unable or unwilling to undergo surgery [5]. Large defect created after excision can be covered with SSG or flaps with the help of plastic surgeon.
The main prognostic factor is the time to diagnosis; when the diagnosis is made in the first six months the mortality rate is about 14% [10]. After the sixth month the mortality rates rises to 38% [10]. five years survival for extraocular sebaceous carcinoma is 68% [11]. Factors associated with poor prognosis are [3] vascular, lymphatic, orbital metastases, poor differentiation, multicentric origin, duration of symptoms more than six months, tumour diameter exceeding 10mm and a highly infiltrative pattern.
Conclusion
Sebaceous Cell Carcinoma is a rare and aggressive malignancy. It is to be considered as a differential diagnosis in any ulceroproliferative growth over the skin. This tumour should suggest the possibility of MTS and alert to search an occult internal malignancy. The patient should be followed up for long periods because of late reccurence and metastases are known.
[1]. Tandon RK, Jasani Jasmin, Patel Jigar, Patel Arti, Extra ocular sebaceous carcinoma of the sternum in biopsy: A case reportIndian Journal of Applied Basic Medical Sciences 2012 14B(19):119-23. [Google Scholar]
[2]. Ho C. K., Sebaceous CarcinomaHong Kong Dermatology & Venereology Bulletin 2002 10(3):129-32. [Google Scholar]
[3]. Ostler Daniel A, Reed Jon Allison, Pathology of Sebaceous Carcinoma, medscape references [Google Scholar]
[4]. Martinelli Paul T, Cohen Philip R, Schulze Keith E, Tschen Jaime A, Nelson Bruce R, Sebaceous Carcinoma; Chapter 17 Skin Cancer:240-50. [Google Scholar]
[5]. Oh S. -H, Lee S. -S, Seo Y. -J, P75 Extraocular sebaceous carcinoma treated with wide excision and island flap, Melanoma Research June 2010-20 :76-e77. [Google Scholar]
[6]. Hammedi Faten, Trabelsi Amel, Belajouza Colanda, Beïzig Nadia, Gannouchi Nadia, Sriha Badreddine, Extra ocular sebaceous carcinoma of the thigh: A case reportN Am J Med Sci 2010 January 2(1):48-50. [Google Scholar]
[7]. Torres José Saulo, Amorim Ana Cristina, Hercules Flavio Marcondes, Kac Bernard Kawa, Giant extraocular sebaceous carcinoma: case report and a brief review of a literatureDermatology Online Journal 18 (11):7 [Google Scholar]
[8]. James MS, Elston Dirk M, Dermatologic Manifestations of Sebaceous Carcinoma, medscape references [Google Scholar]
[9]. Paschalis G, Sotirios B, Vasiliki T, Barbara C, Extraocular sebaceous carcinoma mimicking benign sebaceous cystBMJ Case Reports 2013 [Google Scholar]
[10]. Panjwani PK, Tirumalae R, Crasta JA, Manjunath S, Rout P, Extraocular sebaceous carcinoma: a series of three cases with varied presentationDermatol Pract Conc 2012 2(1):7 [Google Scholar]
[11]. Dasgupta Tina, Lynn D, Wilson and James B. A Retrospective Review of 1349 Casesof Sebaceous CarcinomaCancer 2009 115:158-65.2008 American Cancer Society [Google Scholar]
[12]. Shah SN, Sebaceous carcinoma on the chest wall of an elderly maleGujarat Medical journal 2009 Vol 64(2) [Google Scholar]
[13]. Torres JS, Ana C A, Flavio M H, Bernard K K, Giant extraocular sebaceous carcinoma: case report and a brief review of a literatureDermatology Online Journal 18 (11):7 [Google Scholar]
[14]. Khan S, Husain M, Ansari MM, Sebaceous Gland carcinoma - Case Report and Literature ReviewJSM Clin 2014 Case Rep 2(2):1025 [Google Scholar]