Incidental Detection Microfilaria in Subcutaneous Breast Nodule of Lactating Female Fnac: A Rare Case Report
Ajay KR. Singh1, Prashant Gupta2, Soma Yadav3, H.S Pahawa4
1Assistant Professor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
2Assistant Professor, Department of Microbiology, King George’s Medical University, Lucknow, UP, India.
3Resident Doctor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
4Professor, Department of Surgery, King George’s Medical University, Lucknow, UP, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajay Kumar Singh, Assistant Professor, Department of Pathology, King George’s Medical University Lucknow-226003, UP, India.
Phone: 919415082798,
E-mail: drajaysingh007@gmail.com
Filariasis is a major public health problem which is faced in tropical countries like India. Its diagnosis is made by using peripheral blood smears. However, microfilaria has been detected incidentally during FNACs of various lesions, which were done in clinically unsuspected cases. We are reporting here, an uncommon case of filariasis, which caused a nodular, subcutaneous swelling in left breast of a 30 year old lactating female. A nodular subcutaneous swelling can be caused in breast of a lactating female by lactational associated mastitis, but filaria causing a nodular swelling in a lactating breast is a rare presentation. Aspiration of the swelling demonstrated enormous pathogen presence caused by Woucheria bancrofti and the patient responded well to six weeks of daily anti-filarial treatment with diethylcarbamazine citrate.
Microfilaria, FNAC, Subcutaneous nodule
Case Report
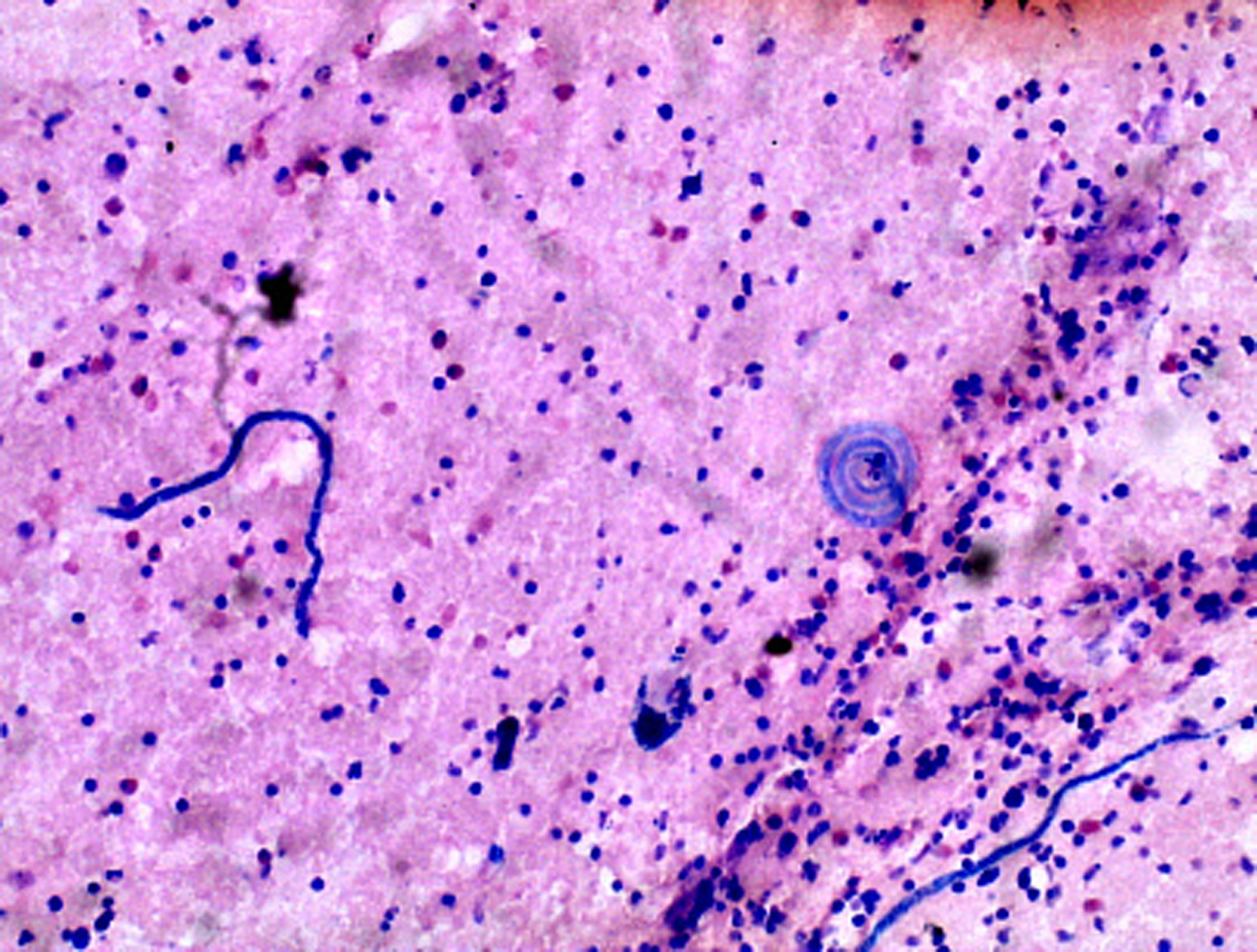
A 30-year-old, breast-feeding female presented with a painless, cystic-to firm swelling, which measured 2 cm, over left breast [Table/Fig-1] about 2 cm above the nipple- areola complex. Clinically, it was a perplexing situation, as the patient had no other symptoms apart from intermittent fever with malaise. On examination, a string like structure was felt in the subcutaneous skin, which measured 2 cm in length. The patient had stopped breast feeding since the past 7 days because of the same reason. There was no neurological deficit or lymphadenopathy. USG showed left preareolar dilated and tortuous channels in mammary zone, which were suggestive of dilated ducts caused by lactational cysts, in view of the history of lactation. Patient was sent to Pathology Department of medical university for FNAC. Aspiration from swelling solved the diagnostic question as it revealed a straw coloured fluid, which showed large number of microfilariae on microscopic examination [Table/Fig-2]. Examination of smears proved that these were W. bancrofti, as there was presence of a hyaline sheath, a large cephalic space and presence of somatic cells (nuclei), which appeared as granules. The tail tip was free from nuclei. Few inflammatory cells, multinucleated giant cells and occasional benign ductal epithelial cells of the breast were also seen.
Peripheral blood smear examination did not show presence of microfilariae. Patient had no past history of filariasis. After the diagnosis was made, the patient was prescribed two weeks of therapy with diethylcarbamazine (2mg/kg/day). After one month’s follow up, patient improved and has been living well since then.
Photograph of breast showing skin nodule

Haematoxyline and Eosine stain (20x) of breast nodule showing numerous microfilaria
Discussion
Lymphatic filariasis is a major health problem which is faced in tropical countries such as India, China, West Indies, Japan and parts of Africa [1-3] . The disease is endemic all over India, especially in states like Uttar Pradesh, Bihar, Jharkhand, Andhra Pradesh, Orissa, Tamil nadu, Kerala and Gujarat [4] . Causative organisms are Wucheria bancrofti, Brugia malayi and Brugia timori. According to WHO’s present findings, over 120 million people are currently infected and about 40 million have been diagnosed to have this disease and have been incapacitated by the disease [5] . W. bancrofti has a worldwide distribution and it accounts for 90% of detected filariasis cases, which is more prominent than Brugia malayi and Brugia timori. Clinical manifestations include lymphangitis, lymphadenitis, hydrocele and elephantiasis [3] .
Female breast is an unusual site and presentation of filariasis as a subcutaneous nodule is even rarer [2,3,6,7] . W. broncrofti presenting as a subcutaneous nodule is a very rare presentation [1] . Subcutaneous filariasis is mainly caused by Loa loa, Oncocerca volvulus, and Mansonella [1] . The cytology of a filarial infestation can reveal microfilariae with or without adult worms and associated eosinophils, neutrophils, and monouclear cells. The presence of epithelioid cells, granulomas and giant cells is another usual finding in filariasis and so it could be a diagnostic problem when it is associated with granulomatous diseases such as tuberculosis and leprosy, because of common cytomorphological features.
Humans are exclusive and definitive hosts for W. bancrofti. The major vectors are Culex mosquitoes in most of the urban areas and Anopheles mosquitoes in rural areas. Adult worms reside in lymphatic vessels and the larval forms (microfilariae) may circulate in the peripheral blood.
USG can be used as a valuable diagnostic tool in cases of lymphatic filariasis and it can demonstrate the adult worms. A specific distinctive pattern of movement which is called filarial dance has been described in USG [8] . These worms can later on calcify and then they cannot be distinguished from intraductal carcinoma of breast on mammography.
Microfilariae may present in an unusual fashion and so, careful screening of cytology smears, even when filariasis is not suspected, as it was in this case, where patient had no complaints other than a subcutaneous nodule, is important medically for diagnosis and for treatment of the patients, especially in endemic areas [9] . Breast nodules which occur in pregnant and lactating female due to filarisis are a very uncommon presentation. FNA can be used as a safe and reliable method for evaluating breast masses in pregnant females [3] . This is the first case of filariasis which presented with a breast nodule in a lactating female. No such case has been described in the literature before. In the past, diagnosis of microfilaria was based on identification of the microfilariae in blood. The microfilariae of W. bancrofti demonstrate periodicity and blood samples have to be taken at night, between 10 pm and 2.00 am [1] .
Nevertheless, newer studies have reported on making the cytologic diagnosis of filariasis by doing FNA from sites other than breast, such as the testis, epididymis, thyroid, lung, lymph nodes, and skin [3,10,8] . A recent review done of these cases revealed that 18 of these cases had undergone blood examinations for microfilaria, of which only 2 (12%) had been found to be positive [2] . Therefore, because of low yield and stringent sampling requirements of a blood examination, FNA cytology appears to be a more convenient, quick and effective diagnostic method [3 ,10 ,11] . Making an early diagnosis and providing an early treatment, prevent the more severe manifestation the disease, especially lymphatic filariasis [12] . To conclude, one should always consider filariasis in the differential diagnosis of unusal subcutaneous cystic swellings, especially in endemic areas [13] and FNAC is the best tool for making an early diagnosis, even when microfilariae are not found in the peripheral blood smears.
[1]. AG Valand, BS Pandya, YV Patil, LG Patel, Subcutaneous filariasis : An unusual case report.Indian J Dermatol. 2007 52:48-9. [Google Scholar]
[2]. N>G Singh, L Chatterjee, Filariasis of the breast, diagnosed by fine needle aspiration cytologyAnn Saudi Med. 2009 29(5):414-5. [Google Scholar]
[3]. M Lau, P Tauchi, M Kim, F Liu, T Namiki, Filarisis of the breast in a pregnant women diagnosed by fine-needle aspiration cytology: a case report.Infect Dis Obstet Gynecol 1995 3:245-7. [Google Scholar]
[4]. SK Mitra, RK Mishra, P Verma, Cytological diagnsosis of microfilariae in filarisis endemic areas of eastern Uttar PradeshJ Cytol. 2009 26:11-4. [Google Scholar]
[5]. World Health Organisation global programme to eliminate lymphatic filariasis: Progress report on mass drug administration 2010.Wkly Epidemiol Rec 2011 86(35):377-88. [Google Scholar]
[6]. N Rukumangadha, V Shanthi, CM Kiran, NP Kumari, SJ Bai, Breast filariasis diagnosed by fine needle aspiration cytology: a case report.Indian J Pathol Microbiol. 2006 49(2):243-4. [Google Scholar]
[7]. Bhardwaj S, Mahajan D, Attri MR, Filariasis of the Breast.JK Science 2007 9(2):98-9. [Google Scholar]
[8]. PK Garg, BK Jain, V Rathi, N Singh, D Mohanty, Mid-arm and Epitrochlear lymphadenopathy: a clinico-radiological SurpriseJ Infect Dev Ctries 2011 5(11):820-4. [Google Scholar]
[9]. P Singh, N Chand, R Singal, M Madan, J Bala, Filariasis presenting as multiple subcutaneous nodules : a rare case report.Acta Med Indones 2011 43(4):249-51. [Google Scholar]
[10]. S Gupta, R Gupta, B Bansal, S Singh, K Gupta, M Kudesia, Significance of incidental detection of filariasis on aspiration smears: a case seriesDiagn. Cytopathol 2010 38(7):517-20. [Google Scholar]
[11]. B Kumar, S Karki, SK Yadava, Role of fine needle aspiration cytology in diagnsosis of filarial infestation.Diagn Cytopathol. 2011 39(1):8-12. [Google Scholar]
[12]. SK Mondal, Incidental detection of filaria in fine-needle aspirates : a cytologic study of 14 clinically unsuspected cases at different sitesDiagn Cytopathol. 2012 40(4):292-6. [Google Scholar]
[13]. RC Dwivedi, P Gupta, RC Dwivedi, K Kishore, N Bhatia, Lymphadenovarix of Head-neck region-A rare presentation of Bancroftian Filariasis.J Trop Pediatr 2009 55(5):332-4. [Google Scholar]