Perianal fistulae has been affecting mankind since antiquity and are mentioned in literature from the time of Hippocrates. As many great kings and rulers have also suffered from the disease, much has been written on the subject.
Perianal fistula is a tract lined by infected granulation tissue that connects anal canal or rectum to the skin around anus. Its wall is made of inflammatory granulation as well as fibrous tissue. Perianal fistulae occur in approximately 10 out of 10,000 persons [1]. It usually occurs in adult men with maximum incidence between third and fifth decades [2]. Perianal fistulae are not only painful and irritating but can also be a nidus for systemic spread of infection. The most common presenting symptom is discharge (65% of cases) [1]. Perianal fistulae sometime leads to acute abscess formation where immediate surgical decompression becomes necessary, however, most simple fistulae can be treated electively using fistulotomy. The goal of treatment in an anal fistula is to eliminate the primary opening, any associated tracts and any secondary openings without loss of continence [3].
The external opening is visible on inspection and internal opening can be determined by probing, however it seldom helps and not recommended these days. Role of imaging is to define the course of the tract between these openings so that the appropriate surgical option can be used. Surgical treatment of fistula-in-ano is notorious for high recurrence rates. The successful surgical management of fistula-in-ano depends upon accurate preoperative assessment of the course of the primary fistulous tract, the presence and site of any secondary extensions or abscesses [4].
The objective of our study was to evaluate the role of MRI in detection and characterization of perianal fistulae and correlating it with surgical findings.
Methods
The present study included 50 patients with suspected perianal fistulae having one or more external openings attending outpatient department or admitted to our institute were included in the study. Previously operated or patients with recurrent perianal disease were excluded from the study. All patients underwent MRI examinations on Philips Achieva 1.5 Tesla MRI, Philips Medical Systems, Veenpluis, The Netherlands, using Sense Body Coil (Receive only coil). Sequences were acquired in both coronal and axial planes [Table/Fig-1].
LMR imaging protocol. T1W -T1 weighted, T2W - T2 weighted, FS - Fat Saturated, TSE- Turbo Spin Echo, TRA- Transverse, COR- Coronal, TR- Repetition Time, TE- Echo Time, FOV- Field of View, NSA- Number of Signal Averages, MAT-Matrix, REC-Reconstruction
| Numbers | TR | TE | FOV | NSA | MAT / REC |
|---|
| T2W TSE COR FS | 3500 | 90 | 400 | 3 | 252/352 |
| T2W TSE TRA FS | 3500 | 90 | 400 | 3 | 252/352 |
| T1W TSE TRA | 641 | 14 | 400 | 3 | 252/352 |
| T1W TSE COR | 641 | 14 | 400 | 3 | 252/352 |
| T1W TSE COR FS | 756 | 14 | 400 | 3 | 252/352 |
| T1W TSE TRA FS (Post contrast) | 756 | 14 | 400 | 3 | 252/352 |
| T1W TSE COR FS (Post contrast) | 756 | 14 | 400 | 3 | 252/352 |
Gadopentate dimeglumine 0.1 mmol/kg was used as contrast administered intravenously by hand. Each MR image was analysed for specific features that were relevant to the evaluation of perianal fistulae. St. James’s University Hospital MR Imaging Classification of Perianal Fistulae [5] was used to classify fistulae. Surgical exploration was done in all the cases, with the aid of MRI observations and the peroperative findings were used to scrutinize the imaging results. Both internal and external openings were recorded as their position on anal clock and at their correct level in anal canal / rectum.
Statistical Analysis
Imaging findings on T2W TSE fat saturated and postcontrast T1W TSE fat saturated sequences were compared with each other using Chi-square test in relation to correct detection of abscess, horseshoeing, secondary tract and internal opening.
Results
Amongst the 50 patients studied, the mean age was 42 (22-70) years of which 45 patients (90%) were males and 5(10%) patients were females. Age group between 30-39 years accounted for maximum number of cases (34%). Majority of the patients studied have single external opening (45), four patients had two external openings and only one patient had three external openings. In MRI protocol both coronal and axial planes found to be important in complete evaluation. The coronal planes provided the details of the levator ani and puborectalis muscles and the axial planes provided the clear visualisation of the intersphincteric space. MRI findings were correlated to surgical findings [Table/Fig-2].
Surgical correlation of MRI findings. MRI- Magnetic Resonance Imaging
| MRI Findings | True positive | False positive | False negative | True negative |
|---|
| Primary tract | 43 | 1 | 2 | 4 |
| Abscess | 7 | 2 | 1 | 40 |
| Secondary tracts | 15 | 2 | 1 | 32 |
| Horseshoeing | 7 | 2 | 1 | 40 |
| Internal openings | 46 | 1 | 2 | 4 |
Discussion
Perianal fistula is a disease of adult males, occurrence in females in quite uncommon. Conventional fistulography, ultrasonography and computed tomography have proved to be insufficient in correct assessment of the disease [6]. Role of MRI in evaluation of fistula-in-ano was first studied by Koelbel et al., [7] and was followed by many studies till date.
Among 50 cases included in the study, perianal fistulae were seen peroperatively in 45 cases and 5 were negative for perianal fistulae (4 sinuses, one cutaneous lesion only). MRI could correctly detect and classify only 43 cases. We found that MRI has a sensitivity of 95.56%, specificity of 80% and positive predictive value of 97.73% in correctly detecting and grading primary tract. Examples of various grades fistulae are given [Table/Fig-3,3band3c],[Table/Fig-4a,4b],[Table/Fig-5a,5b,5c,5d][Table/Fig-6a,6b,6c]. Initial reports by Lunniss et al., suggested a concordance rate of 86% to 88% [8, 9]. Later studies are describing up to 100% sensitivity for detecting and grading the primary tract [10].
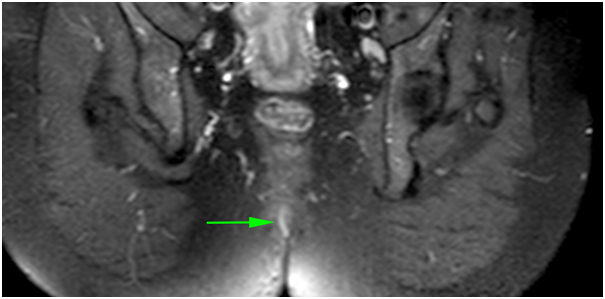
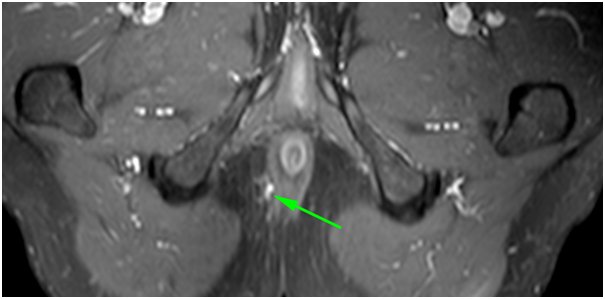
Coronal post contrast T1W FS image is showing enhancing primary tract in left ischioanal and ischiorectal space (arrow) which is opening into anal canal below the levator muscle (arrowhead). Origin of secondary tract is also visible. Similarly, hyperintense primary tract is also visible in coronal T2W FS images in
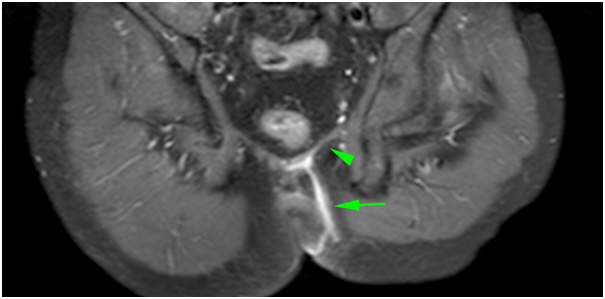
(arrow). It was classified as grade-4 perianal fistula (St. James University Hospital MR Imaging Classification of Perianal Fistulae).T1W-T1 weighted, T2W-T2 weighted, FS-Fat saturated
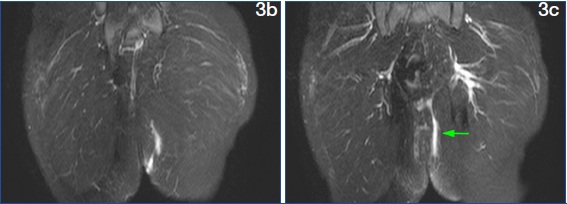
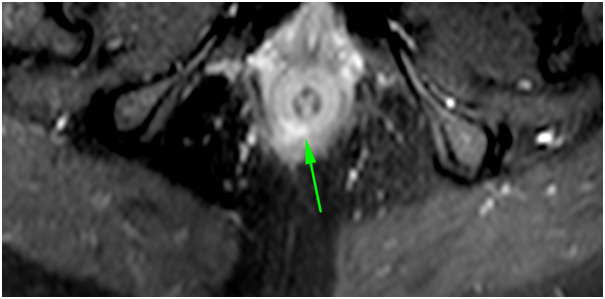
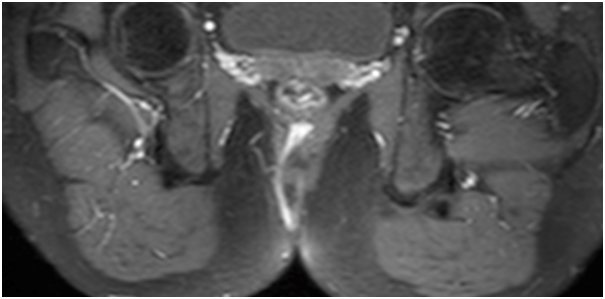
Coronal post contrast T1W FS image is showing enhancing primary tract in left ischioanal and ischiorectal fossa with secondary extension (arrow) breaching and going above the levator plate. In same patient coronal T2WFS image.
at different level is showing abscess formation at the site of internal opening (arrowhead) and hyperintense secondary tract extending above the levator plate (arrow). It was a grade-5 perianal fistula (St. James University Hospital MR Imaging Classification of Perianal Fistulae). T1W-T1 weighted, T2W-T2 weighted, FS-Fat saturated
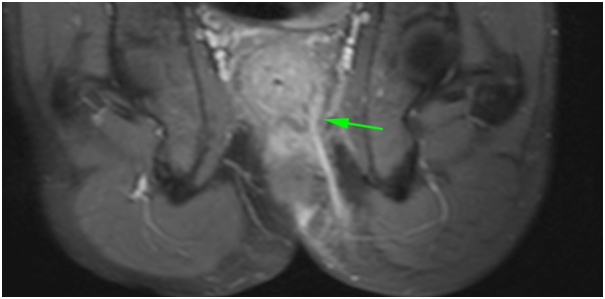
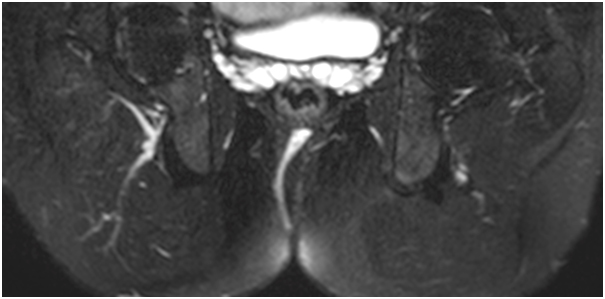
Coronal T2W FS image is showing hyperintense primary tract (arrow) in right ischioanal fossa. In same patient
axial T2WFS image is showing the site of internal opening (arrow). Another axial T2WFS image
is showing intersphincteric nature of primary tract (arrow)
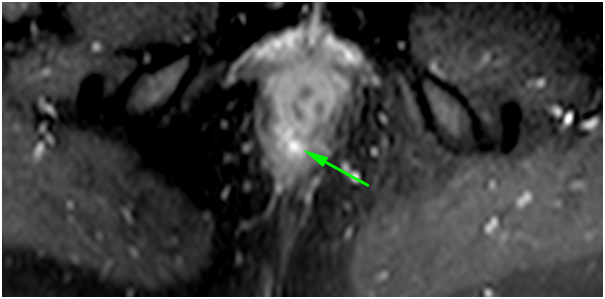
is a coronal post contrast T1WFS image showing enhancing primary tract in right ischioanal fossa (arrow). It was a grade-1 perianal fistula (St. James University Hospital MR Imaging Classification of Perianal Fistulae). T1W-T1 weighted, T2W-T2 weighted, FS-Fat saturated
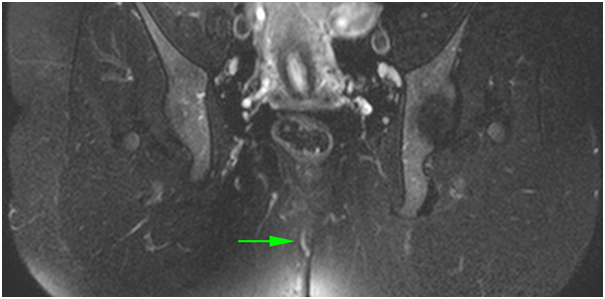
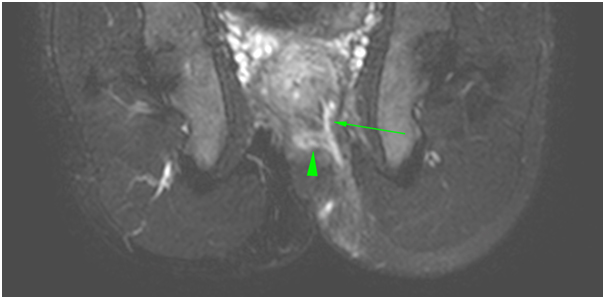
Axial post contrast T1W FS image is showing enhancing primary tract (arrow) in right ischioanal fossa lateral to anal sphincter complex. In same patient
Coronal T1WFS image is showing the enhancing tract in right ischioanal and ischiorectal fossa which is seen crossing the anal sphincter complex
Is coronal T2WFS image showing transsphincteric primary tract. It was a grade-3 perianal fistula (St. James University Hospital MR Imaging Classification of Perianal Fistulae). T1W-T1 weighted, T2W-T2 weighted, FS-Fat saturated
As in study done by Mendoza et al., [11], Torkzad MR [12], and in present study also it was assumed that fluid collection larger than 10 mm in diameter is an abscess; whereas a fluid filled tubular structure with a diameter smaller than 10 mm is a fistula. MRI correctly identified abscess in seven out of eight cases with correct establishment of their relation to levator ani and puborectalis muscle. In one case where MRI detected an abscess, but came out negative on surgery, can be attributed to the fact that it was operated after a delay of 12 days and abscess might have drained in or drained out in mean course of time. MRI was found to have a sensitivity of 87.50 %, specificity of 95.24 %, positive predictive value of 77.78 % and negative predictive value of 97.56 % in correctly detecting abscess. Previous studies done by Beets-Tan et al., [10] and Mahjoubi et al., [13] reported a similar high sensitivity and specificity of 96% and 80% respectively.
Secondary tracts were detected on surgery in total 16 patients, and MRI could correctly identify all the secondary tracts in 15 patients. In one patient MRI failed to detect secondary tract first but was seen retrospectively after disclosure of surgical findings. MRI has a sensitivity of 93.75 %, specificity of 94.12 %, positive predictive value of 88.24 % and negative predictive value of 96.97 % in correctly detecting secondary tracts. It correlates well with previous study by Mahjoubi et al., [13] who reported sensitivity and specificity of 80 and 100% respectively.
Horseshoeing is a type of secondary tract with extension in horizontal plane on either side of midline. In our study MRI was found to have a sensitivity of 87.50% and specificity of 95.24% in detecting horseshoeing. It correlated well with previous study by Beets-Tan et al., [10], who reported sensitivity, specificity and PPV of 100% and study by Barker et al., [14] who reported sensitivity of 97%.
MRI was not able to distinguish clearly the internal sphincter and anal mucosa, therefore the site of the internal opening was inferred by the proximity of the tract within the intersphincteric space [14]. According to Halligan et al., [15] area of maximal intersphincteric sepsis is the probable site of internal opening. An internal opening was considered as correctly identified when it was at the correct level in the anal canal and was within the correct quadrant [10]. Among total 48 internal openings found on surgery, MRI correctly identified 46. In one case it wrongly identified an internal opening and case was actually a sinus tract. Present study has reported sensitivity of 95.83 %, specificity of 80.00% and positive predictive value of 97.87 % in detecting internal openings. This correlates well with previous study by Beets-Tan et al., [10] who reported sensitivity of 96 %, specificity of 90 % and PPV of 90 %. Similarly Barker et al., [14] reported that sensitivity of MRI is 80% in detecting internal openings.
Finally, T2 weighted turbo spin echo fat saturated images and postcontrast T1 weighted turbo spin echo fat saturated images were compared for detection of abscess, secondary tract, horseshoeing and internal openings. Both the sequences provided exactly similar information regarding abscess and horseshoeing in all the cases. There were only two cases where secondary tract was detected on post contrast T1 W TSE FS images and was missed at T2W TSE FS images; however it was given in MRI report, as it came positive in one sequence. On comparing accuracy [Table/Fig-7] for correct detection of secondary tract between these two sequences no significant difference was noted (x2 = 1.087; df = 1; p = 0.297; not significant). Two internal openings were missed by T2W TSE FS which were surgically present, in comparison to 5 internal openings which were missed by post contrast T1W TSE FS images. On comparing these findings [Table/Fig-8], again no statistically significant difference was noted (x2 = 1.705; df = 1; p = 0.192; not significant). Finally it was concluded that among T2W TSE FS and post contrast T1W TSE FS images, there was no statistically significant difference in correctly detecting abscesses, secondary tracts, horseshoeing and internal openings. It was an important inference of our study, since contrast study can be ommited from the MRI protocol, while evaluating primary / previously unoperated perianal fistulae.
Comparison between secondary tracts as visualised on T2W TSE fat saturated and post contrast T1W TSE fat saturated sequences
| (A) T2W TSE FS |
|---|
| SURGERY(+) | SURGERY(-) |
|---|
| MRI(+) | 15 | 2 |
| MRI(-) | 1 | 32 |
|
|---|
| True Posi-tive | False Posi-tive | True Neg-ative | False Neg-ative | n | Sensi-tivity (%) | Speci-ficity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Accuracy (%) |
|---|
| 15 | 2 | 32 | 1 | 50 | 93.75 | 94.12 | 88.24 | 96.97 | 94.00 |
|
|---|
| (B) POST CONTRAST T1W TSE FS |
|---|
| SURGERY(+) | SURGERY(-) |
|---|
| MRI(+) | 13 | 2 |
| MRI(-) | 3 | 32 |
|
|---|
| True Posi-tive | False Posi-tive | True Neg-ative | False Neg-ative | n | Sensi-tivity (%) | Speci-ficity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Accuracy (%) |
|---|
| 13 | 2 | 32 | 3 | 50 | 81.25 | 94.12 | 86.67 | 91.43 | 90.00 |
Comparing Accuracy of T2W TSE FS and POST CONTRAST T1W TSE FS: x2 = 1.087; df = 1; p = 0.297; not significant
MRI - Magnetic Resonance Imaging, T1W -T1 weighted, T2W - T2 weighted, FS - Fat Saturated, TSE- Turbo Spin Echo
Comparison between internal openings as visualised on T2W TSE fat saturated and post contrast T1W TSE fat saturated sequences
| (A)T2W TSE FS |
|---|
| SURGERY(+) | SURGERY(-) |
|---|
| MRI(+) | 44 | 1 |
| MRI(-) | 4 | 4 |
|
|---|
| True Posi-tive | False Posi-tive | True Neg-ative | False Neg-ative | n | Sensi-tivity (%) | Speci-ficity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Accuracy (%) |
|---|
| 44 | 1 | 4 | 4 | 53 | 91.67 | 80.00 | 97.78 | 50.00 | 90.57 say 91% |
|
|---|
| (B) POST CONTRAST T1W TSE FS |
|---|
| SURGERY(+) | SURGERY(-) |
|---|
| MRI(+) | 41 | 1 |
| MRI(-) | 7 | 4 |
|
|---|
| True Posi-tive | False Posi-tive | True Neg-ative | False Neg-ative | n | Sensi-tivity (%) | Speci-ficity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Accuracy (%) |
|---|
| 41 | 1 | 4 | 7 | 53 | 85.42 | 80.00 | 97.62 | 36.36 | 84.91 say 85% |
Comparing Accuracy of T2W TSE FS and POST CONTRAST T1W TSE FS: x2 = 1.705; df = 1; p = 0.192; not significant.
MRI - Magnetic Resonance Imaging, T1W -T1 weighted, T2W - T2 weighted, FS - Fat Saturated, TSE- Turbo Spin Echo
Parks classification used to classify perianal fistulae is basically a surgical classification. To easily report all the relevant imaging findings St. James’s University Hospital MR Imaging Classification of Perianal Fistulae was proposed by radiologists though it does not represent an official surgical reference [5]. Being a simple classification to apply and remember it helps in better describing the disease so that surgeons can understand the relevant findings. According to St. James’s University Hospital MR Imaging Classification of Perianal Fistulae, following grading is used: 0, normal appearance; 1, Simple linear intersphincteric fistula; 2, intersphincteric fistula with intersphincteric abscess or secondary fistulous tract; 3, transsphincteric fistula; 4, transsphincteric fistula with abscess or secondary fistulous tract within the ischio-anal or ischio-rectal fossa; 5, supralevator or translevator disease [5, 12].
Sometime contrast enhanced vascular structures, suture material and relatively thin puborectalis muscle may confuse the radiologist hindering correct localisation of the fistulous tract. Further, it is also important to choose a correct plane for coronal images, relevant to anal canal to avoid misinterpretation.
Recommendations
MRI is gold standard and should be the modality of choice for detail preoperative evaluation of perianal fistulae.
Intravenous contrast MRI study can be omitted, particularly while evaluating primary/previously unoperated perianal fistulae.
Limitations
The high cost of scan and availability of MRI.
The present study considered only the primary cases; thus, the reverberation of our research is not applicable to recurrent/previously operated cases wherein distorted anatomy and presence of scar tissue/fibrosis pose an unusual challenge.
Conclusion
High sensitivity (87.5-95%) and specificity (80-95%) of MRI findings were recorded in the present study for the assessment of surgically important parameters (primary tract, internal opening, secondary tract, abscess and horseshoeing) of perianal fistulae comparing with the operative observations. There was no statistically significant difference (accept H0; p>0.05) in imaging findings between T2-weighted fat saturated and postcontrast T1- weighted fat saturated sequences.
Comparing Accuracy of T2W TSE FS and POST CONTRAST T1W TSE FS: x2 = 1.087; df = 1; p = 0.297; not significant
MRI - Magnetic Resonance Imaging, T1W -T1 weighted, T2W - T2 weighted, FS - Fat Saturated, TSE- Turbo Spin Echo
Comparing Accuracy of T2W TSE FS and POST CONTRAST T1W TSE FS: x2 = 1.705; df = 1; p = 0.192; not significant.
MRI - Magnetic Resonance Imaging, T1W -T1 weighted, T2W - T2 weighted, FS - Fat Saturated, TSE- Turbo Spin Echo