Puerperal sterilization is one of the surgeries which are most commonly performed in the immediate post partum period. Anaesthesia given in these patients should ensure faster recoveries and minimal impairment of psychomotor functions, to enable satisfactory handling of the babies by their mothers in the postoperative period.
The combination of fentanyl and propofol ensures that adequate anaesthesia and analgesia are provided during the intraoperative period, but the post-operative recovery is not completely satisfactory [1]. There have also been incidences of intra and post operative respiratory depression and hypotension [2]. Ketamine has a different recovery profile and superior analgesia, it causes lesser incidence of hypotension, apnoea and airway obstruction, lesser sedation and a lesser incidence of post operative nausea and vomiting [3]. Hypertension and psychomimetic emergence reactions limit the role of ketamine as a sole anaesthetic agent.
This study was undertaken to compare the intraoperative haemodynamics and post operative recovery profile, while using ketamine versus fentanyl under intravenous anaesthesia with propofol for puerperal sterilization.
Materials and Methods
This randomized, clinical study was conducted after getting ethical clearance from the institutional ethics committee. Sixty ASA physical status 1 patients who were admitted to undergo puerperal sterilizations, 48 hours after their deliveries, were included. The exclusion criteria were patients with anticipated difficult airway or psychiatric Illness. A previous study done by Akin et al., used 40 sample size with 20 each. Based on this study, for an alpha error of 0.05, power of study as 80% for a hypotension difference of 20%. The sample size was estimated to be 60 with 30 each. Written Informed consent was taken from all the patients. All the patients were kept nil per oral and were premedicated with ranitidine, metoclopramide and glycopyrrolate 0.2 mg, 60 minutes prior to performance of the surgery. In the theatre, baseline heart rate (HR), non invasive systolic pressure (SBP) and diastolic pressure (DBP) and room air saturation (SPO2) were noted and an 18 G peripheral intravenous (IV) line was secured. All patients were started on oxygen at a flow rate of 4L/min, with use of Hudson’s facemask and they continued to receive it intraoperatively. All patients received inj. midazolam 1 mg IV. Patients were then randomized to two groups by using sealed envelope technique.
Group PK (n = 30): infusion of a ketamine – propofol solution was prepared by mixing 20ml of 1% propofol, 4mL of ketamine (200mg) and 1ml of normal saline. The final concentration had propofol -8mg/ml and ketamine -8mg/ml.
Group PF (n = 30): received fentanyl 2 μg/kg IV bolus, followed by a propofol infusion which was prepared by mixing 20 ml of 1% propofol with 5 mL of normal saline. The final concentration of propofol was 8 mg/ml.
The anaesthesiologist who assessed the parameters was blinded to the study drugs.
In both the groups, the infusion was started at 300ml/hr, till patient lost consciousness. Subsequently, the rate was set at 1.5ml/kg/hr for group PF and at 0.75ml/kg/hr for group PK. After the initial 10 minutes, the infusion rate was reduced to 1ml/kg/hr for group PF and to 0.5ml/kg/hr for group PK. Bupivacaine 0.25% was infiltrated at the surgical site at a dose of 1.5 mg/kg, after induction (Omit giving) before making the incision.
Throughout the intraoperative period, HR, SBP, DBP and SPO2 were measured at 5 minute intervals. Any episodes of hypotension or bradycardia (a change of 20% from the baseline) and episodes of desaturation (a change of 10% from the baseline) were noted. Adequacy of satisfactory surgical conditions in terms of patient movement and relaxation were noted. Additional bolus doses of propofol were given on patient movement and they were noted. The infusion was stopped end operatively, the time taken for giving response to verbal commands was recorded and patients were shifted to post-anaesthetic care. The following postoperative parameters were assessed at awakening and at 1,2,4 and 6 hours postoperatively. Pain score was assessed by using visual analogue scale (VAS). Sedation scores, maternal ease and comfort in handling the baby, time when mother was able to breastfeed the baby, postoperative nausea and vomiting (PONV), dreams and delirium were also recorded. Patients with VAS scores of greater than 3 were given 50 mg of intramuscular diclofenac and the time at which first analgesic was received was noted.
Statistical Analysis
Data was analyzed by using independent students t-test for the analysis of continuous variables between the groups and analyses of variance was used to compare the significance of repeated measures within the groups. Comparison of parameters which were assigned numeric scores was done by using Mann Whitney U-test and Chi- square test. p-values of < 0.05 were considered to be significant for all tests. The analysis was done by using SPSS software package.
Results
The two groups were comparable in terms of age, weight and the baseline recordings of HR, SBP, DBP and SPO2 [Table/Fig-1].
Patient details and baseline recordings
| Group PF | Group PK | p-value |
|---|
| (Mean ± S.D) | (Mean ± S.D) | |
| Age (years) | 25.4 ± 2.2 | 24.6 ± 2.5 | 0.24 (NS) |
| Weight (kg) | 46 ± 7 | 46 ± 5.6 | 0.83 (NS) |
| Heart Rate (bpm) | 78.4± 8.8 | 77.1± 7.9 | 0.54 (NS) |
| Systolic BP (mm Hg) | 122.3±1.67 | 125.1±1.45 | 0.22 (NS) |
| Diastolic BP (mm Hg) | 82.2±1.34 | 80.87±1.31 | 0.48 (NS) |
| Oxygen Saturation (%) | 99.07±0.26 | 99.57±0.17 | 0.12 (NS) |
p<0.05, NS: not significant, S: significant
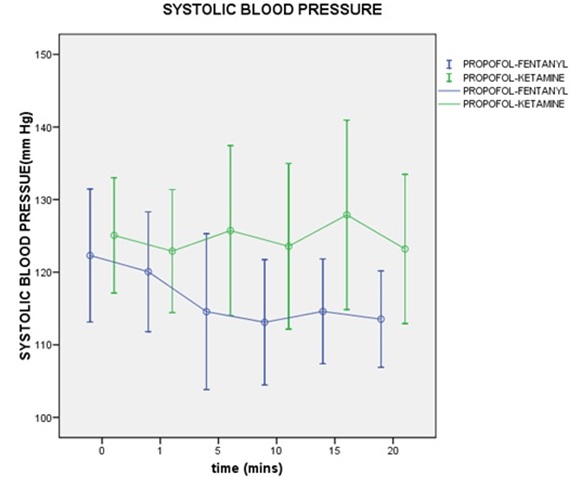
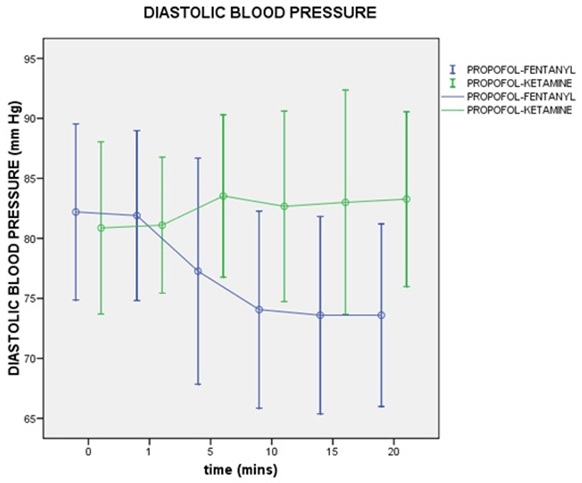
HR, SBP and DBP values did not show significant variations from the baseline recordings at any time during anaesthesia, in the PK group. Patients in the PF group showed reductions in the HR, which was not statistically significant, but reductions which occurred in the SBP and DBP from the fifth and tenth minutes respectively were significant [Table/Fig-2,3]. None of the patients had hypotension or bradycardia beyond 20% of the baseline values. Seven out of 30(23.3%) patients in PF group experienced a fall in SPO2 upto 92%, in spite of oxygen being supplemented, which was significant between the groups [Table/Fig-4]. These patients were treated with jaw thrust and chin lift. There were no incidences of desaturation which were <90%, which required airway placement. Ninety percent of patients in the group PK, in comparison to 60% of patients in group PF, had adequate surgical conditions [Table/Fig-4]. In these patients, the number of times bolus was administered was more in PF group than in PK group (3 versus 1). There was no statistically significant difference in the time, from stopping the propofol infusion, to eye opening and to following verbal commands in these groups [Table/Fig-5]. The mean time in PF group was 8.26± 2.9 (minutes) and that in PK group was 9.7±5 (minutes).
Systolic blood pressure over time
Diastolic blood pressure over time
Frequency of specific Intra operative events
| Event | Group PF (n=30) | Group PK (n=30) | p-value (Significance) |
|---|
| Desaturation | 7 | 0 | Significant |
| Patient Movement | 12 | 3 | 0.01(S) |
p<0.05, NS: not significant, S: significant
Time delay after stopping propofol Infusion to specific recorded events. p<0.05, NS: not significant, S: significant
| Event | Group PF (n=30) | Group PK (n=30) | p-value (Significance) |
|---|
| (Mean ± S.D) | (Mean ± S.D) | |
| Eye Opening (in Mins) | 8.2±6 3 | 9.7± 5 | 0.21 (NS) |
| First request for analgesia (in Hrs) | 4.4 ±0.9 | 5.2± .1 | 0.000(S) |
| Breast feeding (in Mins) | 48.4 ±12.5 | 43.3±11.1 | 0.11(NS) |
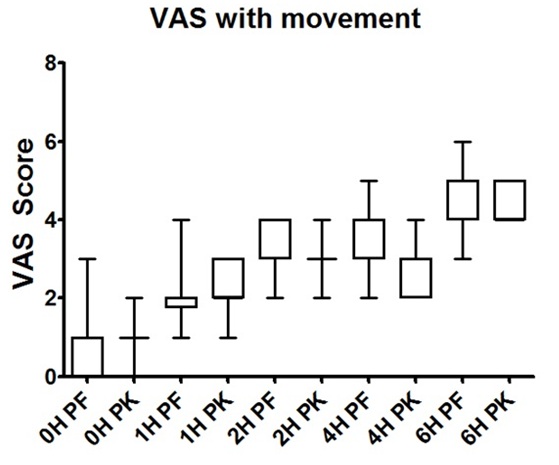
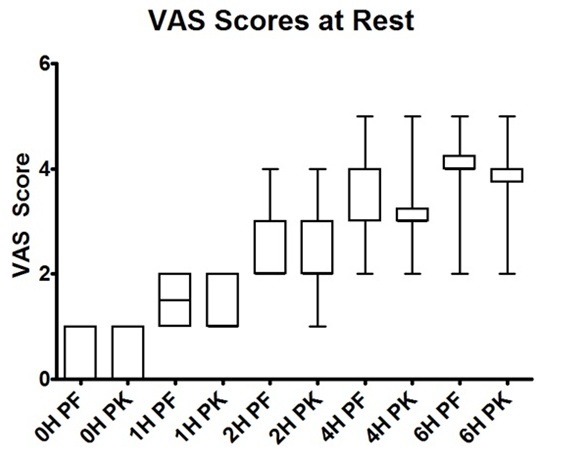
There was no difference in the already expanded in left side of page 2, line 9 visual analogue scale (VAS) scores for pain at rest and movement between the groups at recovery. However, a statistically significant difference was observed at second hour on movement and at fourth hour, both at rest and on movement [Table/Fig-6,7]. The observed mean time when first analgesia was given in the post-operative period was 4.4±0.9 (hours) in PF group and it was 5.2±0.1 (hours) in PK group, which was statistically significant (p< 0.05) [Table/Fig-5]. The sedation scores obtained during the post-operative period, showed no significant difference between the median sedation scores at recovery and at the first and sixth post-operative hours. Median sedation scores obtained at second hour were 4(PF) and 3(PK) and those obtained at fourth hour were 3(PF) and 2(PK). This difference was statistically significant.
There was no statistically significant difference in the scores of mother handling the baby [Table/Fig-8] and the time when mother was able to breast feed the baby in the post-operative period [Table/Fig-5]. The mean time in PF group was 48.4 ±12.5 (minutes) and it was 43.3±11.1 (minutes) in PK group. There was no difference in PONV in both the groups. No patients experienced any bad dreams or hallucinations.
Sedation score: Assessment was done by a scoring system - a score of “0” if the mother was alert and comfortably handled the baby, “1” if there was mild discomfort but mother was able to handle the baby and “2” if the mother was unable to handle the baby due to pain or sedation [Table/Fig-9].
Adequacy of mother handling baby
| Time | Group PF, n=30 | Group PK, n=30 |
|---|
| Score= 0 | Score= 1 | Score= 2 | Score= 0 | Score= 1 | Score= 2 |
| At recovery | 0 | 0 | 30 | 0 | 0 | 30 |
| 1st hour | 0 | 8 | 22 | 0 | 10 | 20 |
| 2nd hour | 5 | 20 | 5 | 9 | 18 | 3 |
| 4th hour | 10 | 20 | 0 | 17 | 13 | 0 |
| 6th hour | 15 | 15 | 0 | 20 | 10 | 0 |
p<0.05, NS: not significant, S: significant
Median post operative sedation scores
| Time | PF | PK | Significance |
|---|
| At recovery | 5 | 5 | NS |
| 1st hour | 4 | 4 | NS |
| 2nd hour | 4 | 3 | Significant |
| 4th hour | 3 | 2 | Significant |
| 6th hour | 2 | 2 | NS |
P<0.05, NS: not significant, S: significant
Discussion
An ideal anaesthetic technique which is used for mothers who undergo puerperal sterilizations should provide adequate depth of anaesthesia, analgesia and muscle relaxation for a short period of time and it should also ensure rapid recoveries. Good residual postoperative analgesia and minimal sedation which ensure satisfactory handling of the baby by the mother, are essential pre-requisites.
The combination of propofol and fentanyl which is used for short procedures, is quite popular and is accepted widely. Fentanyl provides adequate analgesia, which extends into the post-operative period too, while minimally affecting the psychomotor functions. Propofol provides an adequate plane of anaesthesia. Our concern with this combination was the possibility of a respiratory and a haemodynamic compromise, since both fentanyl as well as propofol are known to cause respiratory depression and a fall in blood pressure. In our current study, patients of the PF group recorded falls in heart rate and blood pressure during anaesthesia. Additionally, oxygen desaturation requiring maneouvers like jaw thrust and chin lift occurred in patients who received fentanyl in combination with propofol. The incidence of desaturation was statistically significant and it occurred despite giving oxygen supplementation. These patients responded to maneouvers like jaw thrust and chin lift.
Propofol, like other sedative drugs such as barbiturates and benzodiazepines, cannot be used as sole agent for providing anaesthesia, as it lacks analgesic activity. The dose of propofol which is needed to prevent patient movement intraoperatively, when it is used alone, is large and it is associated with significant impairments in cardio respiratory functions. Narcotics can reduce the required dose of propofol, but the risks of respiratory depression and hypotension are unacceptable.
Ketamine, in contrast, offers better haemodynamic stability and it produces lesser effects on respiration. Ketamine has been used with propofol for both general anaesthesia and IV sedation. The theoretical benefits obtained on combining propofol with ketamine are several. There is synergism between propofol and ketamine when they are used for induction of general anaesthesia in female patients and therefore, the requirements of propofol are reduced when it is used in combination with ketamine [4]. The difference in the doses of propofol which were used in the two groups in this study reflected this observation.
Several investigators, in various studies which were done, found that the co administration of ketamine with propofol during induction prevented the adverse haemodynamic outcomes which were seen when propofol was used alone [5,6]. Several strategies, including IV administration of 0.5 mg/kg ketamine prior to propofol induction and infusion, have been shown to decrease adverse haemodynamic events which were associated with isolated use of propofol [5]. We recorded the haemodynamic parameters in patients who received propofol ketamine combination and compared the incidence of adverse events seen in this group with that which was seen in patients who received propofol fentanyl combination. None of the patients in the PK group recorded any significant change in BP or HR. Patients who received PF recorded significant drops in BP and HR after the onset of anaesthesia.
Ketamine, when it was used alone, was associated with serious problems such as laryngospasms, excessive secretions and cough. On the positive side, for ketamine is the maintenance of muscle tone and thus the airway. The addition of propofol has been shown to abolish the unwanted side effects of ketamine, while preserving the airway tone [1,7]. Our study supports this observation. None of the patients who received propofol ketamine had any episodes of oxygen desaturation, airway obstruction or apnoea. This was in contrast to the patients who received fentanyl propofol, a significant number of whom had oxygen desaturation caused by airway obstruction. Literature suggests that such positive outcomes seen in the respiratory parameters are primarily owed to ketamine [1]. In a study which compared propofol alone with propofol and ketamine, a higher incidence of desaturation was seen in the propofol only group [8]. Co administration of ketamine with propofol was found to improve ventilation, normalize the end expiratory PaCO2 and to lessen the incidence of apnoea and respiratory distress [5,9,10]. Ketamine was also found to attenuate propofol induced hypoventilation in adults during Monitored anaesthesia care [9].
Reports suggest that propofol could be effective in eliminating the side effects of subanaesthetic doses of ketamine in humans [11].In addition, co- administration of low dose ketamine is known to produce positive mood effects without bringing about perceptual changes and it may also provide an earlier recovery of recognition [9]. Side effects which limit the total dose of ketamine are emergence of psycho mimetic reactions (dreaming, delirium and hallucinations), increased secretions and delayed recoveries. The patients who received propofol ketamine combination in our study did not report emergence of any of the reactions which were associated with ketamine. Satisfactory surgical conditions with adequate muscle relaxation were present in 60% of patients in PF group and in 90% of patients in PK group. In either group (30 patients each), the number of times bolus was administered was found to be more in PF group then in PK group (3 versus 1). This could be attributed to the complementary effects of propofol and ketamine, wherein propofol provides better muscle relaxation, while ketamine contributes towards superior analgesia, resulting in a balanced anaesthesia. Similar studies done by other authors also suggested that a combination of propofol and ketamine, as against propofol when it was used as a sole agent, guaranteed better operating conditions and prevented movement of the patients during surgery [5,8]. Also, the patients required fewer numbers of boluses [6,12].
In our study, all patients were equally sedated at awakening and at 1st postoperative hour. But at 2nd and 4th hours, patients of group PF were more sedated as compared to those of group PK. Propofol induced sedation may be related to a generalized neural inhibition. Subanaesthetic doses of ketamine also produce a dose dependent impairment, but ketamine, in sedative doses, is associated with EEG activation and it increases arousal [13]. Our data suggest that sedative effects of propofol may be partially antagonized by the arousal effects of ketamine. This is consistent with literature reports, that suggest that patients who receive propofol and ketamine show better vigilance as well as better pain relief post-operatively and that patients who receive fentanyl along with propofol tend to be sedated and that they have inadequate analgesia [2,9].
The mean time for the request for analgesia in the post-operative period was earlier in group PF as compared to that in group PK (4.4 hr in PF versus 5.2 in PK). In previous studies, fewer patients who received propofol and ketamine had required rescue doses of analgesics as compared to those who had received propofol and fentanyl [2,9,11]. Our results were consistent with those of previous studies, that suggested that small doses of ketamine, an N-methyl-D-Aspartate antagonist, may exert a prolonged antinociceptive effect in the postoperative period. In further support of this, we found that pain scores obtained on using visual analogue scale revealed lower VAS scores on movement in the 2nd hour of post-operative period and at rest and on movement at 4th postoperative hour in the PK group as compared to those in PF group. In the immediate post-operative period, none of the patients were able to handle their babies, as they were sedated. In the subsequent postoperative period, the abilties of mothers in handling their babies were comparable between the two groups. Mothers of group PK had no discomfort, while those in the group PF had mild discomfort, but they were still able to handle their babies and breastfeed them. There was no difference in PONV in both the groups in our study. None of them had vomiting and no patient received antiemetics. Studies have shown that as the dose of ketamine increases, there is an increase in the occurrence of PONV [1].
Conclusion
The combination of propofol and ketamine has several benefits due to their complementarily of actions. This is superior to propofol fentanyl combination in terms of haemodynamic stability, absence of respiratory depression, post-operative analgesia and recovery. Our findings suggest that propofol ketamine combination could be a good choice for anesthetizing postpartum women for sterilization.
p<0.05, NS: not significant, S: significant
p<0.05, NS: not significant, S: significant
p<0.05, NS: not significant, S: significant
P<0.05, NS: not significant, S: significant