Primary Abdominal Pregnancy in the Uterosacral Ligament with Haemoperitoneum: A Near Miss
Sirisha Rao Gundabattula1, Manjula Pochiraju2
1Consultant, Department of Obstetrics and Gynaecology,Fernandez Hospital,Hyderabad, India.
2Consultant, Department of Obstetrics and Gynaecology,Fernandez Hospital,Hyderabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. Sirisha Rao Gundabattula, 4-1-1230, Bogulkunta, Hyderabad – 500001, India.
Phone: 09052595013,
E-mail: drgsirisharao@gmail.com
Primary abdominal pregnancy has a higher mortality rate than other ectopic gestations. Delayed diagnosis can be associated with catastrophic haemorrhage. This report describes a spontaneous conception which occurred in the uterosacral ligament in a woman with no known risk factors for an ectopic pregnancy. Extrauterine pregnancy was diagnosed by ultrasound and laparoscopy was performed secondary to haemoperitoneum, which revealed a pregnancy implanted in the right uterosacral ligament. The rarity of this condition signifies the need for reporting all cases to facilitate future research and clinical management.
Ectopic pregnancy, Acute abdomen, Primary peritoneal pregnancy, Haemoperitoneum, Laparoscopy
Case Report
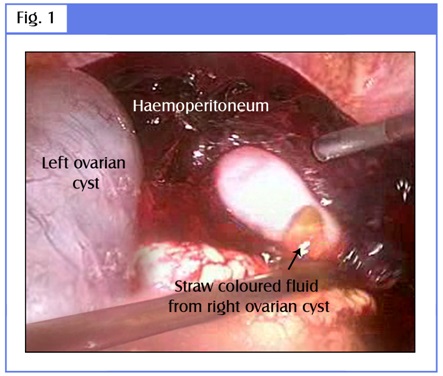
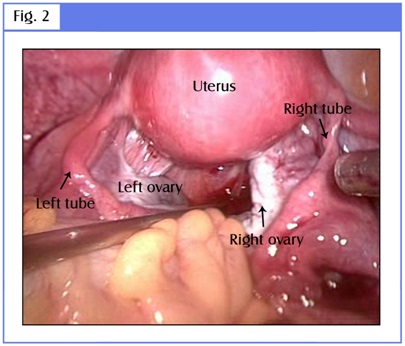
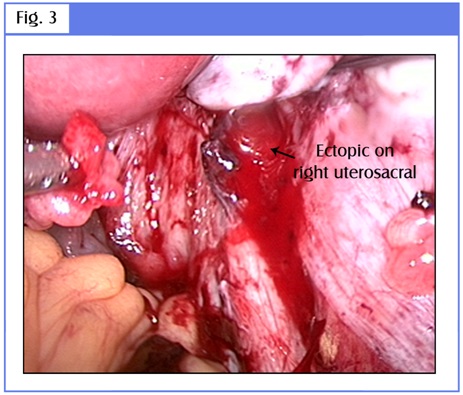
A 30-year-old lady, G3P1L1A1 presented with a one-day history of right-sided lower abdominal pain and giddiness, of one day’s duration. There was no preceding amenorrhoea. Examination revealed mild pallor and normal vital signs. Cervical movements were tender. Ultrasonography revealed a normal uterus and bilateral anechoic ovarian cysts (30 and 50 mm in right and left ovary respectively). A 20 x 16 mm echogenic right adnexal mass with a 2 mm viable embryo was noted in the pouch of Douglas. There was free fluid in the pelvis and minimal fluid in Morrison’s pouch. Investigations revealed haemoglobin level of 9.2 gm/dL and serum Beta human chorionic gonadotropin (hCG) level of 5699 mIU/mL. With a provisional diagnosis of a right tubal ectopic pregnancy, she was taken up for emergency surgery. Laparoscopy disclosed haemoperitoneum which amounted to ~1000ml. Both ovaries were enlarged and had simple cysts [Table/Fig-1]. Both fallopian tubes were found to be normal [Table/Fig-2]. The ectopic pregnancy was localized in the right uterosacral ligament, close to its uterine attachment. It measured 20 x 20 mm and there was active bleeding from this site [Table/Fig-3]. Hydrodissection was used and the products of conception were removed laparoscopically. Bipolar diathermy was applied to secure haemostasis. A single dose of parenteral methotrexate 50 mg/m2 was administered postoperatively. Histopathologic examination of the tissue from the site of ectopic pregnancy showed chorionic villi. Serum Beta hCG level dropped to 81 mIU/mL, a week later.
Bilateral ovarian cysts with haemoperitoneum
Ectopic pregnancy implanted in the right uteroscacral ligament
Characteristics of women with uterosacral ligament implantation NA – Not available
| Characteristic | Lo & Lau [8] | Lo & Lau [8] | Shin et al., [11] | Dasari & Devi [12] | Cheung & Rosenthal [13] | Park & Shin [14] | Present Case |
| Age (years) | 33 | 32 | 28 | 22 | 24 | 24 | 30 |
| Obstetric formula | G1 | G4 P2 | G2 A1 | G2 P1 | NA | NA | G3 P1 A1 |
| Risk factor | Endometriosis | None | None | Intrauterine device | None | None | None |
| Amenorrhoea (weeks) | 6 | 7 | 8 | NA | NA | 5 | None |
| Serum Beta hCG (mIU/mL) | NA | NA | NA | NA | 1654 | NA | 5699 |
| Treatment modality | Laparotomy | Laparoscopy | Laparotomy | Laparotomy | Laparoscopy | Laparoscopy | Laparoscopy |
Discussion
An abdominal pregnancy is a form of ectopic pregnancy which is implanted within the peritoneal cavity, outside the fallopian tube and ovary and which is not located in the broad ligament. Its incidence is reported to be 10.9/100,000 pregnancies and 9.2/1000 ectopic pregnancies [1] . Pregnant women with advanced maternal age may be at an increased risk of extra-tubal gestations [2] . The mortality rate associated with early abdominal pregnancies can be as high as 30/1000 [3] .
Abdominal pregnancies result from secondary implantation of aborted tubal pregnancies or intra-abdominal fertilization of sperms and ova. Our patient fulfilled the criteria for diagnosis of primary abdominal pregnancy put forth by Studdiford: pregnancy related exclusively to the peritoneal surface (early enough to eliminate the possibility of a secondary implantation after a primary tubal nidation), normal tubes and ovaries and no evidence of a uteroperitoneal fistula [4] . As the original site of implantation may be hard to determine, the original criteria were subsequently modified, to include only pregnancies which had completed less than 12 weeks of histologic gestation [5] .
Risk factors for abdominal pregnancy include tubal damage pelvic inflammatory disease, endometriosis, intrauterine insemination, assisted reproductive techniques and use of intrauterine contraceptive devices [3,6,7]. Endometriotic spots represent a favourable site for implantation [8] . Poole et al., reviewed 225 cases of early abdominal pregnancies (which had completed less than 20 weeks gestation) from 1965 to 2009. One-fourth of them were located in the pouches surrounding the uterus (majority in the pouch of Douglas). Abdominal pregnancy was diagnosed at 9 weeks of gestation on an average, at a mean serum Beta hCG level of 15670 mIU/mL [3] . The most frequent complaint is abdominal pain [9] and other symptoms relate to the site of placental attachment. The trophoblast erodes into arterioles which lie underneath the peritoneum and can lead to massive intraperitoneal haemorrhage [8] .
The uterosacral ligament is a very rare location for a primary abdominal pregnancy. The probable pathophysiology is the occurrence of fertilization in the rectouterine pouch, where sperms are known to accumulate and where the ovum lies due to dependent flow of peritoneal fluid [10]. [Table/Fig-4] depicts the characteristics of the reported cases of pregnancies which had occurred in the uterosacral ligament. Extra-tubal implantations were not suspected preoperatively.
Treatment modalities consist of surgery, parenteral/intraamniotic methotrexate, intracardiac potassium chloride, embolization and combinations of these [3,15]. Management depends on the gestational age, site of placental attachment, patient’s condition and clinician’s experience. The Beta hCG levels do not correlate with the success of medical management. Nearly 90% of cases of early abdominal pregnancies are treated by primary surgery, because most present with haemoperitoneum and almost half of those who are treated medically subsequently need to undergo operative procedures [3].
Select first trimester patients who are diagnosed early can be managed laparoscopically [6]. Operative laparoscopy should be limited to cases in which the conceptus has not become implanted in the intestinal interstices and is not near sites which are susceptible to complications [15]. The future fertility may not be affected, as the tubes and ovaries are not directly involved in pregnancy, nor are removed during the operative procedure nor are involved in postoperative adhesion formation [9].
Prior to presenting to our institute, our patient was admitted elsewhere with abdominal pain, was diagnosed to have bilateral ovarian cysts and given symptomatic treatment. The classic clinical triad of abdominal pain, amenorrhoea and vaginal bleeding is found in only 50% of ectopic pregnancies and vigilance is key to making the right diagnosis. Extrauterine pregnancies should always be considered in the differential diagnosis of abdominal pain which occurs in women who are in the reproductive age group. The timely and appropriate use of transvaginal ultrasound and serum Beta hCG can facilitate early diagnosis and successful management by minimally invasive surgery. Had there been no evidence of intraperitoneal bleeding, we might have considered medical management and the diagnosis of a primary peritoneal pregnancy would have been missed altogether, which leads to speculation about the true incidence of this condition. It was a near miss in more than one sense: both for the patient and the fraternity of gynaecologists.
[1]. HK Atrash, A Friedge, CJ Hogue, Abdominal Pregnancy in the United States: Frequency and Maternal MortalityObstet Gynecol 1987 69(3):333-7. [Google Scholar]
[2]. M Pochiraju, K Surampudi, LR Marakani, S Dasari, SR Gundabattula, A Case Control Study Comparing Risk Factors for Ectopic Gestation in Unusual and Tubal GestationsInt J Infert Fetal Med 2013 4(1):14-7. [Google Scholar]
[3]. A Poole, D Haas, EF Magann, Early Abdominal Ectopic Pregnancies: A Systematic Review of the LiteratureGynecol Obstet Invest 2012 74:249-60. [Google Scholar]
[4]. WE Studdiford, Primary peritoneal pregnancyAm J Obstet Gynecol 1942 44:487-91. [Google Scholar]
[5]. EG Friedrich, CA Rankin, Primary pelvic peritoneal pregnancyObstet Gynecol 1968 31:649-53. [Google Scholar]
[6]. RSH Young, MC Huang, CP Chen, Successful Laparoscopic Management of Primary Abdominal Pregnancy in the Cul-de-sac.Taiwanese J Obstet Gynecol 2005 44(2):172-4. [Google Scholar]
[7]. S Kar, Primary abdominal pregnancy following intrauterine inseminationJ Hum Reprod Sci 2011 4(2):95-9. [Google Scholar]
[8]. KW Lo, TK Lau, Ectopic Pregnancy in Uterosacral LigamentJ Obstet Gynaecol Res. 1997 23(5):415-9. [Google Scholar]
[9]. JN Martin, JF McCaul, Emergent Management of Abdominal PregnancyClin Obstet Gynecol 1990 33:438-47. [Google Scholar]
[10]. D Cavanagh, Primary peritoneal pregnancyAm J Obstet Gynecol 1958 76:523-32. [Google Scholar]
[11]. JS Shin, YJ Moon, SR Kim, KT Kim, H Moon, YY Hwang, Primary Peritoneal Pregnancy Implanted on the Uterosacral Ligament: A Case ReportJ Korean Med Sci 2000 15:359-62. [Google Scholar]
[12]. P Dasari, S Devi, Primary Peritoneal Pregnancy: A Case ReportJ Obstet Gynaecol Res 2000 26:45-7. [Google Scholar]
[13]. VYT Cheung, DM Rosenthal, Abdominal pregnancyJ Minin Invas Gynecol 2005 12(1):9 [Google Scholar]
[14]. IY Park, JC Shin, A case of abdominal pregnancy implanted on uterosacral ligament.Ultrasound Obstet Gynecol 2007 30(P 29.04):561 [Google Scholar]
[15]. L Cobellis, L Stradella, EM Messalli, Contribution to the choice of therapy in abdominal pregnancyPanminerva Medica 2000 42(2):159-161. [Google Scholar]