A number of imaging techniques were investigated to assess the jaw bone invasion by tumors. There is no imaging modality that is adequately reliable when used alone [9]. Conventional radiography including PR is insensitive to early bone changes, [5,10–15] but provide accurate morphological information necessary for tumor localization and detection of structural abnormalities. However, some studies [4,8,10,16–20] have concluded that nuclear bone scan is a highly sensitive, but lack structural delineation. So it is difficult to locate the focus. Therefore, the fusion of functional and static imaging may be more accurate in defining the surgical margin than individual imaging. The purpose of the study was to evaluate the accuracy of Tc scan, PR and their combination (Tc scan/PR) for assessing jaw bone invasion by oral cancer.
Materials and Methods
Twenty patients were randomly recruited in this study from our Oral Medicine and Maxillofacial Radiology department over a period of two years. All patients provided informed consent for investigation with technetium bone scan. This study followed the ethical standards of the committee on human experimentation of the institution. All patients were evaluated for serum calcium, serum phosphorous and alkaline phosphatase to rule out diseases of bone or systemic diseases influencing bone. None of our patient had diseases of bones, especially of jaw bones. All female patients were investigated for pregnancies. None of our female patient was pregnant. The histopathological diagnosis in all cases was squamous cell carcinoma except one who had osteosarcoma of mandible and was, therefore, excluded. The remaining 19 patients were evaluated for presence and extent of jaw bone cancerous invasion by clinical examination and on PR and Tc scan. The data was gathered prospectively but evaluated retrospectively. They consisted of 16 males and 3 females, aged 32 to 80 (mean 56) years. [Table/Fig-1] shows sites and TNM staging of the cancers. None of the patient had recent history of dental extraction, radio or chemotherapy. Each patient had oral cancer that was in, on or adjacent to the jaw bones.
Comparative assessment of jaw bone invasion by oral carcinoma using Clinical, PR, Tc scan, Tc scan/PR and Histopathological findings
| Patient No. | TNM Staging | Site | Clinical bone Invasion | PR finding | Tc scan finding | Tc scan/PR finding | Histologic finding |
|---|
| Corresponding to lesion | Bone invasion | Uptake | Bone invasion |
|---|
| 1 | T3N2M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 2 | T4N2M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 3 | T4N2M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 4 | T3N3M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 5 | T2N1M0 | Vestibular mucosa | Suspected | NAD | - | ↑ | + | + | + |
| 6 | T2N2M0 | Vestibular mucosa | Suspected | NAD | - | ↑ | + | + | + |
| 7 | T3N2M0 | Vestibular mucosa | Suspected | Well defined XL | + | ↑ | + | + | + |
| 8 | T2N0M0 | Buccal mucosa | Not suspected | NAD | - | NAD | - | - | - |
| 9 | T2N2M0 | Floor of mouth | Suspected | Apical dental disease | - | ↑ | + | - | - |
| 10 | T1N1M0 | Vestibular mucosa | Suspected | Apical de/ntal disease | - | ↑ | + | - | - |
| 11 | T3N1M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 12 | T2N1M0 | Vestibular mucosa | Suspected | NAD | - | ↑ | + | + | + |
| 13 | T1N1M0 | Gingiva | Suspected | NAD | - | ↑ | + | + | + |
| 14 | T3N2M0 | Floor of mouth | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 15 | T1N1M0 | Floor of mouth | Not suspected | Ill-defined XL | + | ↑ | + | + | + |
| 16 | T3N2M0 | Tongue | Not suspected | NAD | - | NAD | - | - | - |
| 17 | T1N0M0 | Vestibular mucosa | Suspected | NAD | - | NAD | - | - | - |
| 18 | T4N2M0 | Gingiva | Suspected | Ill-defined XL | + | ↑ | + | + | + |
| 19 | T2N1M0 | Floor of mouth | Not suspected | Ill-defined XL | + | ↑ | + | + | + |
The radiographic examination and the nuclear bone scan were performed on the same day or within 48h of each other. Bone scintigraphy was performed with a dual head gamma camera equipped with a parallel hole collimator. A dose of 10 to 20mCi (370 to 740 MBq) of technetium-99m methylene diphosphonate (99Tcm MDP) was injected intravenously and imaging was performed three hours later. Anterior and lateral projections of maxillofacial skeleton were performed. All 19 patients had undergone surgical excision of the tumor. 11(57.9%) patients had segmental bone resection and remaining 8 (42.1%) had marginal resection of the bone. Each surgical specimen was decalcified and sectioned for histopathological examination for final confirmation of bone invasion and its extent. First, bone scan and PR were assessed independently to check out their efficacy when used alone. Tc scans were evaluated by a nuclear medicine physician and PRs were interpreted by an oral radiologist. Here, bone invasion was considered positive when there was an increased or abnormal activity corresponding to the clinical site of the tumor. In second part, bone involvement was assessed on Tc scan/PR using diagnostic criteria by same interpreters together. In all three analyses, both interpreters were kept blind from clinical information. To evaluate the efficacy of outlined criteria on Tc scan/PR, all results including clinical were compared with the histopathological findings.
Lewis-Jones’s Diagnostic Criteria for Jaw Bone Invasion on TC Bone Scan/PR [
6]
If the site of the tumor corresponded to the site of the dental disease, then site and size of uptake on scintiscan compared with the site and size of the dental disease on PR.
Bone invasion was considered positive when PR and/or scintiscan revealed an asymmetrical or increased activity in the area of jaw bone which corresponded to the clinical site of the primary tumor, and where PR demonstrated no evidence of dental disease. If the site of the tumor corresponded to the site of the dental disease, it was considered positive only when there was an increase in size of the uptake on scintiscan compared to the actual size of the dental disease on PR.
Bone invasion was considered absent when both PR and scintiscan showed no evidence of abnormal activity corresponding to the site of the tumor.
Modification: Following points are also taken into consideration
The intensity of uptake by cancer invasion is always higher than of chronic periapical or periodontal foci.
Oral Cancer enters the jaw bone at the point of contact, which is often at the junction of the attached and reflected mucosa.
Results
Comparative evaluation of the efficacy of clinical, PR, Tc scan and Tc scan/PR with histopathological findings in determining the jaw bone invasion by SCC is shown in [Table/Fig-1]. The diagnostic accuracy of Clinical findings, PR, Tc scan alone and with PR according to the gold standard (microscopic examination) are shown in [Table/Fig-2,3,4and5]. Tc scan/PR had higher sensitivity (100%), specificity (83.3%), accuracy (94.7%), PPV (92.8%) and NPV (100%) than PR and Tc scan alone (69.2%, 83.3%, 73.6%, 90%, 55.5% and 100%, 50%, 84.2%, 81.2%, 100% respectively) as well as clinical findings (92.3%, 50%, 78.9%, 80% and 75%).
Diagnosis for bone invasion using Clinical Assessment
| TP | TN | FP | FN | Total |
|---|
| 12 | 3 | 3 | 1 | 19 |
| Accuracy of Clinical Assessment |
| Sensitivity | Specificity | Accuracy | PPV | NPV |
| 92.3% | 50% | 78.9% | 80% | 75% |
Diagnosis for bone invasion using PR
| TP | TN | FP | FN | Total |
|---|
| 9 | 5 | 1 | 4 | 19 |
| Accuracy of PR |
| Sensitivity | Specificity | Accuracy | PPV | NPV |
| 69.2% | 83.3% | 73.6% | 90% | 55.5% |
Diagnosis for bone invasion using Tc scan alone
| TP | TN | FP | FN | Total |
|---|
| 13 | 3 | 3 | 0 | 19 |
| Accuracy of Tc scan alone |
| Sensitivity | Specificity | Accuracy | PPV | NPV |
| 100% | 50% | 84.2% | 81.2% | 100% |
Diagnosis of bone invasion using Tc scan/PR
| TP | TN | FP | FN | Total |
|---|
| 13 | 5 | 1 | 0 | 19 |
| Accuracy of Tc scan/PR |
| Sensitivity | Specificity | Accuracy | PPV | NPV |
| 100% | 83.3% | 94.7% | 92.8% | 100% |
TP = true positive, TN = true negative
FP = false positive, FN = false negative
PPV = positive predictive value
NPV = negative predictive value
Discussion
One of the treatment modality of oral cancer is surgery consisting of marginal and segmental bone resection. Politi et al., suggested that the cases most suitable for marginal resection are those with no bone invasion, but requiring bone removal to ensure good tumor margins because of the proximity of the cancer to the jaw [21]. Tumor enters the mandible at the point of contact, which is often at the junction of the attached and reflected mucosa, [22] leading to acceptance of the view of marginal resection. The erosion pattern of the disease is associated with shallow mandibular invasion, or invasive bone defects confined to a superficial area of the alveolar bone [22,23], they stated that marginal resection was thought effective. Ideally, the resected margin in the bone and soft tissues should be clear of tumor by at least 5mm [24]. Close resection of margins of tumor within 5mm of the edge, were associated with high incidence of early recurrence and poor prognosis [25]. Therefore, preoperative information concerning the extent of jaw bone invasion is a most important issue.
CT (computed tomography) was anatomical imaging modality, provides accurate morphological information necessary for tumor localization and detection of structural abnormalities, but can not reflect the functional or metabolic activity of the tumor [26]. Yamamoto et al., [27] reported that, only 5 of the 13 patients in whom histopathology revealed mandibular invasion were identified on CT, while in 9 patients, the CT image was obscure because of dental artifacts. Shaha [28] confirmed that CT is not very useful in detecting bone invasion because of the presence of irregular dental sockets. Furthermore, dental amalgam artifacts and beam-hardening artifacts from the dense mandible may obscure CT imaging [29]. The specificity of MRI was significantly lower than that of CT due to chemical shift artifact by bone marrow fat that obscured the black line of the cortex [30,31]. The subset of ferromagnetic metals and certain other metals causing radiofrequency and power tissue maldistribution cause artifacts on MRI [29]. Another disadvantage of MRI is its susceptibility to motion artifacts by tongue movement and swallowing. However, CT is useful when there is gross involvement of bone as well as soft tissue but less successful in early bone invasion or new periosteal bone formation.
Some investigators recommend using two or more modalities that can complement each other. Clinical judgment and conventional radiographs are accurate in cases when there is gross involvement of bone (17 of 19) but are significantly less successful in determining early bone invasion [11]. However, a combination of panoramic radiography and bone scintigraphy is recommended in early invasion [32].
Another important clinical parameter was fixation of tumor to underlying bone. Tumor fixation to bone was present in 14 cases, we found 13 true positive. False positive case was on the oral floor and seems to be attached to the lingual cortex. In a study by Caroline et al., [9], clinical assessment results in overdiagnosis leading to high sensitivity and low specificity. Clinical evaluation was little overestimated in our case and most importantly not able to determine the correct extent of bone involvement. But it gave more useful information regarding tumor, its site, size, proximity and fixation with underlying bone for diagnosis and treatment planning.
The determination of clinical bone invasion largely depends on the proximity (P) and fixity (F) of the tumor with the bone. In addition, high T-value (T) favors it because larger the size higher the chance of contact. Higher the PFT higher is the chance of bone involvement. Tumor cells usually follow least resistance pathway; hence bone invasion through dense cortical margin usually happens last except in high PFT. Bone invasion is unrelated to nodal involvement. Accuracy of clinical assessment in terms of bone involvement (sensitivity 92.3%, specificity 50%, accuracy 78.9%, PPV 80%, NPV 75%) was almost similar with plain Tc scan. Clinical examination especially the intraoperative one after periosteal stripping as described by Brown et al., [33] is accurate in detecting bone invasion but has disadvantage of low specificity. It is also affected by irregular dental sockets due to periodontitis.
In our study, hybrid Tc scan/PR was used with Lewis-Jones’s diagnostic criteria [6] to evaluate bone invasion by oral cancer. Its specificity, accuracy and PPV were higher than single Tc scan. Our study showed 50% specificity, 84.2% accuracy and 81.2% PPV with Tc scan but 83.3% specificity, 94.7% accuracy and 92.8% PPV using Tc scan/PR. Lewis-Jones et al., [6] reported 100% sensitivity, 100% NPV, 86% specificity and 92% PPV by using combination of these two complementing modalities. In another study, the accuracy of bone scinitigraphy was 100% (36 of 36 patients) in determining the full extent of tumor involvement in jaw bones [34]. Some studies found that combination of real and rear time imaging was more precise over single modality [6, 11, 13, 19, 32, 35]. Sensitivity and NPV obtained by us were 100% with Tc scan when used either alone or in Tc scan/PR compared to PR alone (69.2%, 55.5%). The low sensitivity and NPV of PR is because of its anatomic (static) rather than functional radiography and sufficient demineralization or remineralization (36%) is required to be visible on conventional radiograph. PR is a tomograph so early changes in the structure outside or inside the focal trough will not be noticed; furthermore it is a two dimensional view of three dimensional object leading to superimposition on the smaller changes. The values of PR is further restricted because of double images, ghost shadows, thin anterior focal trough and cervical superimpositions. Some studies found PR specific for revealing periapical or periodontal infections that may be misinterpreted by other imaging modalities [13,14]. With histological findings as the standard of reference, PR was found to be 100% specific in a study carried out on 15 patients [20]. A negative Tc scan rules out bone invasion (100% sensitivity, 100% NPV). We assessed 5 of 6 patients correctly on Tc scan/PR as not having bone involvement.
Weisman et al., [4] found a 53% false positive rate with bone scintigraphy as a result of mandibular inflammatory changes. Gilbert et al., [10] also showed that the false positive rate with bone scintigraphy was 50% (3/6). We had 50% of false positive rate with bone scintigraphy but it was reduced to 16.7% when scintiscan used with PR under outlined criteria. Our specificity with Tc scan/PR was relatively low (83.3%) partly because our patient population without bone invasion was small (6 of 19 patients).
There were three false positive cases when bone scintigraphy used alone because of corresponding dental diseases. Two of them were correctly identified by outlined criteria as there was no increase in size of the uptake on scintiscan corresponding to the actual size of the dental diseases on PR. Chan et al., [36] suggested that lesion to non-lesion ratio (uptake) in mandibular invasion by using Tc SPECT were significantly higher than in those with normal mandible or dental disease. But the third patient had severe periodontal bone loss associated with large apical ill-defined rarefying ostitis corresponding to the site of the tumor and was, therefore falsely identified as positive even on Tc scan/PR. In this case, we were unable to determine mandibular invasion with certainty even though the size of the uptake was equal to size of the periodontal disease on PR. This uncertainty is because severe periodontal bone loss usually opens door for overlying/adjacent tumor to invade medullary cavity. As the final radiology report suggested bone invasion, they were listed as positive for the purpose of the study. But clinically, bone invasion was not suspected as tumor was located on the mouth floor [Table/Fig-6], not immediate and fixed to the bone. This case clearly indicates the importance of clinical judgment.
Carcinoma of the Oral floor

The superficial cortical erosion is not included under definition of bone invasion which, according to accepted TNM classification, requires complete cortical penetration [37]. Bone scan can be positive even in superficial erosion as well as periosteal reaction however such involvement show microscopic invasion and should be recommended for marginal resection. In our study, the decision to proceed bone resection especially the marginal one was based on clinical and radiological evaluation and intraoperative assessment of bone invasion by stripping the periosteum.
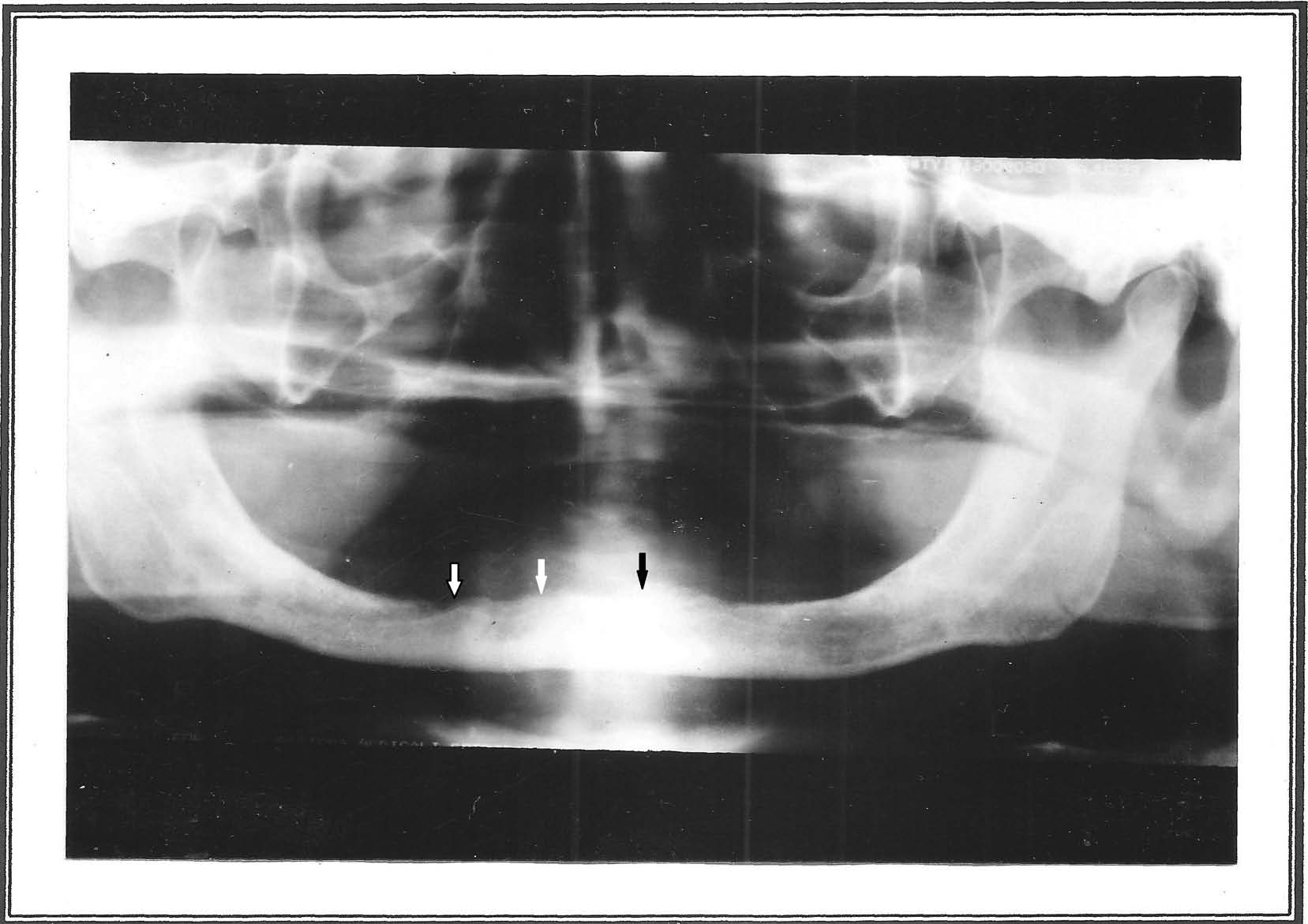
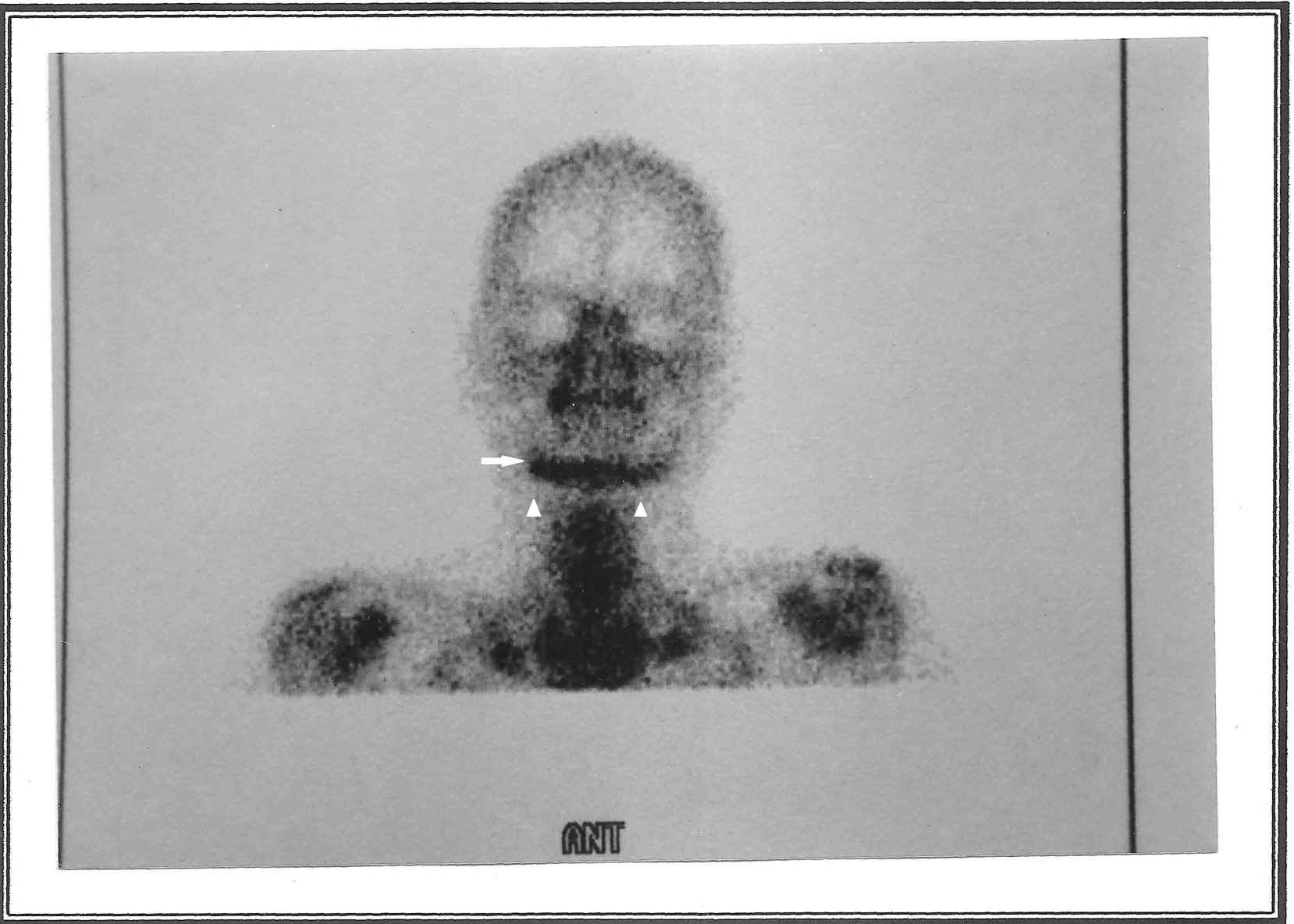
Of the 13 true positives, four were with gross bone involvement and all of them were identified on PR. The cortical penetration with cancellous bone invasion was present in 7 patients; PR was correct in 5 cases. The remaining 2 cases had superficial cortical erosion. Panoramic radiography was false negative [Table/Fig-7] but scinitiscan was true positive [Table/Fig-8] in these four cases. This indicated that the scintigraphic technique may be more sensitive in detecting early bone changes than panoramic radiography. In eight cases including four with gross involvement, the extent of lesion demonstrated by scintiscanning was greater than delineated by panoramic radiography; histopathology of resected specimen confirmed this findings. Bone scintigraphy was superior in showing correct extent of the lesion. Baker et al., [12] reported similar findings.
Panoramic radiography (PR) was negative in terms of bone invasion by the carcinoma. PR was normal (arrow) at the site of the carcinoma shown in figure one
Bone scintiscan (Tc scan) demonstrated increased uptake (arrow) in the anterior mandible corresponding to the cancer location without involving lower border (arrowheads). Bone invasion was considered positive on scintiscan and subsequent histology confirmed this finding. This case illustrates detection of bone invasion earlier with bone scintiscan than on PR
There were no instances of an abnormal radiograph with a normal bone scintigraph. In 1996, Higashi et al., [38] reported similar observation in their study. In our study, there was no false negative result on Tc scan when used either alone or in combination indicates its extreme sensitivity. But few studies with false negative results [4,17,33] were observed. Such cases may arise because of misinterpretation of adjacent or opposite side dental disease on scintiscan. Tc scan/PR using outlined criteria can be helpful in resolving such misreading. PR provides an excellent general survey of the jaws; in addition dental diseases are better diagnosed and differentiated on it. Thus, it provides complementary information regarding coincidental dental diseases and considerably increases specificity of bone scintigraphy.
Conclusion
Hybrid Tc scan/PR has high sensitivity and specificity in detecting the existence and extent of malignant bone infiltration. Although the sensitivity of Tc scan is similar to that of Tc scan/PR, the latter provides a much better delineation of the tumor and dental foci in spite of two dimensions. Based on this information, the surgical margin of the tumor can be planned and performed more precisely. Patient outcome can be improved by avoiding undertreatment and unnecessary excisions.
Future Scope
Fusion of conventional radiography along with three dimensional static and functional imaging will be an ideal fusion in detecting and differentiating cancerous bone invasion from dental foci.
TP = true positive, TN = true negative
FP = false positive, FN = false negative
PPV = positive predictive value
NPV = negative predictive value