Localized Multiple Cemental Excrescences: A Rare Presentation of Hypercementosis
Nadeem Jeddy1, Radhika T.2, Krithika C.3, Saravanan R.4, Ramachandran Prabakar5
1 Professor and Head, Department of Oral Pathology, Thai Moogambigai Dental College, Golden George Nagar, Chennai, India.
2 Reader, Department of Oral Pathology, Thai Moogambigai Dental College, Golden George Nagar, Chennai, India.
3 Reader, Department of Oral Medicine, Thai Moogambigai Dental College, Golden George Nagar, Chennai, India.
4 Professor, Department of Orthodontia, Thai Moogambigai Dental College, Golden George Nagar, Chennai, India.
5 Professor and Head, Department of Orthodontia, Thai Moogambigai Dental College, Golden George Nagar, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Radhika T., Reader, Department of Oral Pathology, Thai Moogambigai Dental College, Golden George Nagar, Chennai-600107, India.
Phone: 91-9566016165,
E-mail: radhikasashi26@gmail.com
Hypercementosis is an abnormal thickening of cementum which may be generalized or localized. Localized hypercementosis is usually characterized by nodular enlargement of apical third of root. Hypercementosis in the form of multiple cemental spikes distributed throughout the entire length of root is a very rare finding. In this article, we report such a rare manifestation of localized hypercementosis affecting right maxillary third molar in a 24-year-old male. This finding was an accidental observation following a difficult extraction procedure as the spikes were not evident in the orthopantamogram. It is imperative that every dental practitioner be aware of several presentations of hypercementosis and ensure that such an entity is considered in the differential diagnosis of difficult extraction procedures as an Intraoral Periapical (IOPA) radiograph or even an Orthopantamogram (OPG) could not differentiate the root morphology.
Hypercementosis, Localized, Cemental spikes
Case Report
A 24-year-old male patient reported to a private Dental clinic for oral prophylaxis. He also complained of pain in right lower back region due to impingement of right upper back tooth on the mucosa of the lower jaw. On intraoral examination, it was noted that 18 was impinging on the mandibular alveolar mucosa distal to 47 during occlusion. 38 and 48 were impacted. OPG revealed mesioangular impaction of both mandibular third molars. Maxillary third molars were completely erupted [Table/Fig-1]. His medical history was noncontributory and vital signs were normal. Patient did not give a history of any orthodontic treatment or any other major dental procedures. His haemogram and blood sugar values were normal.
Pre-operative panoramic radiograph showing erupted 18, 28, and impacted 38, 48. All third molars appear apparently normal in morphology

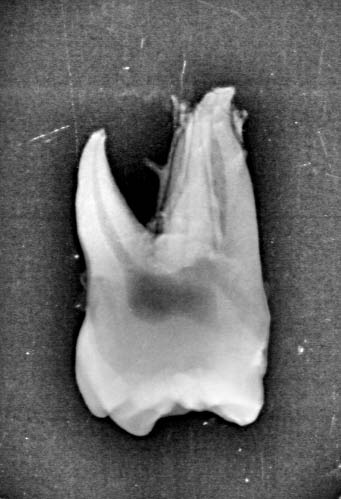
Extraction of all four third molars was planned. When extraction of 18 was attempted, there was resistance to the movement of the tooth upon traction; but it was carefully and patiently manipulated out of the socket and removed in toto. However, morphology of all third molars appeared apparently normal on the pre-operative radiograph and there was no associated pathology. The extracted tooth in this case showed multiple calcified spike like projections (6 in number) on the mesiobuccal and distobuccal roots of 18 [Table/Fig-2]. These spikes were seen on the buccal and palatal aspects as well as the middle and apical thirds of both the buccal roots; the palatal root however, did not have any cemental spikes. Intra oral digital radiograph of the extracted tooth was taken to confirm the nature of the spikes. The radiograph confirmed the presence of spike like projections which were continuous with the external surface of the root suggesting their origin from the cementum [Table/Fig-3]. The tooth showed no evidence of caries or attrition and appeared otherwise normal. Serial estimation of serum calcium, phosphorus, alkaline phosphatase, T3, T4 and TSH levels were normal. The extraction site healed uneventfully and there was no post- operative complication.
Extracted right upper third molar as viewed from the mesial aspect, showing the presence of multiple cemental spikes on the buccal and palatal aspects of the buccal roots.

Digital intra oral radiograph showing the spikes which is continuous with the cementum.
Discussion
Hypercementosis refers to an abnormal and prominent thickening of cementum. It is a form of cemental hyperplasia which can be generalized or localized. Generalized hypercementosis is characterized by increased thickness of cementum involving all teeth and is a classical feature of Paget’s disease. Other systemic disturbances associated with hypercementosis include acromegaly, arthritis, calcinosis, rheumatic fever and thyroid goiter [1].
Localized hypercementosis affects single tooth and usually presents as generalized thickening of cementum with nodular thickening of apical third of root. Cemental excrescences in the form of spikes are an uncommon condition and a rare manifestation of hypercementosis characterized by presence of small spikes or outgrowths of cementum on root surface [2].
Cementum is a calcified avascular mesenchymal tissue that forms outer covering of anatomic root of a tooth [3]. Abnormalities in the thickness of cementum can range from Cemental aplasia or hypoplasia (absence or paucity of cellular cementum) to Cemental hyperplasia or hypercementosis (excessive deposition of cementum) [1].
Hypercementosis is characterized by cementum formation beyond the physiological limits of the tooth. Hypercementosis usually occurs as a generalized thickening of the cementum with nodular enlargement of the apical third of the root. Various reasons attributed for hypercementosis include functional stress due to occlusal forces [4], continuous dental eruption [5], incorporation of periodontal cementicles during physiologic cementum deposition, reactionary deposition in response to periapical inflammatory processes as well as systemic factors such as atherosclerosis, acromegaly, deforming arthritis, hypertrophic arthritis, thyroid diseases and Paget’s disease [6]. Based on the macroscopic appearance, hypercementosis is classified as a) Club shaped b) Focal and c) Circular cemental hyperplasia [7].
Spike formation of cementum is an uncommon condition characterized by the occurrence of small spikes or outgrowth of cementum on the root surface. The occurrence of cemental spikes has been attributed to excessive occlusal stress or excessive tension from orthodontic appliance probably as a result of deposition of irregular cementum in a focal group of fibers of the periodontal ligament or coalescence of cementicles that adhere to the root or the calcification of periodontal fiber at the site of insertion into the cementum [8].
Functional stress cannot be considered as an etiological factor in our case because the opposing mandibular third molar was impacted and hence was not in occlusion with the tooth in question. Besides, unlike the first molar, a third molar seldom bears the brunt of the occlusal stress. The patient has not undergone any orthodontic treatment which again rules out tension from orthodontic appliance as an etiologic factor for cemental spikes in the present case. In tooth without antagonist, hypercementosis usually presents as nodular thickening of apical third of root and occurs as an attempt to maintain the width of the periodontal ligament and to compensate the accelerated eruption of tooth [8]. However, the present report is also a tooth without antagonist whereas hypercementosis was in the form of spikes rather than nodular enlargement of apical third of the root. The fact that these cemental spikes were not visible on the pre-operative panoramic radiograph added to our clinical dilemma during the extraction procedure. Since this patient had no obvious systemic contributory factors, the mechanism of spike formation in the maxillary third molar in this patient cannot be explained in simple terms and hence presumed to be idiopathic in nature.
Conclusion
This is a rare case of focal hypercementosis in the form of cemental spikes. Although several cases of focal hypercementosis affecting a mandibular molar have been reported in literature, our case is unique in two aspects: firstly in the nature of the hypercementosis, which was in the form of multiple spikes along the root surface and secondly in the tooth affected, which was a maxillary third molar out of occlusion with the opposing tooth.
It is mandatory for every dental practitioner to be aware of such a rare variety of localized hypercementosis. Cemental spikes, however rare or undetectable, should be considered in the differential diagnostic possibilities of any tooth that poses a considerable difficulty during extraction.
[1]. Newman Takei Klokkevold Carranza Carranza’s Clinical Periodontology: South Asia Edition 2013 1st edIndiaElsevier Publishers:35 [Google Scholar]
[2]. Rajendran R, Sivapathasundaram B, Regressive alterations of the teeth. In: Rajendran R, Sivapathasundaram B (editors)Shafer’s text book of oral pathology 2009 6th edNoidaElsevier Publishers:585-6. [Google Scholar]
[3]. Reddy Shantipriya, Essentials of Clinical Periodontology and Periodontics 2008 2nd edNew DelhiJaypee Publishers:26 [Google Scholar]
[4]. Comuzzie AG, Steele DG, Enlarged occlusal surfaces on first molars due to severe attrition and hypercementosis: examples from prehistoric coastal populations of TexasAm J Phys Anthropol 1989 78:9-15. [Google Scholar]
[5]. Azaz B, Michaeli Y, Nitzan D, Aging of tissues of the roots of nonfunctional human teethOral Surg 1977 43:572-8. [Google Scholar]
[6]. Soni NN, A microradiographic and polarized light study of cementum in Paget’s diseaseJ Oral Med 1969 24:27-30. [Google Scholar]
[7]. Pinheiro BC, Pinheiro TN, Capelozza ALA, Consolaro A, A scanning electron microscopic study of hypercementosisJ Appl Oral Sci 2008 16(6):380-4. [Google Scholar]
[8]. Newman MG, Takei H, Klokkevold PR, Fermin A, The normal periodontium. In: Newman MG, Takei H, Klokkevold PR, Fermin A (editors)Carranza’s clinical Periodontology 2007 11th edChinaElsevier: Saunders:77 [Google Scholar]