Non carious cervical lesions (NCCLs) are commonly encountered condition in clinical practice with the incidence varying between 5-85% [1]. Their prevalence and severity increases with age. The lesion characteristics range from a shallow groove to large wedge-shaped defect. The abrasive materials, acids, and occlusal stress can interact or operate separately resulting in NCCLs. However their initiation and progression is faster when all three factors are present simultaneously [2].
Restoring cervical lesions is a challenge for the clinicians. Traditional methods includes the use of non adhesive restorative materials which required extensive removal of sound tooth structure for retention [1,3]. Advances in material science have made it possible to restore these lesions with minimal tooth preparation using bonded restorations such as glass ionomer cement (GIC), resin-modified GIC (RM-GIC) or composite resins. GIC have characteristics of being truly adhesive material, release of fluoride and low modulus of elasticity [4]. However poor aesthetics, solubility particularly in acidic oral environments and fracture induced failure under parafunctional forces precludes their use as cervical restorations. The best materials to restore these lesions is micro filled composite (MC) having modulus of elasticity similar to dentin as it will thus flex and dissipate stresses. These allow micro-mechanical bonding, have the coefficient of thermal expansion closer to dentin and provides better aesthetic [5]. However their durability is confronted by gaps at tooth restoration interface due to polymerization shrinkage and weak bonding at gingival wall. Pre-treatment of cavity with acid conditioning before placing the restorative material helps to clean and improve the surface energy for better bonding [6]. Air abrasion (AA) was first described by Black as an alternative technology for tooth cutting to increase patients’ comfort by reducing pressure, heat, vibration, and noise [7]. When used as preconditioning agent it was claimed to prepare enamel surfaces in a manner similar to acid etching (AE) with the possibility of increasing adhesion [8].
Effect of AA on integrity of class V cavities restored with GIC and MC has not been compared previously. Hence the present study was planned to evaluate and compare the effect of AA as a preconditioning agent for both GIC and MC as compared to conventional preconditioning methods, without and with cyclic loading at enamel and cementum margin.
Materials and Methods
Forty freshly extracted (for orthodontic purpose) mandibular 1st premolars were used because the sound teeth need to be in this study were easily available as their extraction was most commonly indicated for orthodontic treatment. The extracted teeth were hand scaled and cleaned with slurry of flour of pumice to remove any remaining soft tissue. All teeth were stored in distilled water with 0.2% thymol at room temperature for less than 3 months before use. The study was performed at Department of Conservative Dentistry and Endodontics, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India. Simple random sampling was done to distribute teeth into the study groups.
Tooth preparation: Standard class V cavities of dimensions 5x3x3 mm were prepared on buccal surfaces of teeth using flat fissure diamond point and tapered fissure burs in an airrotor handpiece under continuous water spray. The occlusal margins were kept in enamel and the cervical margins were taken to cementum, just 1mm below the cemento-enamel junction.
Restoration: After cavity preparation all the teeth were distributed into four groups (n=10) and restored as follows:
Group I (GIC): The cavity surface was preconditioned with 10% polyacrylic acid (PAA) and restored with GIC (Ketac molar TM 3M ESPE). The restoration surface was protected by thin layer of cavity varnish. The teeth were stored in distilled water at 370C for 24 hours and restorations were polished.
Group II (AA+GIC): AA of cavities was performed with 27 μm silica particles at 80° angle with 60 psi air pressure at a distance of 1-2 mm for 5 second. Thereafter procedures as in group I were followed.
Group III (AE+MC): The cavity surface was etched with 35% Phosphoric acid (PA) followed by application of dentin bonding agent (DBA), restored with microfilled composite (MC) (Heliomolar, Ivoclar Vivadent) and cured with LED light cure unit (Ivoclar Vivadent). The contouring, finishing and polishing were accomplished with composite polishing kit (Shofu Inc., Japan).
Group IV (AA+MC): AA of cavities was performed as described previously for group II. No AE of cavities was performed prior to DBA application, cavities restored with MC. The contouring, finishing and polishing were accomplished with composite polishing kit (Shofu Co., Japan). Each group was further divided into two subgroups A & B having 5 teeth each.
Cyclic loading: All teeth in subgroup B were covered with addition silicon rubber based impression material (to simulate periodontal ligament) and placed in a custom prepared acrylic mould. Buccal cusp was subjected to the load of 60N at an angle of 200 to the long axis of tooth to simulate masticatory load on mandibular premolars. Total 1, 50,000 cycles were completed at a frequency of 4-6 cycle/sec to replicate six months of clinical usage.
All the teeth were kept in deionised water at room temperature till microleakage analysis was performed.
Microleakage analysis: For all the teeth in four groups, entire surfaces except for the restoration and 1 mm margin around it were coated with nail varnish and immersed in 2% Methylene blue dye solution for 24 hours. Teeth were rinsed under tap water, allowed to dry and mounted in light cured methyl acrylate based resin to facilitate handling. They were sectioned longitudinally into two equal halves with the help of diamond disks (Horico H557F220) under copious irrigation. The occlusal and gingival margins of cavities were examined under stereomicroscope at 20X magnification by two independent examiners blinded to groups and procedures. Staining along the tooth restoration interface was scored for dye penetration by following criteria.
0 - No penetration.
1 - Extending < ½ of preparation depth.
2 - Extending > ½ of the preparation depth.
3 - Reaching the axial wall.
Data was statistically analyzed with non—parametric Kruskal-Wallis test and Mann—Whitney U test using SPSS software version 11.5.
Results
Means and standard deviations of microleakage scores of the four groups are presented in [Table/Fig-1]. In general, microleakage at cementum margin was higher than enamel margin [Table/Fig-1]. Cyclic loading resulted into increased microleakage in all the study groups [Table/Fig-1,2and3]. Least microleakage was seen for the cavities restored with GIC alone at both enamel and cementum margins. Kruskal—Wallis test revealed no significant differences in microleakage at cementum margin among groups (p<0.05) [Table/Fig-4]. However, statistically significant difference existed on microleakage at enamel margins among the groups (p<0.05) [Table/Fig-5]. Pair wise comparisons of microleakage at enamel margins were completed by Mann—Whitney U test. Preconditioning with AA (Group II & IV) led to an increase in microleakage compared to conventional acid preconditioning and etching (Group I & III) respectively [Table/Fig-1].
Mean scores± standard deviation (SD) of microleakage at enamel and cementum margin with and without cyclic loading between the four study groups
| Group | Without cyclic loading (A) | With cyclic loading (B) |
|---|
| Enamel margin | Cementum margin | Enamel margin | Cementum margin |
|---|
| (mean±SD) | (mean±SD) | (mean±SD) | (mean±SD) |
|---|
| I | 1 ± 0.70 | 2 ± 0.70 | 1.2 ± 0.83 | 2.4 ± 0.54 |
| II | 2 ± 0.70 | 2.4 ± 0.54 | 2.4 ± 0.54 | 2.6 ± 0.54 |
| III | 2.4 ± 0.54 | 2.4 ± 0.54 | 2.6 ± 0.54 | 2.8 ± 0.44 |
| IV | 2.6 ± 0.54 | 2.8 ± 0.44 | 2.8 ± 0.44 | 3 ± 0.00 |
Calibration curve for the estimation of serum AAT concentration using standard solution of human plasma AAT
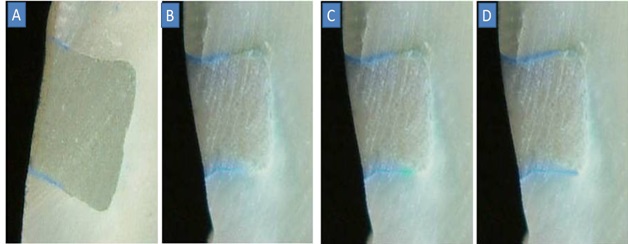
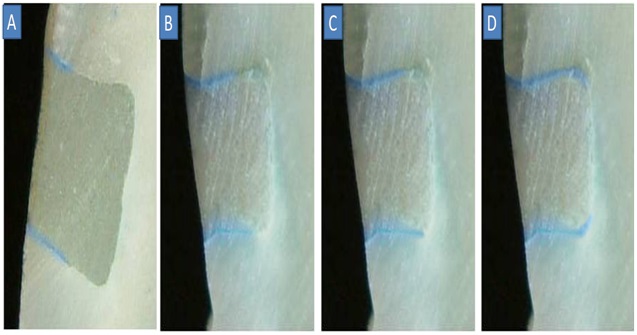
Representative photographs of microleakage at enamel and cementum margin in the four study groups with cyclic loading (A) Group I (B) Group II (C) Group III (D) Group IV
Kruskal-Wallis test for comparison between the four study groups at cementum and enamel margin without cyclic loading
| Margin | Group | n | Mean Rank | p-Value |
|---|
| Enamel | I | 5 | 4.3 | 0.03 |
| II | 5 | 10.2 |
| III | 5 | 13 |
| IV | 5 | 14.5 |
| Cementum | I | 5 | 7.3 | 0.34 |
| II | 5 | 10.3 |
| III | 5 | 10.3 |
| IV | 5 | 14.1 |
| Margin | Group | n | Mean Rank | p-Value |
| Enamel | I | 5 | 4.3 | 0.03 |
| II | 5 | 10.2 |
| III | 5 | 13 |
| IV | 5 | 14.5 |
| Cementum | I | 5 | 7.3 | 0.34 |
| II | 5 | 10.3 |
| III | 5 | 10.3 |
| IV | 5 | 14.1 |
| Margin | Group | n | Mean Rank | p-Value |
| Enamel | I | 5 | 4.3 | 0.03 |
| II | 5 | 10.2 |
| III | 5 | 13 |
| IV | 5 | 14.5 |
| Cementum | I | 5 | 7.3 | 0.34 |
| II | 5 | 10.3 |
| III | 5 | 10.3 |
| IV | 5 | 14.1 |
Kruskal-Wallis test for comparison between four study groups at cementum and enamel margin with cyclic loading
| Margin | Group | n | Mean Rank | p-Value |
|---|
| Enamel | I | 5 | 4.2 | 0.03 |
| II | 5 | 10.9 |
| III | 5 | 12.6 |
| IV | 5 | 14.3 |
| Cementum | I | 5 | 7.5 | 0.41 |
| II | 5 | 9.5 |
| III | 5 | 11.5 |
| IV | 5 | 13.5 |
Discussion
The present study evaluated marginal integrity of class V GIC and MC restorations after preconditioning with AA as compared to conventional process i.e. 10% PAA for GIC and etching with 35% phosphoric acid for composites at both, enamel and cementum margins with and without cyclic loading. A correct diagnosis with consideration of the etiology and progression of condition is a prerequisite for successful management [9,10]. “Tooth flexure theory” is accepted as primary etiologic factor in wedge-shaped cervical erosion and Class V restoration retention failure [11]. However the placement technique, properties of bonding agents, polymerization shrinkage, marginal leakage etc are enlisted as other possible causes of restoration failure [12,13].
Presence of sclerotic dentin is more common in NCCLs and is less receptive to bonding protocols [14]. Use of self-etch adhesives has been proposed over etch and rinse bonding systems that results into discrepancies between depth of mineralization and resin infiltration. However existence of a hypermineralized layer on the surface of NCCLs precludes optimal etching of sclerotic dentin by self-etching primers [15]. GIC possesses many attributes of a perfect restorative material for carious and NCCLs. It sets by acid base reaction and forms an ionic bond between the carboxyl (COO-) ions in the cement acid and the calcium (Ca++) ions in tooth [16]. Pretreatment of the dentin surface with 10% PAA facilitate its bonding with the tooth structure. In addition to calcium complexation and hydrogen bonding, adhesion of GIC to enamel surface occurs by inter crystalline bonding [16].
‘Dye penetration’ technique being a simple, inexpensive, nontoxic, traceable at low concentration, common, and comparable method was utilized for evaluation of microleakage in present study. The results demonstrated better marginal seal with GIC than with MC. Heliomolar used in the present study is a MC resin having elasticity coefficient of 12.2G Pa which tend to flex with tooth rather than debond. The use of MC minimizes polymerization contraction stresses by flow relaxation. However, heliomolar showed shear bond strength of 10.2 Mpa which is below the acceptable bond strength (17 Mpa) for a cavity with C factor equal or less than one (class V, C factor =0.2) to resist contraction stresses that develop in composite during polymerization to prevent marginal debonding [17]. Inferior marginal seal with this composite can be ascribed to the polymerization shrinkage. Although measurements of in vitro bond strengths revealed lower values for GIC compared to resin-based adhesive systems, evaluations in NCCLs restored with GICs showed good long-term retention. Similar to the results of present study, high retention rates for GIC were recorded by Gladys et al. Hence they stated GICs as the materials of choice in cervical area of teeth where no cavity preparation is contemplated [18].
Various surface conditioning methods and adhesion promoters such as roughening with burs, AA with aluminium oxide and laser have been proposed to improve the bonding [7,8,19]. AA at high pressure can roughen the tooth to increase surface area and enhance resin tag formation. It may improve bond strength of composite restoration without the need for acid-etching [19]. A better marginal seal was reported for low-viscosity polyacid modified composite resins and RM-GIC after AA [20,21]. However increased microleakage was seen for restorations placed after preconditioning with AA in the present study. Increased microleakage at enamel margins for teeth Group II & IV can be related to subsurface micro cracks and cohesive failure within the weakened enamel. Duration of AA was limited to 5 second to minimize the obstruction of dentinal tubules from residual dust layer. Furthermore, superficial maceration of collagen fibers and tearing of damaged dentin surface by polymerization shrinkage could be an explanation for increased microleakage at gingival cavity margins in Group IV [22].
Hannig by evaluating different composite resins observed that the combination of AA and etching and adhesives systems resulted in a gap-free adaptation in most cases [20]. The use of stronger acids to improve bonding to sclerotic dentin was recently challenged. The authors maintained that sclerotic dentine, being a part of the body’s natural defence mechanism, should be preserved and AE should be avoided to promote marginal integrity of resin composites [15]. The AE of air abraded cavity surface was not performed in the Group IV prior to composite restoration. However maximum score for microleakage were seen at both enamel and cementum margins in this group. These findings were similar to other studies which reported lower shear bond strength with AA when compared to conventional AE technique [21,22]. It could possibly be due to non-removal of smear layer, preventing the diffusion of monomer into superficial dentin structures and thus not allowing adequate adhesion.
An important aspect to be considered, when selecting a restorative material for NCCL, is the material’s capacity to partially absorb and resist the tension generated during load distribution through the tooth [23]. Cyclic loading had deleterious effect on the restoration-tooth margin and increased the microleakage of both; GIC and MC restorations. When teeth are subjected to mechanical stress, because of difference in modulus of elasticity of tooth and restoration, the integrity of restoration-tooth margin deteriorates over a period of time [3,10,24,25]. Use of lasers for cavity preparation has not shown any improvement in microleakage sealing when compared to the conventional diamond bur preparation, highlighting the importance and need of suitable restorative material [26]. The use of silorane based composites has also been suggested for restoration of class V cavities in a recent study [27].
The present study substantiated the results of previous studies that AA alone as a preconditioned was ineffective and showed higher microleakage as compared to conventional methods. Probably it could have enhanced the marginal bond, if it was followed by conventional conditioning agents.
Conclusion
The microleakage in class V was universally more at cementum margins than at enamel margins and with loading than without loading. AA as a preconditioning agent was not found effective in producing good tooth-restoration bonding, both for GIC or MC restorations. Since the acid etching of cavity was not done before restoring with composite, it could be considered as the limitation of study. Further studies can be planned to evaluate the cumulative effect of Air abrasion and acid etching on the microleakage of composite restoration using conventional and newly introduced composite materials.