Diffuse Osteoradionecrosis of Temporal Bone as a Late Complication of Adjuvant Radiotherapy to Parotid Bed: A Case Report
Sisha Liz Abraham1, Sivaraman Ganesan2, Elizabeth Mathew Iype3, Vijay Jagan4
1 Fellow in Head and Neck, Department of Surgical Oncology, Regional Cancer Center, Trivandrum, India.
2 Assistant Professor, Department of Ear, Nose and Throat, JIPMER, Pondicherry, India.
3 Additional Professor, Department of Surgical Oncology, Regional Cancer Center, Trivandrum, India.
4 Resident, Department of surgical Oncology, Regional Cancer Center, Trivandrum, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sivaraman Ganesan, Assistant Professor, Department of Ear, Nose and Throat, JIPMER, Pondicherry-605006, India.
Phone: 9442355292,
E-mail: gsivram@gmail.com
Localized osteoradionecrosis of bony external auditory canal has been described as a late complication of external beam radiotherapy which is delivered to parotid bed after surgical resection of parotid malignancies. Diffuse osteoradionecrosis of temporal bone is rarely seen in such a setting and it is usually caused by resection of part of the bone for surgical clearance, followed by post-operative radiotherapy.This condition warrants aggressive treatment, in order to avoid potentially life threatening intracranial complications. In this report, we are presenting an uncommon case of extensive osteoradionecrosis which involved the entire temporal bone, in a patient who was treated for mucoepidermoid carcinoma of parotid twelve years ago, with total conservative parotidectomy and adjuvant radiotherapy.
Temporal bone, Osteoradionecrosis, Parotid tumours
Case Report
A 66-year-old lady, a known diabetic and hypertensive, presented to our head and neck Surgical Oncology Out-Patients Department with complaints of a painless mass in the right ear canal, present since the past 2 years, intermittent right ear discharge since the past 1 year and discharge from behind the ear since the past 3 months. The discharge was foul smelling and occasionally blood stained. She had been taking local treatment in the form of ear drops on and off for her symptoms, but the complaint persisted.
The patient gave a past history of undergoing Total Conservative Parotidectomy for mucoepidermoid carcinoma of right parotid (T2N0) in April 2000, followed by adjuvant radiation (external beam radiotherapyof 55Gy) given to parotid bed, which was completed in August 2000. She also gave a history of a hemimandibulectomy which was done in April 2004 for osteoradionecrosis of right mandible, which was refractory to conservative measures.
On examination, she was found to be afebrile and her sensorium was normal. Local examination revealed a fleshy mass and a purulent foul smelling discharge filling the right external auditory canal and sprouting granulation in the retro aural region [Table/Fig-1,2]. There was lower motor neuron facial palsy on right side (House-Brackman grade III), which had persisted since the time of parotidectomy. Considering the refractory nature of the condition, a biopsy was done to rule out a malignancy which arose from the temporal bone, but reports showed only granulation tissue. A clinical diagnosis of osteoradionecrosis of right temporal bone which was secondary to previous radiation which was given was made at this point and a High Resolution Computed Tomography (HRCT) scan was done to confirm the diagnosis, assess the extent of bony destruction and to rule out intracranial complications.
Clinical picture of the patient with Fleshy mass in right external auditory canal

Clinical picture showing Fistula in the retro aural region

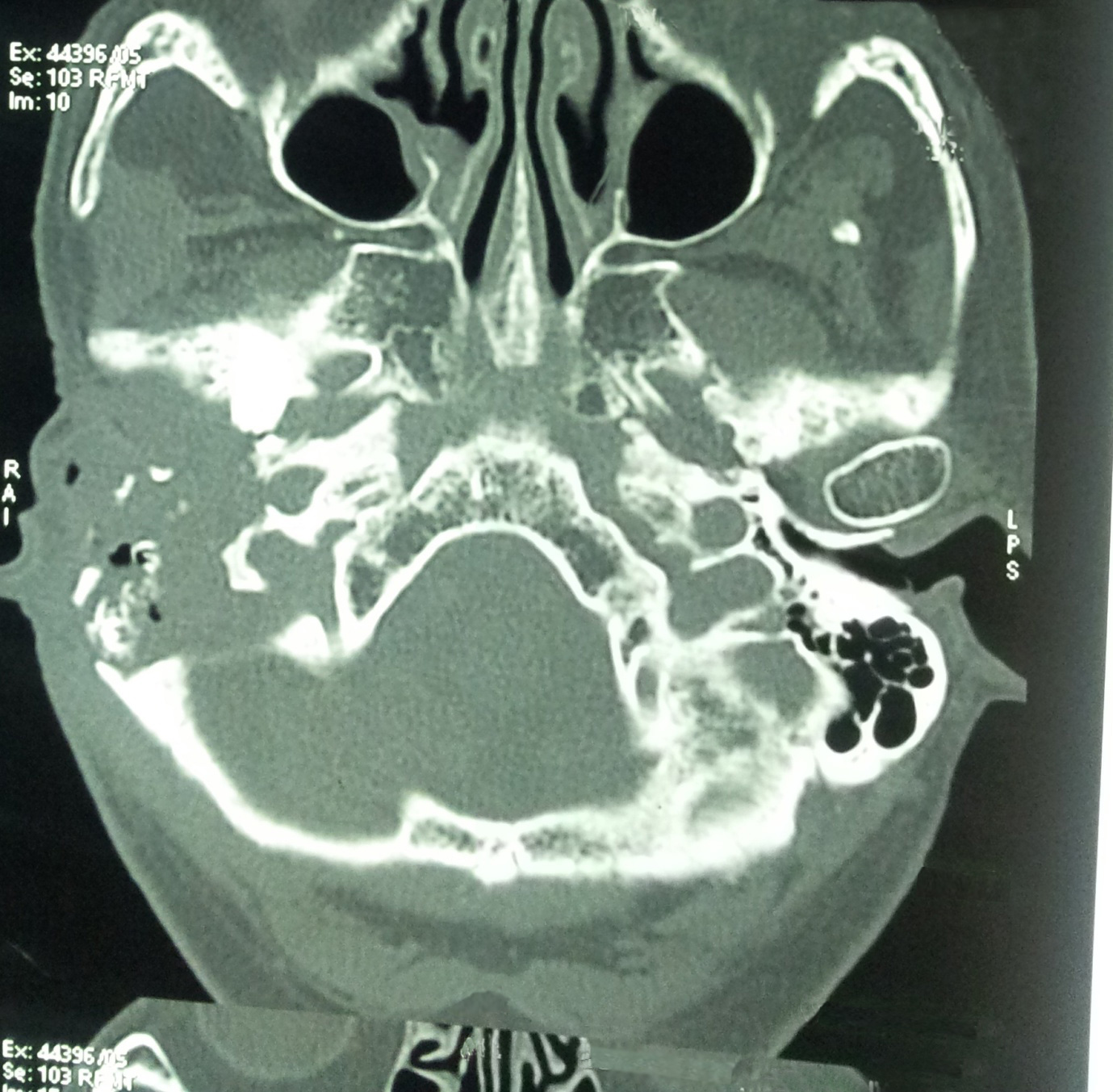
HRCT scan of the temporal bone which was done, showed a non homogenous mass lesion which eroded external auditory canal, middle ear contents, mastoid bone, tegmen tympani, sinus plate, petrous part, cochlea, vestibule, semi-circular canals and the bony facial canal. There was no evidence of any intracranial extension of the lesion.This confirmed the diagnosis of diffuse osteoradionecrosis of the temporal bone from mastoid to petrous tip and which involved the external, middle and inner ear [Table/Fig-3].
HRCT scan of the temporal bone showing non homogenous mass lesion eroding external auditory canal, middle ear contents, mastoid bone, tegmen tympani, sinus plate,petrous part,cochlea,vestibule, semi-circular canals and the bony facial canal
Our plan of aggressively treating the condition by removing all necrotic bony material was explained to the patient, but she was not willing to undergo any surgery. After explaining the possibility of complications which could occur due to administration of inadequate treatment, she was managed conservatively with local debridement, chemical cauterization of granulation tissue and antibiotic ear drops, depending on culture/sensitivity. She has been kept on close follow up, from the time when she presented to us initially in 2006, with frequent ear toileting and is symptomatically better now.
Discussion
Malignant tumours of the salivary glands are relatively rare and they constitute 5 to 7% of head and neck cancers [1]. Although a majority of salivary gland neoplasms arise in the parotid gland, only a small proportion turns out to be malignant. The primary treatment for malignant neoplasms which occur in parotid gland continues to be surgery. Radiotherapy given to the parotid bed is used as an adjuvant treatment for cases with adverse risk factors, such as intermediate or high grade tumours, close or positive margins, perineural invasion and lymphovascular invasion [2]. This has been found to improve loco regional control. Proximity of the temporal bone to the treatment site accounts for the otologic complications of radiotherapy which are associated with the treatment of parotid carcinoma.
The temporal bone becomes susceptible to radiation injury, as it is relatively superficial, receives scanty blood supply, has minimal soft-tissue cover and is constantly exposed to respiratory tract pathogens via Eustachian tube [3]. Hypoxia, hypovascularity and hypocellularity, which are associated with radiation therapy, lead to tissue breakdown, impaired reparative mechanisms and eventually, radionecrosis. Osteoradionecrosis occurs when the irradiated bone becomes devitalized. External auditory canal contains a variety of bacterial and fungal inhabitants and this can also predispose to chronic infections. By definition, it is bone which is exposed through an opening in the overlying skin or mucosa, which persists as a non-healing wound for three months or more [4].
Ramsden et al., provided a classification for osteoradionecrosis of the temporal bone; local and diffuse types [5]. The local type is confined to the external auditory canal, whereas the diffuse type is wide spread and it can involve the skull base and adjacent structures.The rarer diffuse type is usually seen in patients who have received higher doses of external irradiation to the temporal bone. The incidence of temporal bone osteoradionecrosis is also higher when amastoidectomy or temporal bone resection is done for surgical clearance, followed by post-operative radiotherapy [6]. Diffuse type is associated with various complications such as suppurative labyrinthitis, meningitis, cerebrospinal fluid leakage, and internal carotid aneurysms [7].
Our patient had undergone only a total conservative parotidectomy without any resection of temporal bone. Still, she developed osteoradionecrosis of the entire temporal bone.The fact that she developed refractory osteoradionecrosis of mandible quite early in the follow up period, probably points to her increased susceptibility to such a condition.The patient did not have any prior otological complaint and she did not give history of any self inflicted trauma to the external auditory canal.
The management of osteoradionecrosis in the temporal bone remains controversial and it is not supported by prospective, randomized, controlled studies. Marx’s classification system, based on response to therapy, which was proposed in 1983, is the system which is most widely used for the treatment of osteoradionecrosis [4]. Later, Kagan and Schwartz described a staging system which was based on clinical and radiologic findings [8]. Studies have shown that patients with advanced disease do not benefit from hyperbaric oxygen therapy [9]. Surgical management of osteoradionecrosis sometimes ends up in failure, because of the difficulty which is faced in accurately assessing the viability of non-necrotic bone [6].
Leonetti et al., reported that patients with parotid malignancies who underwent over sew of the external auditory meatus, subtotal petrosectomy, and temporal bone defect obliteration, did not develop temporal bone osteoradionecrosis [6]. Highly precise conformal therapies help in delivering adequate doses to diseased sites and minimized doses to normal tissues, thus reducing the incidence of such complications [10–12]. The ideal management in our case was surgical debridement, but we had to resort to conservative measures, as our patient did not give her consent for surgery.
Conclusion
Radiotherapy, along with surgery, has been found to increase the loco-regional control in parotid malignancies, but it can give rise to troublesome complications like osteoradionecrosis of temporal bone. A high index of suspicion is required in such cases, because the symptoms and signs can mimic benign condition like chronic otitis media on one extreme, as well as grave conditions like malignancies on the other.
[1]. Pisani P, Bray F, Parkin DM, Estimates of the world-wide prevalence of cancer for 25 sites in the adult populationInt J Cancer 2002 97:72-81. [Google Scholar]
[2]. http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf [Google Scholar]
[3]. Kveton JF, Surgical management of osteoradionecrosis of the temporalboneOtolaryngol Head Neck Surg 1988 98:231-4. [Google Scholar]
[4]. Marx RE, A new concept in the treatment of osteoradionecrosisJ Oral Maxillo fac Surg 1983 41:351-7. [Google Scholar]
[5]. Ramsden RT, Bulman CR, Lorigan BP, Osteoradionecrosis of the temporal boneJ Laryngol Otol 1975 89:941-55. [Google Scholar]
[6]. Leonetti JP, Marzo SJ, Zender CA, Porter RG, Melian E, Temporal bone osteoradionecrosis after surgery andradiotherapy for malignant parotid tumorsOtol Neurotol 2010 31:656-9. [Google Scholar]
[7]. John DG, Porter MJ, van Hasselt CA, Beware bleeding from the earJ Laryngol Otol 1993 107:137-9. [Google Scholar]
[8]. Schwartz HC, Kagan AR, Osteoradionecrosis of the mandible: scientific basis for clinical stagingAm J Clin Oncol 2002 25:168-71. [Google Scholar]
[9]. Gal TJ, Yueh B, Futran ND, Influence of prior hyperbaric oxygen therapy in complications following microvascular reconstruction for advanced osteoradionecrosisArch Otolaryngol Head Neck Surg 2003 129:72-6. [Google Scholar]
[10]. Garden AS, El-Naggar AK, Morrison WH, Post-operative radiotherapy for malignant tumors of the parotid glandInt J Radiat Oncol Biol Phys 1997 37:79-85. [Google Scholar]
[11]. Nath SK, Simpson DR, Rose BS, Sandhu AP, Recent advances in image-guided radiotherapy for head and neck carcinomaJ Oncol 2009 2009:752135 [Google Scholar]
[12]. Rao Kumuda Arvind, Shetty Shishir Ram, Babu Subhas G, Castelino Renita Lorina, Osteoradionecrosis of the Mandible and Mastoiditis after Radiotherapy for Parotid MucoepidermoidCarcinomaClinical Medicine and Research 2012 10(2):78-82. [Google Scholar]