Body Stalk Anomaly Complicated by Ectopia Cordis in the First Trimester
Shibata Y.1, Terada K.2, Igarashi M.3, Suzuki S.4
1 Lecturer, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo 124-0012, Japan.
2 Lecturer, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo 124-0012, Japan.
3 Resident, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo 124-0012, Japan.
4 Director, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo 124-0012, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shunji Suzuki, Director, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan.
Phone: +81-3-3693-5211, Fax: +81-3-3694-8725,
E-mail: czg83542@mopera.ne.jp
The most serious conditions seen in body stalk anomaly may be the cases which are complicated by ectopia cordis, which is characterized by the abnormal location of the heart outside the thorax. We encountered four cases of body stalk anomaly, which were complicated by ectopia cordis, which were diagnosed in the first trimesters of pregnancy. In three of these cases, ultrasound scans revealed foetuses with large anterior abdominal wall defects, with their hearts extending outside their thoracic cavities. Their mothers, along with their husbands opted for termination of their pregnancies. In 1 other case, an ultrasound scan revealed a dead foetus, with gastroschisis. Based on the current cases, we suggest that the diagnosis of ectopia cordis caused by body stalk anomaly can be made during the first trimester of pregnancy.
Body-stalk anomaly, Prenatal diagnosis
Case Report
Case 1
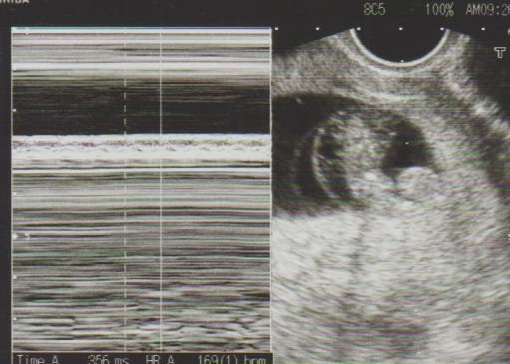
A 30-year-old women, gravida 2, para 1, got pregnant after the use of ovulation-stimulating drugs (human menopausal gonadotropin and human chorionic gonadotropin) and was referred to our hospital for a suspected foetal anomaly at 12 weeks of gestation. A detailed ultrasound scan revealed a foetus with a large anterior abdominal wall defect, nuchal translucency, heart pulsating outside the thorax and a very short umbilical cord [Table/Fig-1]. Estimated diagnoses such as body stalk anomaly and an estimated severe prognosis were discussed with the patient and her husband; they opted for termination of pregnancy [Table/Fig-2]. The foetal karyotype was 46,XY.
A fetus with large abdominal wall defect, nuchal translucency, heart pulsating outside the thorax at 12 weeks of gestation
A fetus after termination showing gastroschisis complicated by ectopia cordis and the attached placenta

Case 2
A 34-year-old-woman, gravida 1, para 0, who conceived by in vitro fertilization and embryo transfer (IVF-ET), was referred to our hospital after a routine dating ultrasound, which revealed a foetus with its heart extending outside the thoracic cavity, gastroschisis and hydrops, at 10 weeks of gestation. [Table/Fig-3]. Estimated diagnoses such as body stalk anomaly and an estimated severe prognosis were discussed with the patient and her husband; they opted for termination of pregnancy.
A fetus with the heart noted to extend outside the thoracic cavity, abdominal wall defect and hydrops at 10 weeks of gestation

Case 3
A 37-year-old-woman, gravida 2, para 0, was referred to our hospital because of an intrauterine foetal demise (IUFD) which had occurred at 14 weeks of gestation. A detailed ultrasound scan revealed a dead foetus with gastroschisis and hydrops [Table/Fig-4]. The postmortem diagnosis of the foetus confirmed body stalk anomaly which was complicated by ectopia cordis [Table/Fig-5].
A dead fetus with gastroschisis and hydrops

A dead fetus showing a body stalk anomaly complicated by ectopia cordis and the attached placenta

Case 4
A 35-year-old-woman, gravida 3, para 0, who conceived by IVF-ET was referred to our hospital after a routine dating ultrasound, which revealed a large subchorionic haemorrhage at 10 weeks of gestation. An ultrasound scan done at our hospital revealed a foetus with gastroschisis, and with its heart pulsating outside the thorax, at 11 weeks of gestation [Table/Fig-6]. Estimated diagnoses such as body stalk anomaly which was complicated by ectopia cordis and an estimated severe prognosis were discussed with the patient and her husband; they opted for termination of pregnancy [Table/Fig-7].
A fetus with gastroschisis, and heart pulsating outside the thorax at 11 weeks of gestation

A fetus after termination showing gastroschisis, ectopia cordis and the attached placenta

Discussion
Body stalk anomaly is a rare, large and severe abdominal wall defect, with evisceration of thoracic and/or abdominal organs [1–4]. The most serious conditions seen in body stalk anomaly may be the cases which are complicated by ectopia cordis [5], which is characterized by the abnormal location of the heart outside the thorax. An early amniotic rupture with subsequent foetal thoracic wall disruption has been supposed to be the most probable cause of this condition [2]. In the current cases, defects in the thoracic and abdominal walls and diaphragm could have led to the lethal displacement of the heart.
The incidences of body stalk anomaly and ectopia cordis have been reported to be 1 in 7,500 and 1 in 15,000 pregnancies in the first trimester, respectively [1–5]. In a review of 11 cases of body stalk anomaly done by Smrcek et al., [4], for example, four cases (36%) were complicated by ectopia cordis. On the other hand, two (50%) of four cases of ectopia cordis were associated with body stalk anomaly, as was seen in a review done by Sepulveda et al., [5]. During this study period, in addition, we encountered only 1 case of ectopia cordis without body stalk anomaly (Cantrell’s pebtalogy was suspected) and two cases of body stalk anomaly without ectopia cordis. Therefore, the incidence of ectopia cordis may not be rare in cases of body stalk anomaly.
Cases of ectopia cordis may be difficult to diagnose if only the apex of the heart is extrathoracic and if visualization is hindered by extruded abdominal content. However, in the current cases, we decided that the diagnosis of ectopia cordis caused by body stalk anomaly could be made, except a case of IUFD which had occurred during the first trimester of pregnancy. Making an early diagnosis of body stalk anomaly which is complicated by ectopia cordis is desirable, considering their poor prognoses.
[1]. Morrow RJ, Whittle MJ, McNay MB, Raine PA, Gibson AA, Crossley J, Prenatal diagnosis and management of anterior abdominal wall defects in the west of ScotlandPrenat Diagn 1993 13(2):111-5. [Google Scholar]
[2]. Daskalakis G, Sebire NJ, Jurkovic D, Snijders RJ, Nicolaides KH, Body stalk anomaly at 10-14 weeks of gestationUltrasound Obstet Gynecol 1997 10(6):416-8. [Google Scholar]
[3]. Tsirka A, Korkontzelos I, Diamantopoulos P, Tsirkas P, Stefos T, Prenatal diagnosis of body stalk anomaly in the first trimester of pregnancyJ Matern Fetal Neonatal Med 2007 20(2):183-4. [Google Scholar]
[4]. Smrcek JM, Germer U, Krokowski M, Berg C, Krapp M, Geipel A, Prenatal ultrasound diagnosis and management of body stalk anomaly: analysis of nine singleton and two multiple pregnanciesUltrasound Obstet Gynecol 2003 21(4):322-8. [Google Scholar]
[5]. Sepulveda W, Wong AE, Simonetti L, Gomez E, Dezerega V, Gutierrez J, Ectopia cordis in a first-trimester sonographic screening program for aneuploidyJ Ultrasound Med 2013 32(5):865-71. [Google Scholar]