Aim: To evaluate and compare the clinical effects of ibuprofen and diclofenac sodium on bleeding during periodontal surgery.
Materials and Methods: Thirteen medically healthy men and women of mean age 37.5±17.67 (mean age± standard deviation) were selected for the study. All the subjects were divided into three groups: control (C) and test groups (T1) and (T2). Each subject of T1 group and T2 group was given ibuprofen and diclofenac sodium respectively, prior to surgery. Bleeding times of patients were recorded prior to performance of periodontal flap surgical procedures.
Results: It was found that there was increased bleeding time and increased peri-operative bleeding when ibuprofen and diclofenac sodium were taken prior to surgery and this was statistically significant. (2.5538 (T1), 1.8385 (T2) versus 1.2385 (C) minute, p= .001) (mean blood loss) and (62.0325 ± 9.0594 (T1), 51.082 ± 9.792 (T2) versus 37.4992 ± 5.99 (C) millilitre, p = .000).
Conclusion: The findings of this study suggested that pre-operative administration of ibuprofen and diclofenac sodium could increase bleeding time and peri - operative blood loss.
Blood loss, Ibuprofen, Diclofenac sodium, Periodontal flap surgery
Introduction
The prevalence of medical conditions such as arthritis and heart disease is steadily increasing in our society. Rheumatoid arthritis (RA) is a chronic, inflammatory disease of the joints. RA is a disabling condition, and it can lead to long-term joint damage which results in persistent pain and loss of function in affected areas. Previously, it was found that patients with RA had a higher incidence of periodontal disease. For some patients, adverse RA symptoms may affect manual dexterity, which can make one’s daily routine quite difficult and affect oral hygiene, which can ultimately lead to periodontal disease [1]. While several studies are presently being done to assess the relationships between heart disease, arthritis and periodontal disease, only little research has been done, which has addressed the interaction of drug treatment. Many patients who suffer from arthritis take some form of analgesic, either aspirin or other non steroidal anti inflammatory drugs [2].
Non steroidal anti inflammatory drugs have become increasingly popular as effective analgesics in management of post - operative pain. Non steroidal anti inflammatory drugs are potent analgesics and anti inflammatory and antipyretic agents. In addition, non steroidal anti inflammatory drugs prolong bleeding time by inhibiting platelet aggregation via cyclo oxygenase pathway [3].
Among the non steroidal anti inflammatory drugs, the most commonly prescribed ones are aspirin, ibuprofen and diclofenac sodium. Aspirin is the most potent analgesic and anti-inflammatory drug. Aspirin irreversibly inhibits thromboxane A2 synthesis and interferes with platelet aggregation, thus prolonging the bleeding time. Aspirin is used to prevent thrombosis in cardiovascular and peripheral vascular diseases. It was suggested that use of even low dose aspirin before an operation could lead to increased pre -operative bleeding. In addition, it was also used in treatment of osteoarthritis and rheumatoid arthritis in doses of 3-5 gm/day. Since large doses of aspirin are poorly tolerated for long periods, non steroidal anti inflammatory drugs like ibuprofen and diclofenac sodium are preferred [4].
Ibuprofen is a phenyl propionic acid derivative and diclofenac sodium is a phenyl aryl acetic acid derivative. Ibuprofen and diclofenac sodium are better tolerated than aspirin. Their side effects are milder and the incidences of these effects are lower as compared to those of the side effects of aspirin. As anti- inflammatory agents, they are mainly used in treatment of musculoskeletal disorders such as rheumatoid arthritis, osteoarthritis and ankylosing spondylitis [4]. The interruption of non steroidal anti inflammatory drug therapy will result in increased pain which is associated with inflammation of joints in patients who suffer from osteoarthritis and rheumatoid arthritis [2]. For these reasons, it is beneficial to determine the effects of non steroidal anti inflammatory drugs on bleeding which occurs during surgery.
However, non steroidal anti inflammatory drug induced cyclo- oxygenase inhibition is reversible and it lasts only as long as drug is in circulation . So these drugs need to be stopped for 1-2 days , depending on their half lives, for the bleeding to return to normal [5,6]. It has been indicated that ibuprofen, at modest dose levels, produces least complication.
A study conducted by Gilder et al., [7] suggested that pre-operative administration of ibuprofen during oral surgical procedures increased intraoperative bleeding. Hence, this study was designed to compare clinical effects of non steroidal anti inflammatory drugs (ibuprofen and diclofenac sodium) on bleeding times and blood losses which occurred during periodontal surgeries.
Materials and Methods
Patient selection
Thirteen patients, five females and eight males with a mean age of 37.5±17.67 (mean age ± standard deviation) years, who attended the Out Patients Department of Periodontics at A.B Shetty Memorial Institute of Dental Sciences, Deralakatte, Mangalore, consented to take part in the study, after being approved by institutional ethical committee. All the patients underwent a baseline clinical examination to determine their eligibilities for the study.
Study Design
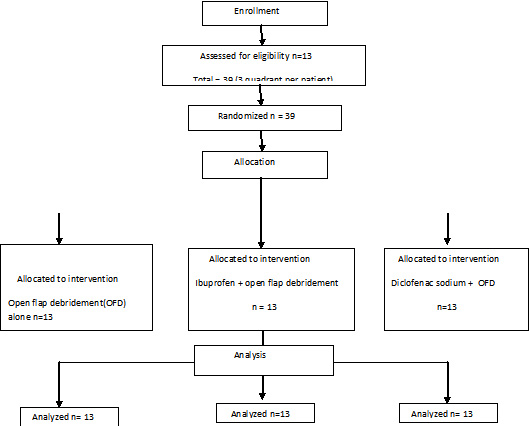
A split mouth design was used. A total of 39 quadrants in 13 patients (three quadrants in each patient) was operated. Complete medical evaluations of all the patients were done to rule out any systemic conditions .
Inclusion criteria included patients with chronic generalized periodontitis with pocket depths which were ≥ 6 mm, with radiographic evidence of bone loss in atleast six teeth in each quadrant (atleast 3 quadrant), with three sites, who required same type and complexity of periodontal surgery and with ability to schedule each surgery on separate visits but at the same time of the day (allotted time to perform surgery was 90 ±15 minutes)[2]. Exclusion criteria included medically compromised patients, those with a history of taking antibiotic therapy since past 6 months, those with a history of any drug allergy, pregnant and lactating mothers, smokers and alcoholics, women undergoing menstrual cycles, postmenopausal women and those with a history of taking anticoagulant therapy.
Treatment procedure
Thirteen patients who met the inclusion / exclusion criteria were randomized into 3 groups.
3 quadrants were selected for modified flap operation (Kirkland) under local anaesthesia, with each quadrant being control C(13) , test group T1(13) and test group T2(13) .
Control group C – where no drug was given prior to surgery
Test group T1 – where patients were given ibuprofen prior to surgery
Test group T2 – where patients were given diclofenac sodium prior to surgery
Each subject received a package which contained an informed consent form, three 400 mg ibuprofen tablets, and instructions to take one tablet 9, 5 and 1 hour/s prior to first surgery and two 100 mg diclofenac sodium tablets , and instruction to take one tablet 6 and 1 hr/s prior to the second surgery. This dose regimen was selected to achieve a peak plasma concentration and maximum drug activity during the surgical procedure. Prior to surgery, the bleeding time was recorded for each patient. Each subject received 4 ml of 2% lignocaine with 1:80,000 epinephrine in the form of block or infiltration.
Bleeding time test
The bleeding time test was conducted by using capillary tube method.
Collection of blood during surgery
Estimation of blood loss consisted of
(1) The volume of water which was used for irrigation during the surgery (a) and that which remained after the surgery (b) were noted. During the surgery, all the blood and water were collected in a graduated beaker by using a portable aspirator.
The volumes of water which was left in the bottle and the beaker were recorded at 15 minutes intervals during the procedure. The length of time taken for performance of the procedure was recorded.Volume of irrigation fluid which was used = b-a = ____millilitre(ml)
(2) The weight of blood soaked gauze was measured
Weight of dry gauze= c
Weight of wet gauze=d
d-c= milligram(mg)
Volume X specific gravity of blood = Weight in mg
____ml X 1.056= ____mg
Any saliva which was generated during procedure was considered to be negligible, since patient served as his/her own control and as all the surgeries were performed at same time of the day, to minimize the changes in rates of salivary flow caused by Circadian rhythm. Each of the scheduled surgeries which were performed on the same subject were matched for their complexities and durations.
Statistical Analysis
Statistical analysis was done by using SPSS, 15.0 software package. Repeated measure Analysis of Variance (ANOVA) was used to determine the mean blood losses and mean bleeding times between control and ibuprofen groups, control and diclofenac sodium groups and between ibuprofen and diclofenac sodium groups. If any significance was observed, Bonferroni’s multiple comparison test was used to compare the mean blood losses and mean bleeding times in all the 3 groups. The level of statistical significance was set at 5%.
Results
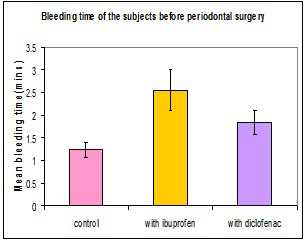
Mean bleeding time was found to be statistically significant between all the three groups (p < .001 ) [Table/Fig-1]. The mean bleeding times for ibuprofen group, diclofenac sodium group and control group were 2.5538±.17097, 1.8385±.44463 and 1.2385±.25998 minutes respectively.
Mean bleeding time and blood loss of control, ibuprofen and diclofenac sodium group and comparisons between two groups
| Treatment group | Multiple BONFERRONI Pairwise comparison |
|---|
| C | I | D | C vs I | C vs D | I vs D |
|---|
| (mean ± SD) | (mean ± SD) | (mean ± SD) | | | |
| Mean bleeding time (in min) | 1.239 ±0.17 | 2.5538 ±0.44 | 1.8385 ±0.25 | (-1.321)*** | (-0.6)*** | (-0.715)*** |
| Mean blood loss (mean ± SD) in ml | 62.03 ± 9.06 | 51.082 ± 9.79 | 37.499± 5.99 | (24.53) *** | (13.58)** | (10.95)* |
C –control group, I – ibuprofen group, D –diclofenac sodium group p<0.001 - ***, p<0.01- **, p<0.05-*
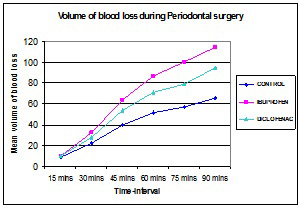
The mean blood losses for 13 patients throughout periodontal surgeries done for ibuprofen, diclofenac sodium and control groups were 62.0325 ± 9.0594, 51.082 ± 9.792 and 37.4992 ± 5.99 ml respectively [Table/Fig-1].The increased blood loss was statistically highly significant for ibuprofen group.
Mean blood losses which occurred during surgeries in all the 3 groups at 15 mins were not statistically significant, while they were statistically significant after 30, 45, 60 and 90 mins between control and ibuprofen groups and between control and diclofenac sodium groups [Table/Fig-2]. At 75 min, blood losses were statistically significant among all the three groups.
Comparison of mean blood loss between 3 groups at various time intervals
| Mean blood loss(in ml) | Multiple BONFERRONI Pairwise comparison |
|---|
| Time interval (in min) | C | I | D | C vs I | C vs D | I vs D |
|---|
| 15 | 9.23 ± 1.88 | 10.08 ± 1.61 | 10 ± 1.41 | ns | ns | ns |
| 30 | 22.54 ± 4.08 | 32.77 ± 7.362 | 28.23 ± 6.772 | 10.23** | 5.692* | 4.538 |
| 45 | 39.92 ± 6.54 | 64 ±15.7 | 54.08 ±12.95 | 24.077** | 14.154** | 9.923 |
| 60 | 51.38 ± 5.98 | 87.15 ± 12.5 | 71.31 ± 12.51 | 35.77*** | 19.92*** | 15.846* |
| 75 | 57.364 ± 7.4 | 100.55 ± 14.9 | 79.27 ± 14.2 | 43.182*** | 21.909** | 21.2738* |
| 90 | 65.667 ± 2.28 | 114.17 ± 12.4 | 94.50 ± 8.83 | 48.5** | 28.833* | 19.667 |
ns- not significant
Blood lost during surgery in all the three groups increased from start of the sugery to 60 mins. These groups consistently experienced increased bleeding throughout surgery, but blood lost during surgery for the subjects who took ibuprofen and diclofenac sodium was statistically significant than that which was seen in control group [Table/Fig-3].
Flowchart of study design
Discussion
Among the non steroidal anti inflammatory drugs that are more effective, choices of ibuprofen and diclofenac were made, based on their efficacies. The mechanisms of diclofenac and ibuprofen are similar and both are reversible COX inhibitors [5,8]. We observed the effects of ibuprofen and diclofenac on bleeding time. Bleeding time indicated anti platelet activities of diclofenac and ibuprofen. This suggested that both ibuprofen and diclofenac caused a reversible block and that they only altered bleeding time during the time of action of the drug .[9] In this study, both the test groups showed significantly prolonged bleeding times [Table/Fig-4]. Both non steroidal anti inflammatory drugs produced modest, but statistically significant prolongations of bleeding times. This was consisitent with findings of study done by Kenneth et al., where they observed the effects of non steroidal anti inflammatory drugs on haemostasis. The magnitude of change in bleeding time which was seen, was similar to change in bleeding time which had been reported previously for patients who were given ibuprofen and diclofenac [6,10–12]. Many factors can affect bleeding which occurs during surgery, such as general health of the patient, time of the day, surgery which was performed, gender, hormones, type, duration, and anatomical location of the surgery. All the three surgeries which were performed on each subject were of the same type, complexity and duration. Furthermore, the surgeries were carried out at the same time of the day and by the same operator [3]. Our data demonstrated that ibuprofen and diclofenac caused significant increases in blood loss which occurred during periodontal surgery. This finding was consistent with those which were observed during abdominal and prostectomy surgeries which were performed with pre-operative administration of ibuprofen [13,14]. This study involved recording of blood loss at 15 minute intervals during each surgical procedure. This pattern was similar for all the three groups. At 15 minutes, blood loss was not statistically significant, but beyond 15 minutes, statistically significant differences were seen between control and ibuprofen groups, and between control and diclofenac groups. At 75 minutes, there were statistically significant differences between all the three groups [Table/Fig-5]. The mean total blood loss for 13 patients throughout periodontal surgeries were highly significant in the ibuprofen group. Although total blood loss was never more than 128 ml, it being within normal limits, increased perioperative bleeding was noted in ibuprofen and diclofenac groups [3,15]. Any bleeding which was associated with incisions and post surgical bleeding were controlled. In this study, we tested whether preoperative bleeding time could predict as to which patient would have increased perioperative bleeding. We found a correlation between prolonged bleeding time and perioperative blood loss. Similarly, Lawrence et al., observed that intraoperative bleeding complications occurred only in those patients who received non steroidal anti inflammatory drugs and who had prolonged bleeding times [16]. It was suggested that patients with normal bleeding times could continue with non steroidal anti inflammatory drug therapy before their surgeries, without the anticipation of prolonged bleeding [3,17]. In this study, although a statistically significant increase in bleeding time which was within normal limits was seen, a nearly two fold increase in blood loss was seen in ibuprofen group. So, it was suggested that preoperative measurement of bleeding time was helpful, since elevated bleeding time was associated with increased operative blood loss [16–19]. Further studies are required to document an increased risk of bleeding in patients with prolonged bleeding times. The present study included medically healthy individuals; thus, these findings cannot be generalized to unhealthy patients. Based on findings of previous studies, we formulated some clinical guidelines to deal with patients who were on non steroidal anti inflammatory drugs before they underwent periodontal surgeries. Inhibition of COX activity by non steroidal anti inflammatory drugs is reversible and it lasts as long the drug is in circulation. So these drugs need to be stopped 1 or 2 days prior to performance of the surgeries, depending on the half lives of drugs, for the bleeding times to return to normal [20]. For patients who require periodontal surgeries ibuprofen and diclofenac sodium should be temporarily discontinued two days before performance of surgeries [21,22]. However, further studies need to be done on larger populations and on medically compromised patients, to provide a rational basis for preoperative timings of non steroidal anti inflammatory drug withdrawals, with particular emphasis on a careful analysis of perioperative bleeding complications. The summary of the present study is that there was a strong association between prolonged bleeding time and perioperative blood loss and that there may be a strong association between prolonged bleeding time and peri – operative blood loss.
Comparison of bleeding time in the three groups before periodontal surgery
Comparison of volume of blood loss during periodontal surgery at various time intervals in the three groups
C –control group, I – ibuprofen group, D –diclofenac sodium group p<0.001 - ***, p<0.01- **, p<0.05-*
ns- not significant
[1]. Pischon N, Pischon T, Kroger J, Gulmez E, Kleber BM, Bernimoulin JP, Association Among Rheumatoid Arthritis, Oral Hygiene, and PeriodontitisJ Periodontol 2008 79(6):979-86. [Google Scholar]
[2]. Braganza A, Bissada N, Hatch C, The effect of non steroidal anti inflammatory drug on bleeding during periodontal surgeryJ Periodontol 2005 76:1154-60. [Google Scholar]
[3]. Romsing J, Larsen SW, Peri - operative use of non steroidal anti inflammatory drugs in children: Analgesic efficacy and bleedingAnaesthesia 1995 52:673-83. [Google Scholar]
[4]. Gilman AG, Rall TW, Nies AS, The Pharmacological Basis of Therapeutics 2001 10th EdMc Graw Hill [Google Scholar]
[5]. McIntyre BA, Philip RB, Inwood MJ, Effect of ibuprofen on platelet function in normal subjects and hemophiliac patientsClin Pharmacol Therap 1978 245:616-21. [Google Scholar]
[6]. Vogel RI, Desjardins PJ, Major KV, Comparison of presurgical and immediate postsurgical ibuprofen on postoperative periodontal painJ Periodontol 1992 63(11):914-8. [Google Scholar]
[7]. Gilder L, Wideman Keffer M, Analgesic efficacy of a combination of hydrocodone with ibuprofen in post operative painClin Pharmacol Therap 1999 65:66-76. [Google Scholar]
[8]. Amrein PC, Ellman L, Harris WH, Aspirin induced prolongation of bleeding time and peri-operative blood lossJAMA 1981 245(18):1825-8. [Google Scholar]
[9]. Nielsen JC, Pjerring P, Arendt-Nielsen L, Petterson KJ, A double-blind, placebo controlled, cross-over comparison of the analgesic effect of ibuprofen 400 mg and 800 mg on laser-induced painBr J Clin Pharmacol 1990 30(5):711-5. [Google Scholar]
[10]. Bowen B, Yuan Y, James C, Rashid F, Short-Term Use of High-Dose Ibuprofen Linked to GI BleedingClin Gastroenterol Hepatol 2005 3:1-5. [Google Scholar]
[11]. Kokki H, Hendolin H, Ibuprofen in the treatment of post operative pain in small children : A randomized double blind placebo controlled parallel group studyActa Anaesthesiol Scand 1994 38:467-72. [Google Scholar]
[12]. Slappendel R, Weber EW, Durieux ME, Does ibuprofen increase perioperative blood loss during hip arthroplasty?Eur J Anaesthesiol 2002 19:829-31. [Google Scholar]
[13]. Goldenberg NA, Jacobson L, Brief communication: Duration of platelet dysfunction after a 7-day course of ibuprofenAnn Int Med 2005 142(7):506-9. [Google Scholar]
[14]. Tripathi KD, Essentials of Medical Pharmacology 2003 5th editionJaypee Brothers Medical Publisher [Google Scholar]
[15]. Cooper SA, Needle SE, Kruger GO, Comparative analgesic potency of aspirin and ibuprofenJ Oral Surg 1977 35(11):898-903. [Google Scholar]
[16]. Breivik EK, Barkvoll P, Skovlund E, Combining Diclofenac with acetaminophen or acetaminophen- codeine after oral surgery: A randomized, double blind single- dose studyClin Pharmacol Therap 1999 66(6):625-35. [Google Scholar]
[17]. Ardekian L, Gasper R, Peled M, Does low dose aspirin therapy complicate oral surgical procedures?JAMA 2000 131:331-5. [Google Scholar]
[18]. Irwin MG, Roulson CJ, Jones RD, Cheng IK, Visram AR, Peri-operative administration of rectal diclofenac sodium. The effect on renal function in patients undergoing minor orthopaedic surgeryEur J Anaesthesiol 1995 12(4):403-6. [Google Scholar]
[19]. Thiagarajan J, Bates S, Hitchcock M, Blood loss following tonsillectomy in childrenAnaethesia 1994 47:132-5. [Google Scholar]
[20]. Lawrence C, Sakuntabhai A, Grosse TS, Effect of aspirin and non steroidal anti inflammatory drug on bleeding complications in dermatologic surgical patientsJ Am Acad Dermatol 1994 31:988-92. [Google Scholar]
[21]. Campbell WI, Kendrick R, Patterson C, Intravenous Diclofenac sodium :Does its administration before operation suppress postoperative pain ?Anaesthesia 1990 45:763-6. [Google Scholar]
[22]. Robinson PM, Ahmed I, Diclofenac and post tonsillectomy haemorrhageClin Otolaryngol 1994 19:344-5. [Google Scholar]